This article is an answer to the Case – High Fever and Cough with Rusty, Blood-Streaked Sputum
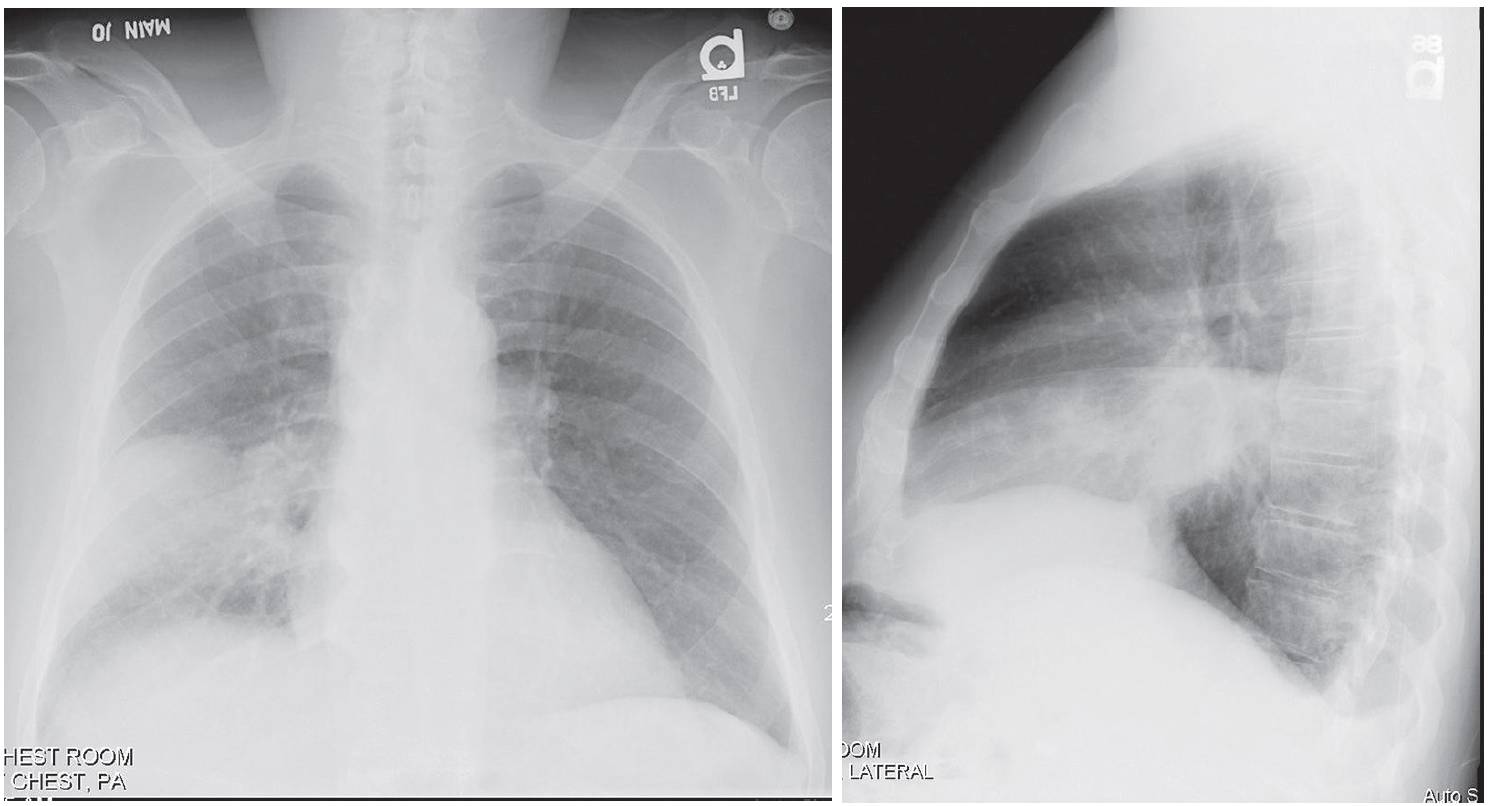
Radiologic Findings
PA and lateral chest X-rays reveal dense, non-segmental homogeneous lobar consolidation that partially silhouettes the right heart border and is bordered by the horizontal and oblique fissure. No associated volume loss. A small ipsilateral pleural effusion blunts the posterior sulcus.
Diagnosis
Pneumococcal Pneumonia; Right Middle Lobe
Differential Diagnosis
Other Community-Acquired Pneumonias
Discussion
Background
Most pneumococcal infections occur in the winter and early spring. The organism is acquired through person- to-person transmission by inhalation of aerosolized droplets, physical contact, or both. Risk factors for infection include very young or advanced age, chronic heart and/or lung disease, alcoholism and/or cirrhosis, ections and Aspiration Pneumonia sickle cell anemia, lymphoma, leukemia, multiple myeloma, HIV-AIDS, intravenous drug abuse (IVDA), and prior splenectomy.
Etiology of Pneumococcal pneumonia
Pneumococcal pneumonia is caused by the Gram-positive, diplococcal bacterium Streptococcus pneumoniae. This bacterium is responsible for at least half of all cases of community-acquired pneumonia and is also the most common cause of community-acquired pneumonia resulting in hospital admission. Pneumococci colonize the upper respiratory tract of 5–60% of the general population.
Clinical Findings in Pneumococcal pneumonia
Pneumococcal pneumonia is the most common bacterial pneumonia to follow influenza pneumonia infection. Additionally, up to 70% of patients with pneumococcal pneumonia have had a recent upper respiratory tract infection (URI).
Affected patients often have an abrupt onset of rigors, followed by fever, cough productive of rusty sputum, and dyspnea. Pleuritic chest pain is common, experienced in up to 75% of patients. Leukocytosis is usually present (WBC 15,000–25,000), but severe infection may be associated with white blood cell counts of less than 3,000/mm3.
Complications of Pneumococcal pneumonia
- Metastatic infection (e.g., endocarditis, meningitis, arthritis)
- Pericarditis
- Rarely empyema
- Pneumatoceles; more common in children
Imaging Findings in Pneumococcal pneumonia
Chest Radiography
- Homogeneous, non-segmental, parenchymal consolidation involving one lobe; multi-lobar involvement less common
- Air space disease abuts surrounding visceral pleura of fissural surfaces
- Predilection for lower lobes or posterior segments of upper lobes
- Minimal volume loss
- Air bronchograms common
- Rare cavitation
- Mass-like rounded consolidation (i.e., round pneumonia) infrequent in adults; more common in children
- Pleural effusion common (60%); empyema unusual
MDCT
- Homogeneous, non-segmental, parenchymal consolidation involving one lobe; multi-lobar involvement less common
- Air space disease abuts visceral pleura of fissural surfaces
- Predilection for lower lobes or posterior segments of upper lobes
- Minimal volume loss
- Air bronchograms common
- Rare cavitation; CT more sensitive than conventional radiography
- Pleural effusion common (60%); empyema unusual; CT more sensitive than conventional radiography
- Lymphadenopathy common in hospitalized patients
- Ipsilateral to pneumonia in most affected patients
- Bronchopneumonia pattern characterized by peribronchial and peribronchiolar consolidation affecting one or more lobes
- Air space nodules 4–10 mm in diameter
- Opacification of entire secondary pulmonary lobule
Management of Pneumococcal pneumonia
- Penicillin is antibiotic of choice
- Vancomycin is antibiotic of choice for penicillin-resistant strains (30% of isolates)
- Pneumococcal polysaccharide vaccine encouraged for high-risk patient populations
Prognosis
- Onset of recovery within 24–48 hours of antibiotic therapy; resolution after two weeks
- Slow clearance in elderly, those requiring hospitalization, smokers, and patients with underlying lung disease and bacteremia; 4–8-week disease course in these cases
- Increased mortality in patients >50 years and those with cirrhosis, cardiac and/or chronic pulmonary disease, asplenia, leukopenia (<4,000 cells/mm3), leukocytosis (>20,000 cells/mm3), malignancy, multi-lobar involvement, hypoxemia, bacteremia, and penicillin-resistant disease
Pearls
- Absence of air bronchograms argues against the diagnosis.
- Round pneumonias are more frequently seen in children <8 years of age, but may be seen in adults. Adult infection rapidly progresses to more typical lobar pneumonia. Failure to do so suggests underlying neoplasia.
- Necrotizing pneumonia most often occurs with polymicrobial infections.
- Lymphadenopathy is common on CT in hospitalized patients. Thus, when a patient with pneumococcal pneumonia has lymphadenopathy identified on CT, other etiologies for the lymphadenopathy need not be suspected.