The classic presentation of an acute coronary syndrome (ACS) is that of an older age male smoker with hypertension who reports exertional chest pressure that radiates to the left upper extremity and is associated with shortness of breath. This presentation is well recognized by the emergency provider (EP).
Unfortunately, many patients with ACS lack overt chest pain or pressure and present to the EP with atypical signs and symptoms. As a result, the EP may fail to consider the diagnosis of ACS, leading to increased morbidity and mortality.
Recent literature has demonstrated that patients with atypical ACS presentations are less likely to receive anti-ischemic therapy and more likely to die when compared to patients with the classic ACS presentation.
Currently, more than 20% of ACS patients who present with atypical signs and symptoms are missed upon initial evaluation. In order to prevent unnecessary morbidity and mortality, it is critical for the EP to identify patients with ACS who do not present with textbook symptoms.
Atypical ACS symptoms
Common atypical ACS symptoms include:
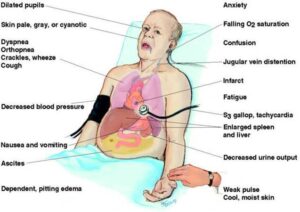
- dyspnea
- diaphoresis
- nausea
- vomiting
- near-syncope
- Jaw pain
- neck pain
- back pain
- extremity pain
- abdominal pain
- fatigue
Due to the absence of chest pain with these symptoms, an electrocardiogram (ECG) and cardiac markers are often delayed or not obtained altogether.
Patients with atypical ACS presentations are more likely to be female or elderly or have a history of diabetes or heart failure.
Women are at particularly high risk for misdiagnosis of ACS. Not only are women more likely to have atypical presentations, they are also more likely to have diabetes and be younger at the time of ACS presentation. In addition, women present later in the time course of their illness when compared to ACS patients who present with the classic symptom of chest pain.
Patients with diabetes have long been recognized to present with atypical features of ACS. This higher rate of atypical ACS presentation is thought to be due to a neuropathy that affects the sensory innervation to the heart.
Finally, patients with atypical ACS presentations are less likely to have a history of smoking, hyperlipidemia, or prior cardiac disease. Importantly, concern for ACS should not solely be limited to female, diabetic, or older patients who present with atypical symptoms. ACS should be considered for any symptom without any obvious cause that could potentially be caused by cardiac ischemia.
Diagnosing Acute Coronary Syndrome (ACS) with Atypical Presentation
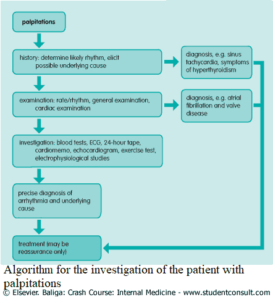
The most important step in making the diagnosis of ACS is to simply consider the diagnosis in patients presenting with the symptoms listed above. Obtain an ECG in any patient that there is clinical concern for ACS. If the ECG is nondiagnostic, consider obtaining cardiac markers and placing patients in observation for additional diagnostic testing.
Furthermore, it is important to administer time-sensitive therapy when the diagnosis of ACS is considered. This may include antiplatelet or anticoagulant medications, along with cardiology consultation.
Key Points
- Patients with atypical ACS presentations are less likely to receive critical, time-dependent therapy and are more likely to die.
- Dyspnea, diaphoresis, vomiting, and fatigue are common atypical signs and symptoms of ACS.
- Atypical presentations of ACS are more likely to occur in women, diabetic patients, and the elderly.
- Patients with atypical ACS presentations are less likely to have existing cardiac disease.
- Obtain an ECG in any patient with signs or symptoms concerning for ACS.
Read Also :