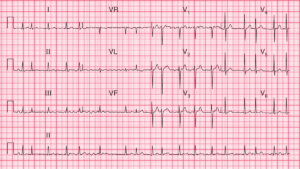
Evaluation of the emergency department patient with a wide-complex tachycardia (WCT) can be a challenge for any emergency provider (EP).
It can be especially difficult to distinguish between ventricular tachycardia (VT) and supraventricular tachycardia (SVT) with aberrant conduction. Fortunately, if the patient is unstable, the initial treatment for both rhythms is synchronized electrical cardioversion.
However, for the stable patient with a wide-complex tachycardia (WCT), misdiagnosis of VT as SVT with aberrant conduction could prove to be a deadly error.
What is wide-complex tachycardia (WCT) ?
A wide-complex tachycardia (WCT) is defined as:
- ventricular rate > 100 beats per minute
- QRS complex duration of more than 0.12 seconds
The primary differential for a WCT is VT and SVT with aberrant conduction.
What Rhythms can Produce SVT with Aberrancy ?
Rhythms that can produce SVT with aberrant conduction include:
- paroxysmal SVT
- atrial fibrillation
- atrial flutter
- sinus tachycardia
- hyperkalemia
Differentiating VT from SVT with Aberrancy
Though it may often seem impossible to differentiate VT from SVT with aberrant conduction, there are a number of electrocardiography (ECG) and historical features that may be used to improve the EP’s ability to differentiate between these two rhythms.
Importantly, there is no single data point from the history, physical examination, or ECG that can reliably distinguish VT from SVT with aberrant conduction.
Factor that increase the likelihood of VT
- Age >50 years
- History of :
- prior myocardial infarction
- ischemic heart disease
- structural heart disease
- VT
Aside from age and components of the past medical history, ECG findings are generally used to help differentiate VT from SVT with aberrant conduction.
ECG findings for Differentiating VT from SVT with Aberrancy
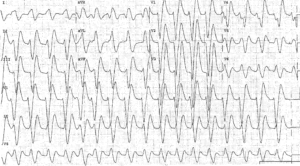
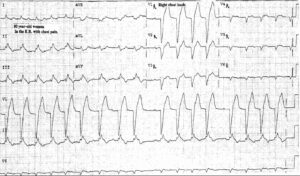
Multiple ECG abnormalities have been proposed to differentiate these rhythms. The regularity of the rhythm can be helpful.
An irregularly irregular rhythm can suggest SVT with aberrant conduction due to atrial fibrillation. In contrast, monomorphic VT is generally a regular rhythm.
Additional findings that suggest VT include:
- QRS concordance in the precordial leads
- atrioventricular (AV) dissociation
- capture beats
- fusion beats
These findings, though poorly sensitive, are highly specific for VT.
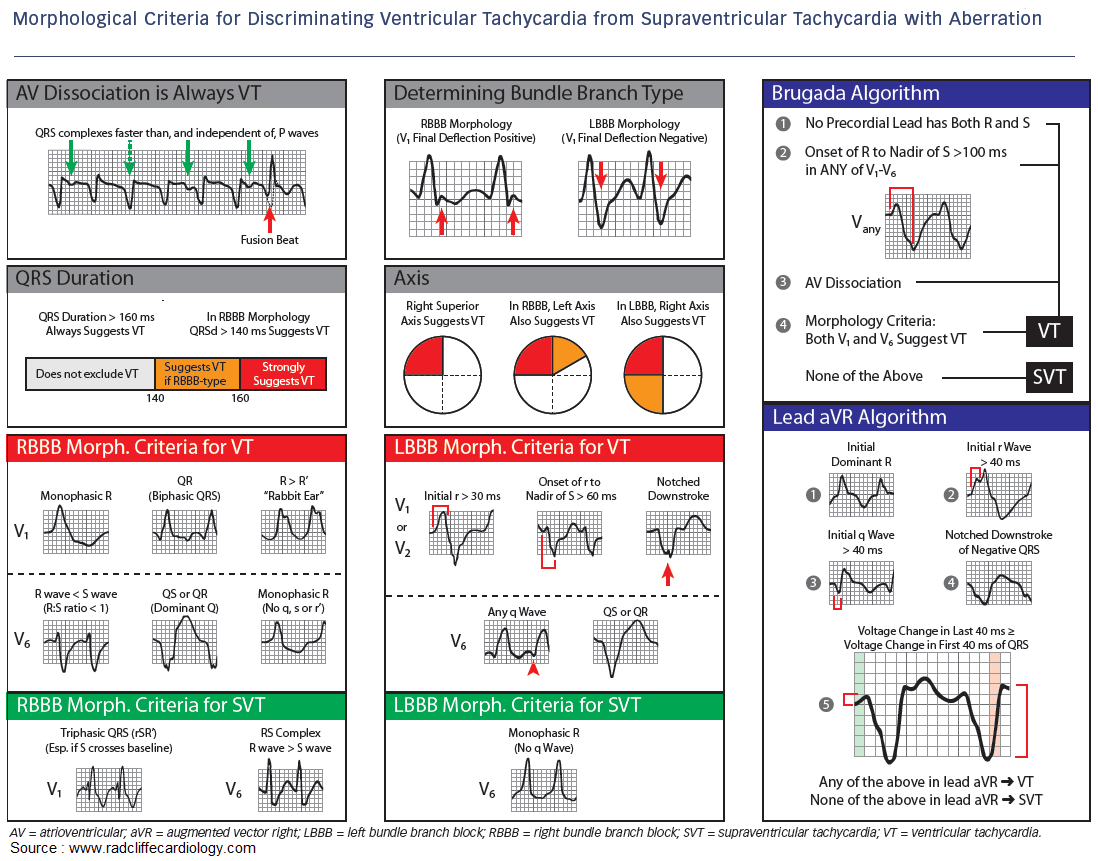
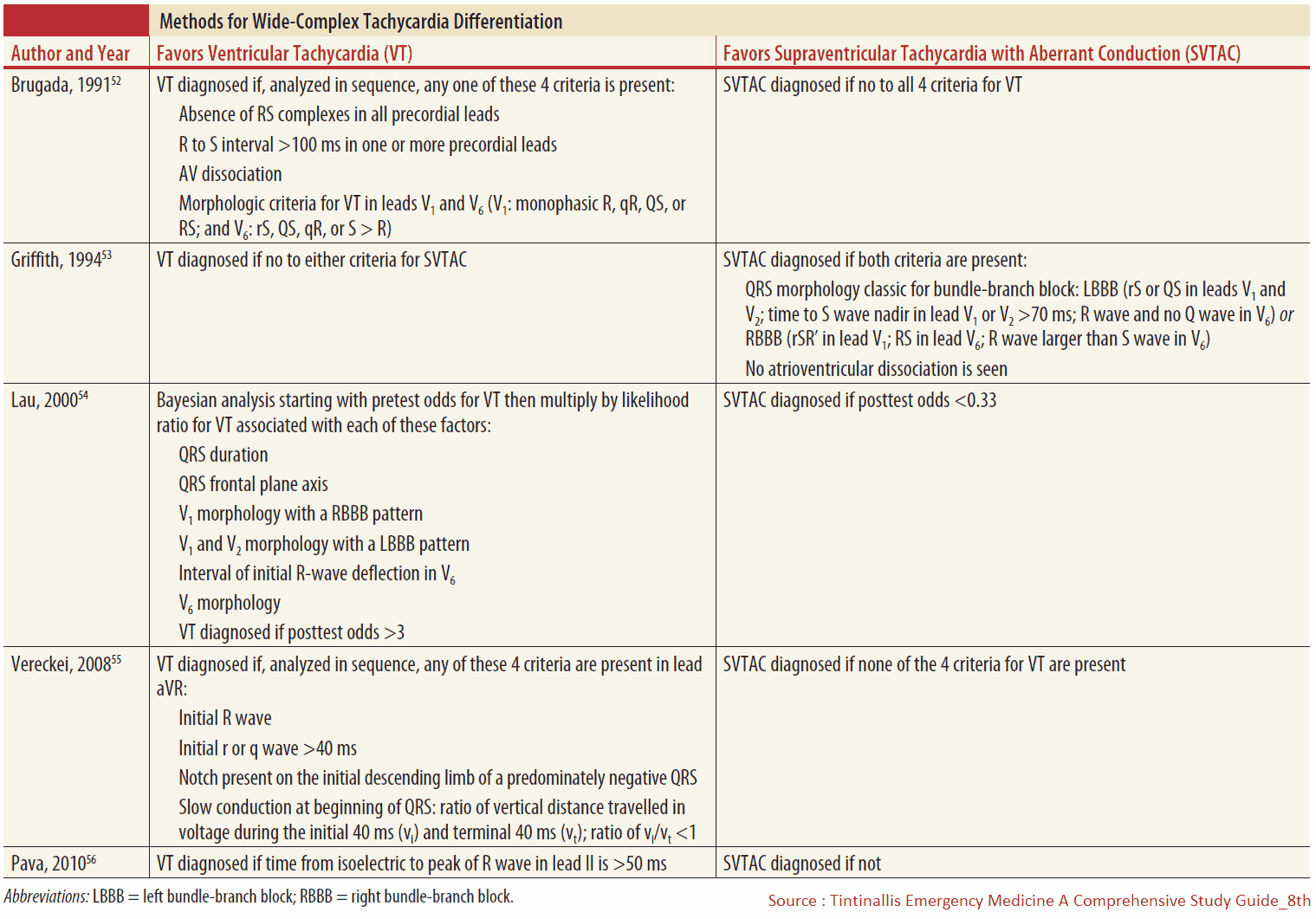
Brugada Algorithm
Brugada and colleagues developed one of the most frequently cited decision rules to distinguish between VT and SVT with aberrant production. In the Brugada algorithm, VT is diagnosed if the ECG demonstrates any of the following four criteria:
- Is there absence of an RS complex in leads V1 through V6?
- Is there an R to S interval >100 ms in one precordial lead?
- Is there AV dissociation?
- Are there morphology criteria for VT?
In practice, the Brugada Criteria can be difficult to recall, and validation studies have shown significantly lower sensitivity and specificity than originally published by Brugada and colleagues. In fact, a recent study showed 22% disagreement among EPs who used the Brugada Criteria in the evaluation of WCT.
Other Algorithms
Additional algorithms have been published, including those by Vereckei and colleagues and by Griffith and colleagues. These algorithms can be easily found online.
In the Griffith algorithm, SVT with aberrant conduction is diagnosed only if the QRS axis and morphology meet criteria for a right bundle-branch block or left bundle-branch block and there is no evidence of AV dissociation. Otherwise, all rhythms are considered VT. Importantly, no ECG criteria or algorithms have been shown to be 100% specific for SVT or VT.
Final words
Hemodynamic stability should also not be used to differentiate VT from SVT with aberrant conduction. Hemodynamic stability is not universally associated with SVT with aberrant conduction and is not indicative of rhythm classification.
In addition, medications used to treat SVT (i.e., adenosine, calcium channel blockers) could cause decompensation if given to a patient with VT. Conversely, medications generally used to treat VT (i.e., procainamide, amiodarone) can be effective in the treatment of a patient with SVT with aberrant conduction.
When there is clinical uncertainty, a regular WCT should be treated as VT until proven otherwise.
READ MORE about : Summary of ECG Interpretation
Key Points
- A regular WCT should be assumed to be VT until proven otherwise.
- There is no single feature of the history, physical examination, or ECG that can reliably distinguish VT from SVT with aberrant
- conduction.
- Age >50 years and a history of prior myocardial infarction, ischemic heart disease, structural heart disease, or VT increases the likelihood of VT.
- There are currently no published ECG algorithms that routinely distinguish VT from SVT with aberrant conduction.
- Hemodynamic stability should not be used to differentiate VT from SVT with aberrant conduction.
Suggested Readings
- deSouza IS, Peterson AC, Marill KA, et al. Differentiating types of wide-complex tachycardia to determine appropriate treatment in the emergency department. Emerg Med Pract. 2015;17:1–22. https://pubmed.ncbi.nlm.nih.gov/26308484/
- Jastrzebski M, Kukla P, Czarnecka D, et al. Comparison of five electrocardiographic methods for differentiation of wide-QRS tachycardias. Europace. 2012;14:1165–1171. https://pubmed.ncbi.nlm.nih.gov/22333239/
- Mattu A, Brady W. Wide Complex Tachycardia. Cardiovascular Emergencies. Dallas, TX: American College of Emergency Physicians, 2014.
- Sousa PA, Pereira S, Candelas R, et al. The value of electrocardiography for differential diagnosis in wide QRS complex tachycardia. Rev Port Cardiol. 2014;33:165–173. https://www.sciencedirect.com/science/article/pii/S2174204914000749
- Szelényi Z, Duray G, Katona G, et al. Comparison of the “real-life” diagnostic value of two recently published electrocardiogram methods for the differential diagnosis of wide QRS complex tachycardias. Acad Emerg Med. 2013;20:1121–1130. https://onlinelibrary.wiley.com/doi/full/10.1111/acem.12247