Table of Contents
Clinical Crearance – Low Risk Patient (NEXUS)
Definitions
Midline posterior bony cervical-spine tenderness is present if the patient reports:
- Pain on palpation of the posterior midline neck from the nuchal ridge to the prominence of the first thoracic vertebra, or if the patient evinces pain with direct palpation of any cervical spinous process
Intoxication: Patients should be considered intoxicated if they have either of the following:
- A recent history provided by the patient or an observer of intoxication or intoxicating ingestion
- Evidence of intoxication on physical examination such as an odor of alcohol, slurred speech, ataxia, dysmetria, or other cerebellar findings
- Any behavior consistent with intoxication
- Patients may also be considered intoxicated if tests of bodily secretions are positive for alcohol or drugs that affect the level of alertness
An altered level of alertness can include any of the following:
- Glasgow Coma Scale score of 14 or less
- Disorientation to person, place, time, or events
- Inability to remember three objects at five minutes
- Delayed or inappropriate response to external stimuli or other findings
A focal neurologic deficit is any focal neurologic finding on motor or sensory examination
Distracting injury: No precise definition of a painful distracting injury is possible
- This category includes any condition thought by the clinician to be producing pain sufficient to distract the patient from a second (neck) injury
- Such injuries may include, but are not limited to, any long-bone fracture; a visceral injury requiring surgical consultation; a large laceration, degloving injury, or crush injury; large burns; or any other injury causing acute functional impairment
- Physicians may also classify any injury as distracting if it is thought to have the potential to impair the patient’s ability to appreciate other injuries
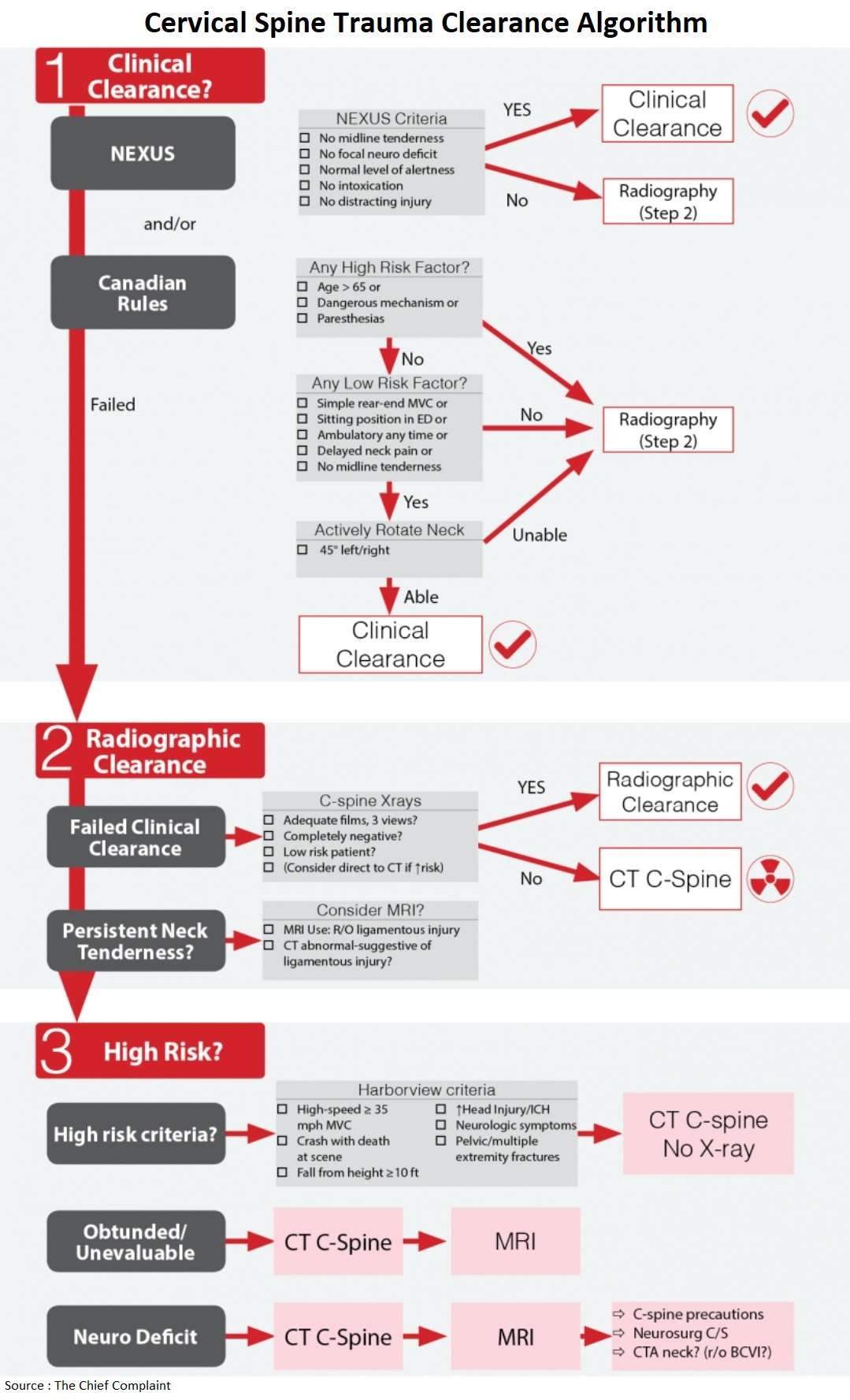
C-Spine Clearance
□ Asymptomatic/↓Risk: → NEXUS +/-CCR
□ Failed NEXUS/CCR → C-spine xrays
□ High risk mechanism: → CT C-spine
□ Unevaluable patient: → CT C-spine
□ Neuro deficit → CT & MRI
Journal Club: NEXUS C-Spine Rules
NEXUS validation study (NEJM 2000;343:94-9)
- Nexus identified all but 8/818 patients with any C-Spine Injury (CSI) and all but 2/578 patients with clinically significant injury (CSI)
- Cervical Spine injury (Sens 99%, NPV 99.8%)
- Clinically significant injury (Sens 99.6%, NPV 99.9%)
CCR vs Nexus study (NEJM 2003;349:2510-8)
- Retrospective study done by developers of Canadian rule
- Sensitivity 90.7% for NEXUS vs 99.4% for CCR
- CCR identified 161 of 162 CSI in patients in whom the range of motion was evaluated
- Nexus missed 1/10 injuries
Do we need each of the 5 criteria? (Ann Emerg Med 2001;38:22-25)
- A substantial number of patients (29%) with clinically significant CSI met only one of the criteria
- Posterior mid-line tenderness was the only criteria present in 61% of these patients
- Distracting injury was sole criterion present in 45/578 of patients with clinically significant CSI
NEXUS vs CT (J Trauma 2007;62:1405)
- Clinical exam (NEXUS) had a sensitivity of only 58% (7/17 injuries missed) when compared to CT C-spine results (gold standard)
Canadian C-Spine Rules (CCR)
For patients with trauma who are alert (GCS = 15), stable and cervical spine injury is a concern, the determination of risk factors guides the use of cervical spine radiography.
A dangerous mechanism is considered to be:
- Fall from an elevation ≥3 ft or 5 stairs
- Axial load to the head (e.g., diving)
- Motor vehicle collision at high speed (>100 km/hr) or with rollover or ejection
- Collision involving a motorized recreational vehicle
- Bicycle collision
A simple rear-end motor vehicle collision excludes being pushed into oncoming traffic, being hit by a bus or a large truck, a rollover, and being hit by a high-speed vehicle.
Journal Club: Canadian C-Spine Rules
CCR validation study (JAMA 2001;286:1841-1848)
- Sensitivity 100%
CCR better than physician judgment? (Ann Emerg Med 2003;42:395)
- Physician judgment had 92% sensitivity for predicting a probability of clinically important fracture
- CCR had 100% sensitivity for predicting a probability of clinically important fracture
CCR vs Nexus study (NEJM 2003;349:2510-8)
- Retrospective study done by developers of Canadian rule
- Sensitivity 90.7% for NEXUS vs 99.4% for CCR
- CCR identified 161 of 162 CSI in patients in whom the range of motion was evaluated
- Nexus missed 1/10 injuries
Radiographic Clearance
Plain X rays
- Use: Low risk patients that fail clinical c-spine clearance
- Negative criteria
- Xrays must be 3 views, adequate, and no abnormality detected to be considered negative
- If not all criteria met → CT
- Journal Club
- Mixed results on utility of plain Xrays
- Flexion/Extension views are not useful/inadequate to evaluate for ligamentous injury (J Orthop Trauma 2011;25:51)
Journal Club: Plain films for C-spine Clearance
NEXUS breakdown (Ann Emerg Med 2001;38:1-7)
- Total misses: Of 818 pts with CSI, Xrays identified 498 patients (Missed 320/818; 39.1%)
- Normal & Adequate: 47 CSI patients xrays were interpreted as normal and adequate (miss rate 47/818; 5.7%)
- Conclusion: “… in many patients with blunt trauma, plain films are not adequate, and adjunctive studies are required before cervical spine injury can be excluded.“
Diaz et al. (J Trauma. 2005;59:897)
- Plain Xray failed to identify 299 of 416 cervical spine injuries (72%)
Meta-analysis (J Trauma. 2005;58:902)
- The pooled sensitivity for cervical spine plain radiography was 52%
EAST Trauma Guidelines (J Trauma 2009;67:651)
- Plain radiographs contribute no additional information and should not be obtained
CT C-spine
- Multiple studies show high sensitivity (100%) if done with lateral reconstructions (to eval alignment)
- Straight to CT? (i.e. no plain films?)
- High risk patient (>1 Nexus criteria, bad mechanism of injury)
- Low likelihood of adequate films: DJD, obese, ALOC
- Harborview Criteria (AJR 2000;174:713)
- Study identified high risk criteria → Patient should go directly to CT (no plain films)
- Patients with > 5% risk of CSI
MRI
Indications:
- Neurologic deficit
- Abnormal CT
- Persistent cervical pain/tenderness
- Obtunded patient, unable to clear C-spine
R/O Ligamentous injury (Ann Emerg Med 2011;58:521)
- MRI obtained for: CT negative + persistent midline tenderness
- 78/178 patients (44%) had acute cervical injury detected on MRI
- 2.8% of these were managed surgically
- Consider MRI for patient that has persistent midline cervical tenderness, even after negative CT
High Risk Patient
High risk criteria
- Harborview Criteria (AJR 2000;174:713)
- Study identified high risk criteria → Patient should go directly to CT (no plain films)
- Patients with > 5% risk of Cervical Spine Injury
- Work-up
- Straight to CT
- Plain Xrays not indicated
High risk criteria: Harborview
□ High-speed ≥ 35 mph MVC
□ Crash with death at scene of motor vehicle accident
□ Fall from height (≥10 ft)
□ Significant closed head injury (or intracranial hemorrhage seen on CT
□ Neurologic symptoms or signs referred to the cervical spine
□ Pelvic or multiple extremity fractures
Altered Mental Status
- Plain Xrays not indicated
- CT C-spine to rule out bony injury
- Consider MRI to rule out ligamentous and cord injury
Neurologic deficit
- Strict C-spine precautions
- Plain Xrays not indicated
- CT C-spine to evaluate for bony injury
- MRI C-spine to evaluate for ligamentous and spinal cord injury
- Neurosurgery consult
- CTA neck?
- Rule out blunt cerebrovascular injury (BCVI)?
C-Spine Algorithm at LAC+USC
• Awake/alert/not intoxicated: NEXUS and/or Canadian C-spine Rules
• Neck tenderness w/low mechanism: plain radiographs/C-spine xrays
• Neck tenderness w/high mechanism: CT C-spine
• Unevaluable patient: CT C-spine
• Evaluable patient w/neurological deficit & normal CT: MRI
Neurogenic Shock
Incidence
- Cervical injury (19%), Thoracic injury (7%)
Definition
- High cord lesion causing decreased sympathetic outflow resulting in hypotension and bradycardia
- Depressed spinal reflexes caudal to spinal cord injury
- Phase 1 (0-1days)
- Areflexia/hyporeflexia
- DPR (delayed plantar response) is first reflex to appear and may be present in the ED
- Phase 2 (1-3 days)
- Initial reflex return
- Return of reflexes: cutaneous return first (Cremaster, BC, anal wink) before DTRs (deep tendon reflexes)
- Phase 3 (4 days-1month)
- Early hyperreflexia
- DTRs (deep tendon reflexes) re-appear early in this phase (AJ → KJ) and DPR (delayed plantar response) will be lost
- Phase 3 (1-12 months)
- Spasticity/hyperreflexia
Treatment
- Rule out Hemorrhage
- Fluid resuscitation (NS or LR)
- Vasopressors (Dopamine vs Norepinepthine vs Phenylephrine) to target MAP (unknown)
References
- Validity of a Set of Clinical Criteria to Rule Out Injury to the Cervical Spine in Patients with Blunt Trauma. https://www.nejm.org/doi/full/10.1056/nejm200007133430203
- The Canadian C-Spine Rule versus the NEXUS Low-Risk Criteria in Patients with Trauma. https://www.nejm.org/doi/full/10.1056/nejmoa031375
- Test performance of the individual NEXUS low-risk clinical screening criteria for cervical spine injury. https://www.sciencedirect.com/science/article/abs/pii/S0196064401762105
- Clinical examination and its reliability in identifying cervical spine fractures. https://pubmed.ncbi.nlm.nih.gov/17563656/
- The Canadian C-Spine Rule for Radiography in Alert and Stable Trauma Patients. https://jamanetwork.com/journals/jama/fullarticle/194296
- The Canadian C-spine rule performs better than unstructured physician judgment. https://pubmed.ncbi.nlm.nih.gov/12944893/
- Traumatic atlantoaxial rotatory subluxation (TAARS) in adults: A report of two cases and literature review. https://www.injuryjournal.com/article/S0020-1383(12)00020-4/fulltext
- Use of plain radiography to screen for cervical spine injuries. https://pubmed.ncbi.nlm.nih.gov/11423803/
- The early work-up for isolated ligamentous injury of the cervical spine: does computed tomography scan have a role? https://pubmed.ncbi.nlm.nih.gov/16374279/
- Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. https://pubmed.ncbi.nlm.nih.gov/15920400/
- Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. https://pubmed.ncbi.nlm.nih.gov/19741415/
- Cervical Spine Injury A Clinical Decision Rule to Identify High-Risk Patients for Helical CT Screening Read More: https://www.ajronline.org/doi/full/10.2214/ajr.174.3.1740713
- Cervical spine magnetic resonance imaging in alert, neurologically intact trauma patients with persistent midline tenderness and negative computed tomography results. https://pubmed.ncbi.nlm.nih.gov/21820209/
- The incidence of neurogenic shock in patients with isolated spinal cord injury in the emergency department. https://pubmed.ncbi.nlm.nih.gov/17688997/