Definition
Boerhaave syndrome is a spontaneous rupture of the esophagus. It usually results from barotrauma related to retching or any sudden increase in intraabdominal pressure against a closed glottis.
Epidemiology of Boerhaave Syndrome
Esophageal perforations are rare and Boerhaave syndrome even rarer, accounting for only about 15% of cases. However, the mortality from this disease varies from ~8% to 60% and increases significantly if care is delayed.
Although we have known about this syndrome for over 200 years, its associated morbidity and mortality remain high due to its nonspecific presenting symptoms and resulting delays in diagnosis.
Symptoms and Signs of Boerhaave Syndrome
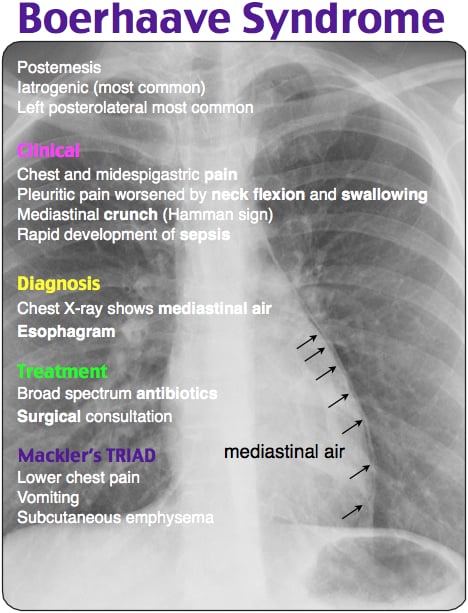
Classically, we associate Boerhaave syndrome with Mackler triad:
- retrosternal chest pain
- vomiting
- subcutaneous emphysema
Like with many other difficult diagnoses, these classic symptoms seldom present all together. Approximately 25% to 45% of patients have no history of vomiting, and even fewer have subcutaneous emphysema.
The diagnosis of Boerhaave syndrome should be suspected in any patient who presents with retrosternal chest pain, neck pain, or epigastric pain, especially if it began after an episode of severe retching or bearing down against a closed glottis (weight lifting, defecation, childbirth, etc.).
The location of pain generally correlates with the location of esophageal rupture, which most commonly occurs in the distal left posterolateral portion.
Be aware that the severity of symptoms may vary widely depending on the time from the actual rupture, ranging from simple retrosternal pain, to respiratory collapse, septic shock, and multisystem organ failure.
Diagnosing Boerhaave Syndrome
- Contrast esophagram (with Gastrografin) – Gold Standard.
- Chest CT can often suggest an esophageal perforation through the detection of:
- esophageal edema,
- periesophageal fluid, or
- air in the mediastinal or pleural spaces.
- CT esophagography,if clinical suspicion is high, can be performed using diluted oral contrast to allow visualization of the specific site of perforation.
- Although Endoscopy may aid in the diagnosis of Boerhaave syndrome, it is generally not recommended due to the risk of extending the esophageal tear through insufflation or direct trauma.
The key to diagnosing Boerhaave syndrome is merely to consider the diagnosis. Many cases, however, are diagnosed incidentally on chest radiographs (Chest X-Ray) that reveal:
- mediastinal air
- subcutaneous emphysema
- pneumothorax
- pleural effusion
Treatment of Boerhaave Syndrome
Once the diagnosis of Boerhaave syndrome is established, treatment should proceed rapidly. Even if a patient initially looks stable, decompensation may be rapid. Patients with Boerhaave syndrome should be regarded as critically ill and be monitored closely, especially in regard to their respiratory status.
- Many will present dehydrated and will require intravenous fluids while remaining NPO (nothing by mouth).
- Broadspectrum intravenous antibiotics should be initiated early including coverage of enteric organisms.
- Intravenous proton pump inhibitors may also be considered, so as to decrease the severity of chemical mediastinitis and pleuritis.
- Rapid surgical or endoscopic repair is the definitive treatment of Boerhaave syndrome. A surgical consultation should be placed early once the diagnosis is suspected, given that early repair has been shown to decrease morbidity and mortality. Nevertheless, in certain subgroups of esophageal perforation, such as cervical perforation, or contained perforation with limited extraluminal extravasation of fluid, nonoperative management may be considered.
Key Points
- Boerhaave syndrome is a rare disease that is almost universally fatal if treatment is not performed.
- Consider this syndrome in any patient that presents with retrosternal pain.
- Recognize that these patients are sick (or soon will be).
- Initiate intravenous fluids and broad-spectrum antibiotics early in the course of treatment.
- Consult surgery as soon as the diagnosis is suspected for expedited surgical or endoscopic repair.
References / Suggested Readings
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004;77(4):1475–1483.
- Garas G, Zarogoulidis P, Efthymiou A, et al. Spontaneous esophageal rupture as the underlying cause of pneumothorax: Early recognition is crucial. J Thorac Dis. 2014;6(12):1655–1658.
- Schweigert M, Beattie R, Solymosi N, et al. Endoscopic stent insertion versus primary operative management for spontaneous rupture of the esophagus (Boerhaave syndrome): An international study comparing the outcome. Am Surg. 2013;79(6):634–640.
- Tonolini M, Bianco R. Spontaneous esophageal perforation (Boerhaave syndrome): Diagnosis with CT-esophagography. J Emerg Trauma Shock. 2013;6(1):58–60.
- Wilson RF, Sarver EJ, Arbulu A, et al. Spontaneous perforation of the esophagus. Ann Thorac Surg. 1971;12(3):291–296.