Table of Contents
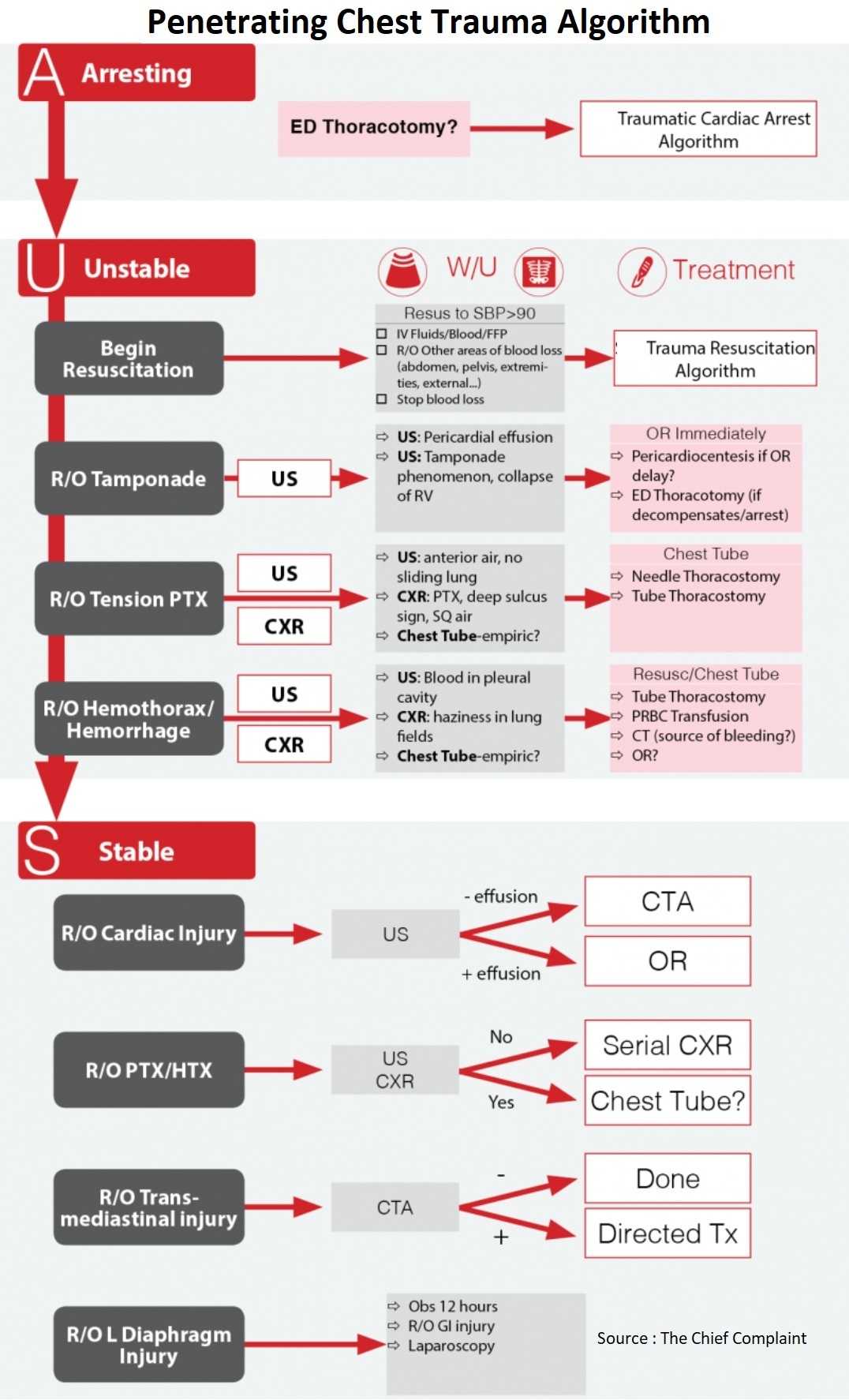
Arresting Patient
ED Thoracotomy indications:
- Trauma patient, CPR, no signs of life (SOL) +:
- Blunt trauma with CPR <10min
- Penetrating trauma with CPR <15min
- Penetrating trauma to neck/extremity < 5 min
No Signs of Life (SOL):
□ No pulse
□ No pupils
□ No movement
□ No breaths
□ No PEA
□ No cardiac motion (US)
Procedure:
- Resuscitative Thoracotomy (Open the left chest)
- Release tamponade and open resuscitation of heart
- Control bleeding
- Cross-clamp aorta → Shunt blood up
- Right Chest Tube
- Blood? → Clamshell thoracotomy to control bleeding
Survival rates:
- Overall survival rate 7.4%, dictated by location & mechanism of injury (J Am Coll Surg 2000;190:288- 98)
- Thoracic injury 10.7% (Cardiac-19.4%), abdominal injury 4.5%
- Penetrating injury 8.8% (stab wounds 17%, GSW 4.3%) blunt trauma 1.4%
Unstable Patient
Resuscitation (See Trauma Resuscitation Algorithm)
- Critical Actions
- Crystalloid resuscitation
- Initiate cross-matching
- Remains Unstable?
- Continue resuscitation
- Blood transfusion → uncross-matched or type specific
- Thaw FFP
- Target endpoint → SBP 90, talking
- Continue resuscitation
Localize bleeding (See Blunt Chest Trauma Algorithm)
- Cardiac Ultrasound
- Pericardial effusion
- Tamponade phenomenon, collapse of RV
- Lung Ultrasound
- Pneumothorax: Anterior air-no sliding lung
- Hemothorax: Blood in pleural cavity
- CXR (Chest X-Ray)
- Pneumothorax: deep sulcus sign, Subcutaneous air
- Hemothorax: haziness in lung fields
- Chest tube, Clinically directed
- Indications
- Hemothorax/Pneumothorax
- Clinical exam/diagnostic
- OR
- Output>1-1.5L
- Continuous output > 200-250ml/h X 2-4h
- Clinical judgment
- Indications
- Rule out other areas of blood loss (Pelvis, extremities, externally)
- Stop bleeding
Stable Patient
General
- ABCs
- IV, O2, Monitor …
Discharge Home Checklist:
□ Examinable
□ Isolated thoracic Injury
□ Negative U/S + radiographs
□ Serial clinical exams
□ Initial and repeat CXR @ 3 hours
What is at risk of injury?
- External wounds → roll early
- Plain X-rays → missile localization and trajectory mapping
Check for specific areas of injury
Pneumothorax
Diagnosis
- Lung Ultrasound as part of FAST
- Rule Out Pneumothorax:
- Initial CXR
- If CXR negative → Repeat CXR at 3 hours (J Trauma 2008;65:549-53)
- Previously would repeat CXR at 6 hours → No additional benefit gained from CXR at 6 vs 3 hours
Penetrating Cardiac Injury
Diagnosis
- Clinical exam, CXR, ECG, Pericardiocentesis → poor sensitivity and specificity
- Cardiac Ultrasound
- Annals of Surgery 1996;223(6):737-746 → Sens 100%, Spec 100%
- Annals of Surgery 1998;228(4):557-567 → Sens 100%, Spec 99.3%
- J Trauma. 2000 Dec;49(6):1159 → Sens 100%, Spec 97%
- Conclusion
- Ultrasound should be the initial diagnostic adjunct for precordial wounds
- Ultrasound is highly sensitive for cardiac injury, and immediate surgical intervention when positive
- ECHO: If US equivocal, may need formal Cardiac ECHO
Treatment
- OR immediately for sternotomy
- ER thoracotomy if too unstable for OR
- Pericardiocentesis if unable to perform thoracotomy
Transmediastinal Injury
Traditional approach
- Unstable → OR
- Stable → pan-endoscopy, contrast swallow, angiography, echo
CT as screening approach (J Trauma 2002;53:635–638) (Ann Thorac Surg. 2007;83:377-82):
- CT Negative → 100% Negative predictive value, no need for further testing
- CT positive
Left Thoracoabdominal Region Injury
Rule Out Diaphragm Injury
- Location:
- Superior: Nipple → scapula tip
- Inferior: Costal margin
- Delayed diagnosis
- If not diagnosed at time of trauma, diagnosis may be delayed many years
- Occult diaphragmatic injury in 26% of Stab Wound and 13% of Gunshot Wound at laparoscopy
- CXR
- May show pneumothorax, hemothorax, herniation of abdominal contents into chest or completely normal
- Usually non-diagnostic
- CT
- Accuracy 96% for diaphragm injury in one study (J Trauma 2007;63:538-43)
- Laparoscopy gold standard to exclude diaphragm injury
- LAC + USC Protocol:
- 6-12 hour observation to rule out GI tract injury
- Then laparoscopic eval +/- repair
- Rule out Pneumothorax as above
References
- Survival after emergency department thoracotomy: review of published data from the past 25 years. https://pubmed.ncbi.nlm.nih.gov/10703853/
- Follow-up after asymptomatic penetrating thoracic injury: 3 hours is enough. https://pubmed.ncbi.nlm.nih.gov/18784567/
- The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. https://europepmc.org/article/med/10217216
- Reevaluation of diagnostic procedures for transmediastinal gunshot wounds. https://pubmed.ncbi.nlm.nih.gov/12394859/
- Triage and outcome of patients with mediastinal penetrating trauma. https://pubmed.ncbi.nlm.nih.gov/17257952/
- Accuracy of computed tomography (CT) scan in the detection of penetrating diaphragm injury. https://europepmc.org/article/med/18073598