Table of Contents
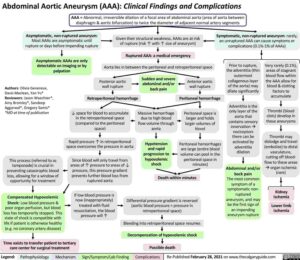
Acute aortic dissection (AD) is defined as a tear through the intima, which results in the flow of arterial blood between the layers of the aorta.
This intimal tear is usually preceded by degeneration of the medial layer of the aortic wall that is caused by various disease processes that include:
- atherosclerosis
- congenital weakness of structural components
- vasculitis
Regardless of the pathologic processes, the medial layer is weakened and can tear with any increase in aortic wall stress. The most common system used to classify acute ADs is the Stanford classification system.
Any dissection involving the ascending aorta is classified as Stanford type A, whereas Stanford type B is limited to dissections involving the descending aorta.
More recently, the term intramural hematoma (IMH) has been used to characterize a thrombus within the wall of the aorta that does not enhance with the administration of contrast agents for computed tomography or magnetic resonance imaging.
Since the clinical presentation and progression of IMH is similar to an acute Aortic Dissection, management of both conditions is identical. Regardless of the presence of an acute AD or IMH, hemodynamic monitoring in multiple limbs may be needed to obtain an accurate blood pressure measurement and guide therapy.
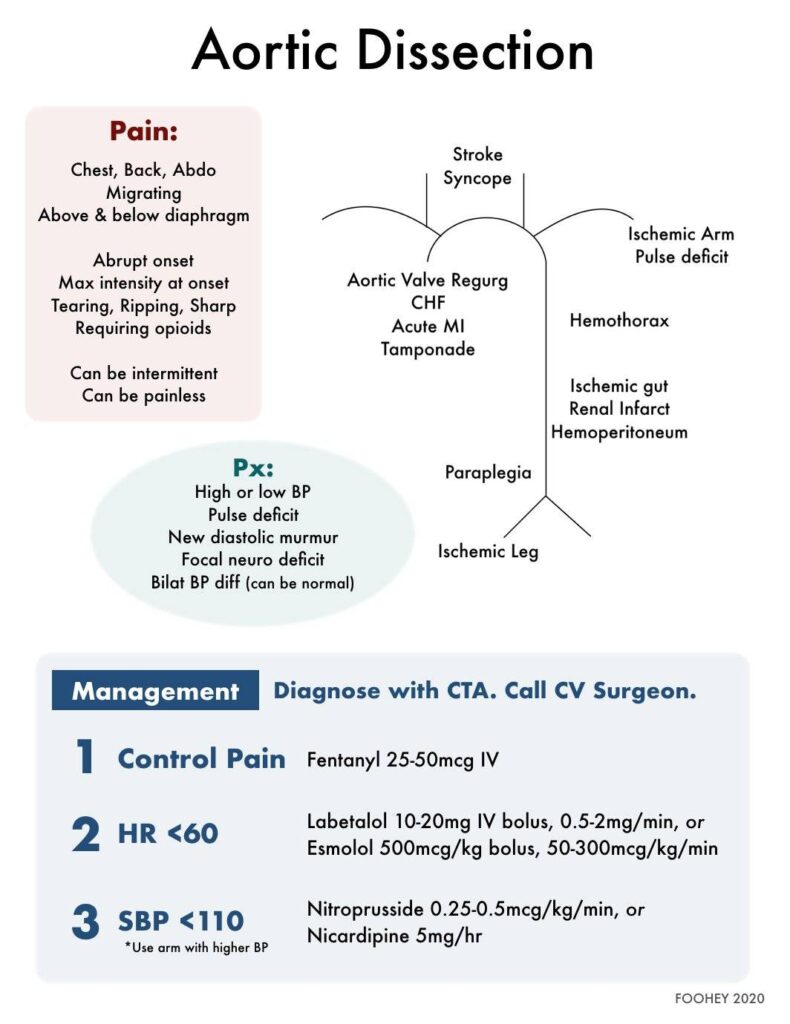
Aortic Dissection Management
The foundation of Aortic Dissection management is based on the theory that a reduction in sheer stress on the aortic wall will slow propagation of the dissection and prevent either aortic rupture or compromised flow to vital organs.
The therapeutic targets to reduce sheer stress are:
- blood pressure
- heart rate (HR)
Classic teaching is to:
- reduce the HR to ~60 beats per minute (bpm),
- rapid reduction in systolic blood pressure (SBP) to <120 mm Hg
Though recent consensus guidelines continue to recommend these targets for HR and SBP, it is important to note that these numbers have not been studied in prospective or randomized trials. In fact, there is only scant observational evidence that reducing HR has any effect on mortality. To that end, current European guidelines for the treatment of Aortic Dissection focus on blood pressure reduction alone.
The most reasonable approach to managing patients with acute Aortic Dissection is to lower SBP and HR as much as tolerable while maintaining perfusion to vital organs. Therapy should be individualized and based on markers of end organ perfusion, such as mentation and urine output.
Medical Management of Aortic Dissection
Beta-blockers
Beta-blocker medications are recommended as the initial agent in acute Aortic Dissection. This will lower HR as well as blunt potential reflex tachycardia commonly seen with vasodilatory medications.
Esmolol and labetalol are the two most common beta-blocker medications used. Both can be administered as continuous infusions.
Esmolol has the advantage of a shorter half-life compared with labetalol, should the infusion need to be discontinued due to hemodynamic compromise.
Importantly, beta-blockers should be avoided in patients with acute aortic insufficiency (i.e., new diastolic murmur, pulmonary edema, tachycardia), as they may cause cardiovascular collapse.
Calcium Channel Blockers
For patients in whom beta-blockers are contraindicated or poorly tolerated, a calcium channel blocker (e.g., diltiazem) can be used.
Vasodilatory Agents
Following a reduction in HR, vasodilatory agents (e.g., nicardipine) should be administered to reduce SBP.
Analgesic Medications
Do not forget to administer an analgesic medication to patients with an acute Aortic Dissection. Pain contributes to elevation of HR and SBP and should be managed. Intravenous opioids (e.g., fentanyl) are recommended.
Surgical Management of Aortic Dissection
Immediate surgical consultation should be obtained for:
- Stanford type A dissections
- complicated Stanford type B dissections
- those at high risk for impending aortic rupture
Complicated Stanford type B dissections are those that demonstrate end organ ischemia to organs such as the spine, kidney, and splanchnic circulation.
Stanford type B dissections that do not have evidence of end organ ischemia or impending rupture are generally managed medically with control of blood pressure and HR.
For patients with an acute Aortic Dissection complicated by cardiac tamponade, pericardiocentesis should be performed only as a last resort. If necessary, remove only enough blood to restore adequate circulation while preparing to move the patient to the operating room. Additional fluid removal may increase flow and propagation of the false lumen.
Key Points
- Current guidelines recommend rapidly reducing HR to approximately 60 bpm followed by a reduction in SBP to 120 mm Hg.
- Beta-blocker medications, such as esmolol or labetalol, are the initial recommended agents to reduce HR.
- Administer a vasodilator agent once HR is controlled.
- Administer an analgesic, such as fentanyl, to all patients with an acute Aortic Dissection.
- Stanford type A, complicated Stanford type B, and those with signs of impending rupture should receive emergent operative therapy.
Suggested Readings
- Diercks DB, Promes SB, Schuur JD, et al. Clinical policy: critical issues in the evaluation and management of adult patients with suspected acute nontraumatic thoracic aortic dissection. Ann Emerg Med. 2015;65:32–42. https://pubmed.ncbi.nlm.nih.gov/25529153/
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. Circulation. 2010;121:e266–e369. https://pubmed.ncbi.nlm.nih.gov/20233780/
- Tsai, TT, Nienaber CA, Eagle KA. Acute aortic syndromes. Circulation. 2005;112:3802–3813. https://pubmed.ncbi.nlm.nih.gov/16344407/