Table of Contents
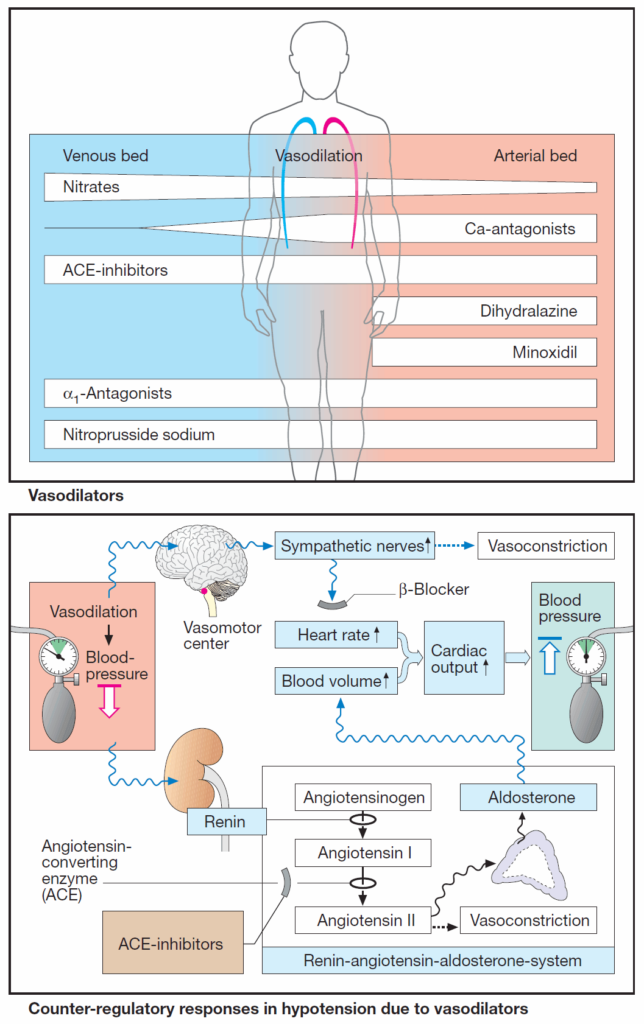
The distribution of blood within the circulation is a function of vascular caliber. Venous tone regulates the volume of blood returned to the heart, hence, stroke volume and cardiac output.
The luminal diameter of the arterial vasculature determines peripheral resistance. Cardiac output and peripheral resistance are prime determinants of arterial blood pressure.
In the image bellow, the clinically most important vasodilators are presented in the order of approximate frequency of therapeutic use. Some of these agents possess different efficacy in affecting the venous and arterial limbs of the circulation (width of beam).
Possible uses of Vasodilators
Arteriolar vasodilators are given to:
- lower blood pressure in hypertension
- reduce cardiac work in angina pectoris
- reduce ventricular afterload (pressure load) in cardiac failure.
Venous vasodilators are used to:
- reduce venous filling pressure (preload) in angina pectoris or cardiac failure .
Practical uses are indicated for each drug group.
Counter-regulation in Acute Hypotension due to Vasodilators
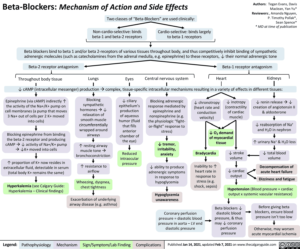
Increased sympathetic drive raises heart rate (reflex tachycardia) and cardiac output and thus helps to elevate blood pressure. Patients experience palpitations.
Activation of the renin-angiotensin- aldosterone (RAA) system serves to increase blood volume, hence cardiac output. Fluid retention leads to an increase in body weight and, possibly, edemas.
These counter-regulatory processes are susceptible to pharmacological inhibition (β-blockers, ACE inhibitors, AT1-antagonists, diuretics).
Mechanisms of Action of Vasodilators
The tonus of vascular smooth muscle can be decreased by various means.
- ACE inhibitors, antagonists at AT1-receptors and antagonists at α-adrenoceptors protect against the effects of excitatory mediators such as angiotensin II and norepinephrine, respectively.
- Prostacyclin analogues such as iloprost, or prostaglandin E1 analogues such as alprostanil, mimic the actions of relaxant mediators.
- Calcium (Ca2+) antagonists reduce depolarizing inward Ca2+ currents, while K+-channel activators promote outward (hyperpolarizing) K+ currents.
- Organic nitrovasodilators give rise to NO, an endogenous activator of guanylate cyclase.
Individual Vasodilators
- Nitrates
- Calcium (Ca2+) – antagonists
- α1- antagonists
- ACE-inhibitors
- AT1- antagonists
- sodium nitroprusside
- Dihydralazine and minoxidil
- Diazoxide
Dihydralazine and Minoxidil
Dihydralazine and minoxidil (via its sulfate-conjugated metabolite) dilate arterioles and are used in antihypertensive therapy. They are, however, unsuitable for monotherapy because of compensatory circulatory reflexes.
Mechanism of action
The mechanism of action of dihydralazine is unclear. Minoxidil probably activates K+ channels, leading to hyperpolarization of smooth muscle cells.
Adverse Reactions
Particular adverse reactions are lupus erythematosus with dihydralazine and hirsutism with minoxidil—used topically for the treatment of baldness (alopecia androgenetica).
Diazoxide
Diazoxide given i.v. causes prominent arteriolar dilation; it can be employed in hypertensive crises. After its oral administration, insulin secretion is inhibited. Accordingly, diazoxide can be used in the management of insulin-secreting pancreatic tumors. Both effects are probably due to opening of (ATPgated) K+ channels.
Other Drugs that Possess Vasodilating Activity
- methylxanthine theophylline
- phosphodiesterase inhibitor amrinone
- prostacyclins
- nicotinic acid derivatives