Table of Contents
- Mild hypothermia → tachypnea, tachycardia, hyperventilation, ataxia, shivering, impaired judgment, “cold diuresis”
- Moderate → bradycardia, hypoventilation, CNS depression, loss of shivering, slow A-fib + other arrhythmias
- Severe → pulmonary edema, oliguria, coma, pupils fixed/dilated, ventricular arrhythmias, asystole
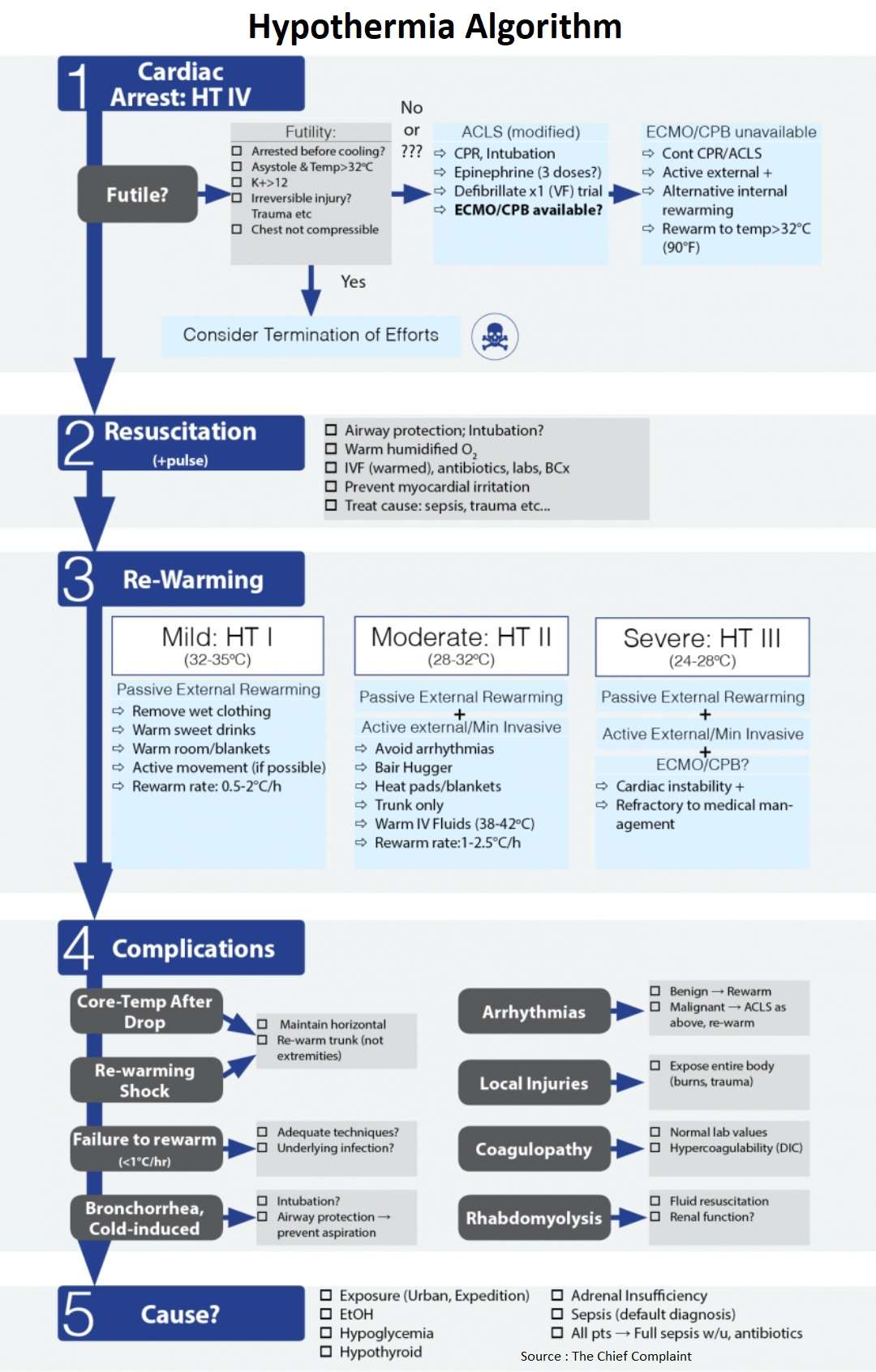
Cardiac Arrest from Hypothermia
Futile? Consider termination of efforts if :
- Irreversible injury ?
- Decapitation, truncal transection, decomposition of the whole body, and a chest wall that is not compressible (the whole body is frozen solid)
- K+ (potassium) > 10-12 mmol/L
- Serum K+ > 10 mmol/L may be a valuable prognostic indicator for irreversible asphyxia and death. (Ann Emerg Med 1987;16:1042-55)
- Cardiac arrest prior to cooling
- Difficult to differentiate from a patient that died and then became hypothermic → resuscitation would obviously be futile
- Better outcome if patients were cooled before heart stopped
- Asystole and Temp > 32°C
- Hypothermia is then not the cause of arrest
Special Cases (trauma, drowning, avalanche)
- Trauma
- Hypothermia will decrease survival of blunt trauma
- Drowning
- Avalanche (3 ways to die)
- Traumatic arrest
- Hypoxic arrest (airway filled with snow)
- Hypothermic arrest
- Patient must be buried long enough to cool → then arrest
- Rate of cooling 10oC/h so must be buried at least 35 minutes
Continued CPR/Resuscitation
- Because of neuroprotective effects of hypothermia → complete recovery is possible even if prolonged resuscitation (hours)
- Survival and neurological recovery reported in temperatures as low as 13.7°C and cardiac arrest > 9 hours (Lancet 2000;355:375-6)
- Continue resuscitation until temperature is 32-35°C
Modified ACLS
- CPR, Intubation
- Rapid re-warming: ECMO/CPB
- Resuscitate until temp >32°C (90°F)
- Defibrillate x1 (VF) trial then rewarm
- Epinephrine x 1 trial then rewarm vs up to 3 doses
- ACLS recommendations
- European Resuscitation Council (Resuscitation 2010;81:1400)
- Defibrillations: up to 3
- Epinephrine: hold until core temp > 30°C then double interval between doses until temp > 35°C
- AHA Guidelines (Circulation 2010;122:Suppl 3: S829-S861)
- Standard ALS protocol
- European Resuscitation Council (Resuscitation 2010;81:1400)
ECMO/CPB
- Define: Extracorporeal Membrane Oxygenation(ECMO) / Cardiopulmonary Bypass (CPB)
- Indications:
- Cardiac arrest (Hypothermia stage IV)
- Hypothermic patients who experience cardiac arrest have a survival rate of 50% when treated in an ECMO center but only 10% in a non-ECMO center
- Cardiac instability refractory to medical management (Hypothermia stage III)
- SBP < 90, ventricular arrhythmias, temp < 28oC
- Cardiac arrest (Hypothermia stage IV)
- In patients with ROSC, multiorgan failure is expected → respiratory support with ECMO may be required.
Termination of CPR
- Consider termination if temp > 32oC and persistent cardiac arrest, not responsive to epinephrine and defibrillation
Hypothermia Resuscitation
Intubation
- Risk of causing VF very low and outweighed by benefits of reliable ventilation, oxygenation, prevention of aspiration – especially if comatose or respiratory failure
Sepsis
- Treat all patients empirically for sepsis
- IVF (warmed), antibiotics, labs, blood cultures, lactate
- See Sepsis algorithm
Re-warming and Hypothermia Stages
General
- Degree of hypothermia and mortality will determine the aggressiveness of re-warming
| Stage | Temperature | Clinical |
| Hypothermia Stage I | 32-35 °C | Conscious Shivering |
| Hypothermia Stage II | 28-32 °C | Impaired consciousness, No shivering |
| Hypothermia Stage III | 24-28 °C | Unconscious, No shiver, Patient has vital signs |
| Hypothermia Stage IV | <24 °C | No vital signs |
Hypothermia Stage I
- Clinical: conscious, shivering
- Treatment
- Passive External Rewarming (0.5-2°C/h)
- Remove wet clothing
- Warm room/blankets
- Passive External Rewarming (0.5-2°C/h)
Hypothermia Stage II
- Clinical: Impaired consciousness, not shivering
- Treatment
- Avoid arrhythmias
- Cardiac monitor
- Minimal/cautious movements
- Horizontal position and immobilization
- Active external/minimally invasive Re-warming (1-2.5°C/h)
- Bair Hugger
- Heat pads/blankets
- Trunk only
- Warm IV Fluids (38-42°C)
- Indications (N Eng J Med 1994;331:1756-60):
- i. Cardiovascular instability, poikilothermia (T<32°C), failure to re-warm, comorbidities
- Avoid arrhythmias
Hypothermia Stage III
- Clinical: Impaired consciousness, not shivering, patient has vital signs
- Treatment
- Hypothermia Stage II treatments
- Airway management as required
- ECMO/CPB (cardiac instability refractory to medical management)
Hypothermia Stage IV
- Clinical: Cardiac arrest, no vital signs
- Treatment
- Hypothermia Stage II and III treatments
- ACLS: CPR, Intubation, epinephrine, defibrillation
- ECMO/CPB if available (N Engl J Med 1997;337:1500-5) (Resuscitation 2003;59:285-90)
- Rate of survival without neurologic impairment is 47 to 63% (vs 37% without ECMO/CPB)
- Cardiopulmonary bypass (CPB) for severe hypothermia and cardiac arrest showed survival rate of 47-63% with minimal to no cerebral impairment, even after prolonged cardiac arrest
- Active external and alternative internal rewarming (ECMO/CPB not available)
- Thoracic lavage with chest tubes
- Bladder lavage?
Complications of Hypothermia
- Rescue collapse
- Define: cardiac arrest that is related to the extrication and transport of a patient with deep hypothermia (stage Hypothermia III)
- Cause: circulatory collapse due to hypovolemia, cardiac arrhythmias triggered by interventions, and further cooling
- Core temperature after drop
- Extremities and trunk are warmed simultaneously → cold, acidemic blood in periphery returns to core → drop in temperature and acidosis
- Rewarming shock
- Peripheral vasodilation → hypotension, low coronary perfusion → fatal arrhythmias (VF)
- Prevention: maintain horizontal, re-warm trunk before extremities
- Arrhythmias
- Avoid jarring pt, no high central lines, gentle movement of patient → irritating myocardium may cause VF
- Most (A-fib, A-flutter) resolve spontaneously during re-warming
- Normal course: bradycardia → slow A-fib → VF → Asystole (refractory to conventional tx, must be rewarmed!)
- EKG changes with hypothermia
- Intervals prolonged: PR, QRS, QT
- J point elevation (Osborne wave – characteristic but not pathognomonic: also seen in hypercalcemia and head injury)
- Failure to re-warm
- Evaluate for adequate aggressiveness for severity of hypothermia
- Evaluate for reversible causes (hypoglycemia)
- Underlying infection?
- Rewarming rates <0.67°C/hr associated with underlying infection and increased mortality (Acad Emerg Med 2006;13:913–921)
- Coagulopathy
- Cold directly inhibits enzymes of coagulation cascade and platelets → normal laboratory evaluation
- Hypercoagulability also present → can lead to thromboembolism; DIC
- Cold induced bronchorrhea
- Intubation? Airway protection → prevent aspiration
- Cold induced diuresis
- Usually diuresed 2-5L, replace with warmed IV Fluids
- Rhabdomyolysis
- Tissue ischemia and cellular destruction by freezing tissue
Causes of Hypothermia
- Environment
- Urban hypothermia
- Most common cause is environmental exposure with acute alcohol intoxication
- Expedition hypothermia
- Urban hypothermia
- Sepsis/Infection
- Treat all patients empirically for sepsis
- Associated with slower re-warming rates (above)
- Begin empiric broad spectrum antibiotics and sepsis work-up
- Adrenocortical insufficiency
- Consider empiric Hydrocortisone 100mg IV q8h or Dexamethasone
- Hypothyroidism/Myxedema Coma
References
- Accidental hypothermia. https://pubmed.ncbi.nlm.nih.gov/23150960/
- Diagnosis and treatment of hypothermia. https://pubmed.ncbi.nlm.nih.gov/15617296/
- Multicenter hypothermia survey. https://www.sciencedirect.com/science/article/abs/pii/S0196064487807576
- Resuscitation from accidental hypothermia of 13.7 degrees C with circulatory arrest. https://pubmed.ncbi.nlm.nih.gov/10665559/
- European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. https://pubmed.ncbi.nlm.nih.gov/20956045/
- Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. https://pubmed.ncbi.nlm.nih.gov/20956228/
- Accidental Hypothermia. https://www.nejm.org/doi/full/10.1056/nejmra1114208
- Outcome of survivors of accidental deep hypothermia and circulatory arrest treated with extracorporeal blood warming. https://pubmed.ncbi.nlm.nih.gov/9366581/
- Outcome from severe accidental hypothermia in Southern Finland–a 10-year review. https://pubmed.ncbi.nlm.nih.gov/14659598/
- Rewarming Rates in Urban Patients with Hypothermia: Prediction of Underlying Infection. https://onlinelibrary.wiley.com/doi/abs/10.1197/j.aem.2006.05.022