Table of Contents
Intraosseous (IO) access can serve as a lifesaving alternative to intravenous (IV) access, especially in the crashing hypovolemic patient. The noncollapsible medullary space of bone is a reliable entry point into the vascular system in patients with difficult or delayed IV access.
In the crashing patient, do not let IV access serve as a delay in administering lifesaving medications, fluids, or blood products! Instead, move quickly to obtaining IO access.
Numerous studies have shown that IO access is faster, easier, and just as reliable as IV access. This is true for patients of all ages (newborns, infants, children, and adults).
Where can Intraosseous (IO) be placed ?
Depending on the clinical scenario, IO access can be placed in the proximal humerus, proximal tibia, or distal tibia. There are no limitations to what can be instilled through the medullary space of the bone.
What are the infusion rates through Intraosseous (IO) line
All medications, fluids, and blood products can be transfused through the IO route. However, infusion rates do depend on the site of access. The proximal humerus has been shown to have an infusion rate under pressure of ~5 L/h, compared to ~1 L/h through the proximal/distal tibia.
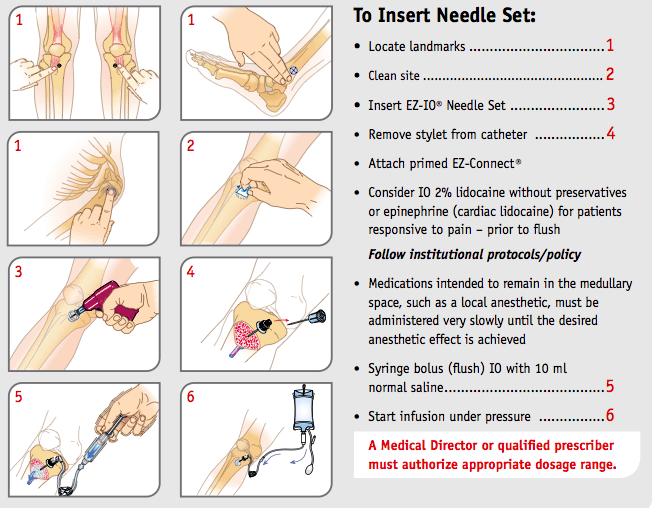
Placing an Intraosseous (IO) line
When placing an IO line it is important to palpate for your landmarks.
- In the extended leg, the proximal tibia insertion site is ~2 cm below the patella and 2 cm medial.
- The distal tibia insertion site is located ~3 cm proximal to the most prominent aspect of the medial malleolus.
- The IO needle should be inserted at a 90-degree angle when accessing the tibia.
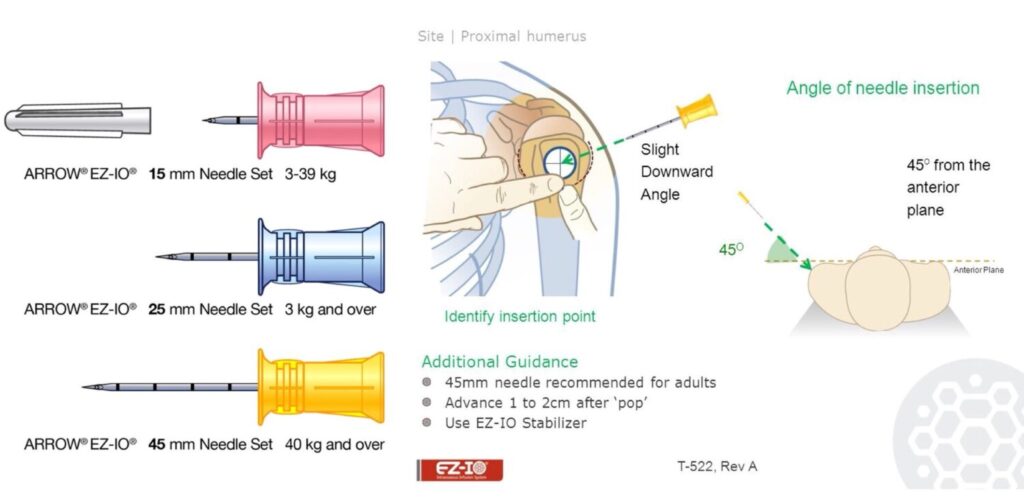
- The humerus insertion site is on the most prominent aspect of the greater tubercle
- When accessing the proximal humerus, position the patient with the hand resting on the abdomen (so that the elbow is adducted and the shoulder is internally rotated).
- The needle should be angled downward at a 45-degree angle.
Once your landmarks have been verified, the needle should be inserted through the skin and soft tissue until it comes in contact with bone. Do not engage the drill until the needle has passed through the skin/soft tissue and is resting in the appropriate orientation on the bone!
At this time, the drill should be engaged with firm pressure until the operator feels a pop as the needle enters the medullary space of the bone.
Needle length should be chosen based on the level of overlying soft tissue. If your needle is resting on the periosteum and you are unable to see at least one black line on the needle shaft — your needle is too small and will not be able to properly enter the medullary space!
Laboratory values from intraosseous line sample
Basic lab work is vital in ED management decisions, particularly in the critically ill. A CBC drawn from an IO will have hemoglobin and hematocrit levels that closely correlate to IV blood samples; however, platelet level may be low and WBC count may be high.
Additionally, many of the lab values from the BMP including glucose, BUN, creatinine, chloride, albumin, and total protein levels will be similar when compared to IV blood draws; however, potassium, CO2, sodium, and calcium levels may vary. Blood drawn from the IO line should be sent for analysis; however, it should be interpreted in the correct clinical context!
Contraindications
Contraindications to intraosseous (IO) placement include:
- overlying cellulitis/abscess
- fracture
- previous or failed IO placement within the past 48 hours in the target bone.
A fracture or previous IO placement in the target bone will lead to extravasation of fluid out of the medullary space and into the soft tissue, which places the patient at risk for compartment syndrome!
Removal of intraosseous line
Removal should be performed within 24 hours. Simply attach a Luer- Lok syringe onto the IO needle and apply firm upward force while turning in a clockwise fashion. Pull straight out; do not bend or rock the needle as this can lead to a retained foreign body!
Key Points
- Intraosseous access can be obtained in patients of all ages (newborns, infant, children, and adults).
- Common intraosseous access sites include the proximal humerus, proximal tibia, and distal tibia (may remain in place for 24 hours).
- All medications, fluids and blood products can be administered through the intraosseous route.
- A CBC drawn from an IO may have low Platelet and high WBC.
- A Basic Metabolic Panel from IO sample may have varying levels of potassium, CO2, sodium, and calcium
- Flow rate varies depending on insertion site: ~5 L/h through the humerus and 1 L/h through the tibia.
- IO access is contraindicated if a fracture is present in the targeted osseous infusion site or if previous IO access has been attempted in the same site in the past 48 hours.