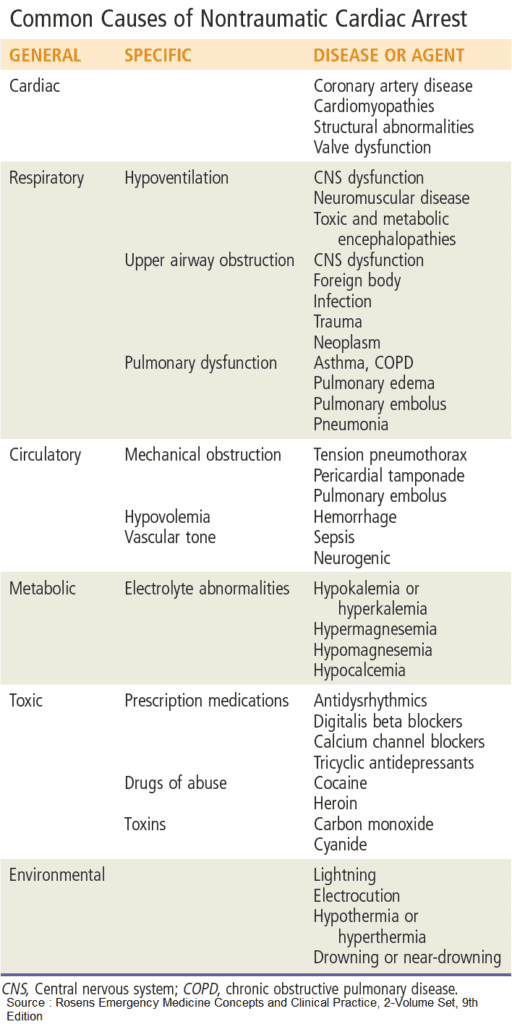
Cardiac arrest (CA) can be defined as the acute loss of heart function, either instantaneously or following a range of symptoms, ultimately leading to an arrest of circulation.
Clinically, the three classic characterizing features of Cardiac arrest are :
- Pulselessness
- Unresponsiveness and
- Abnormal breathing—either agonal or absent.
The estimated annual incidence of out-of-hospital Cardiac arrest ranges anywhere from 250,000 to 420,000 and is still one of most common causes of death in the United States. There is a multitude of underlying etiologies with ischemic heart disease being the most common.
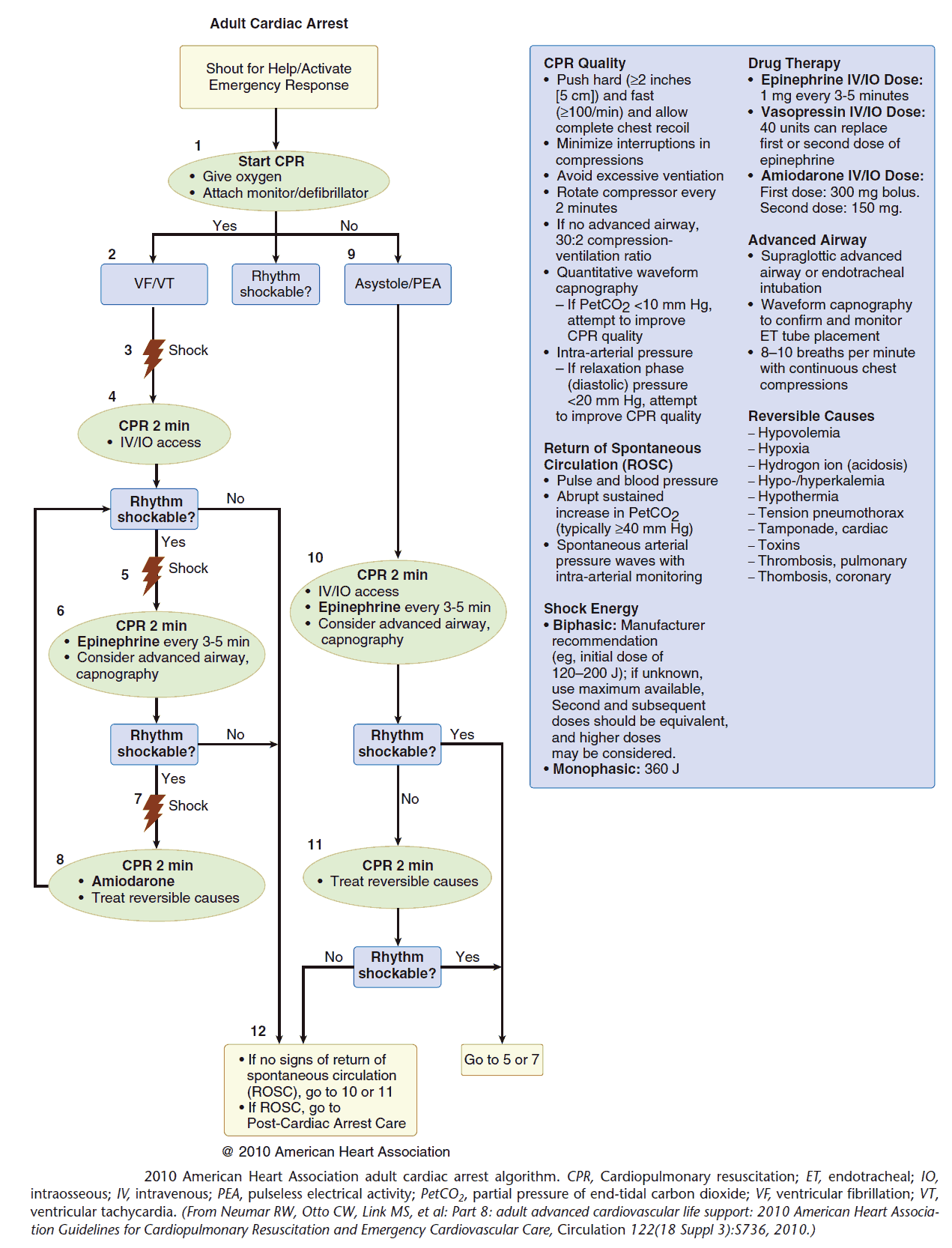
There are four main conduction rhythms of Cardiac arrest :
- Shockable with a more favorable outcome:
- Ventricular fibrillation (VF)
- Pulseless ventricular tachycardia (pVT).
- Nonshockable
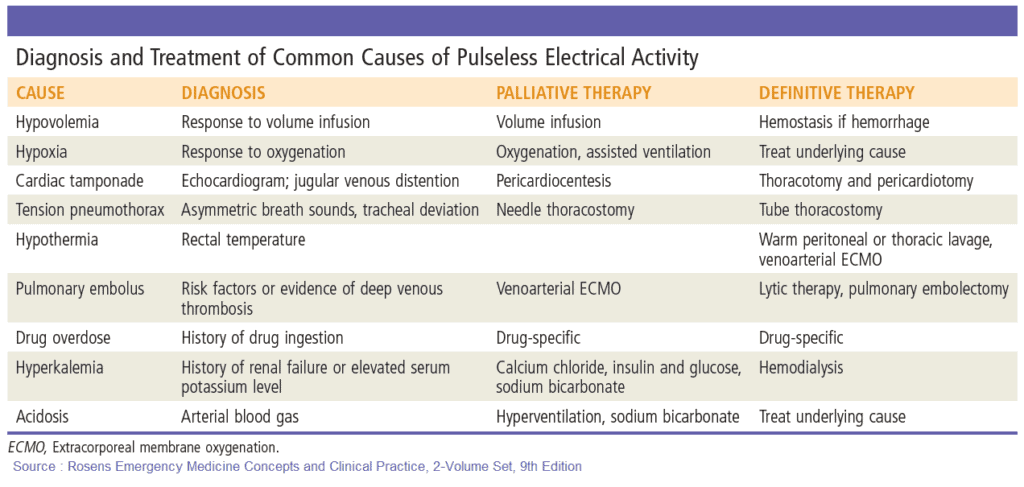
- Pulseless electrical activity (PEA)
- Asystole.
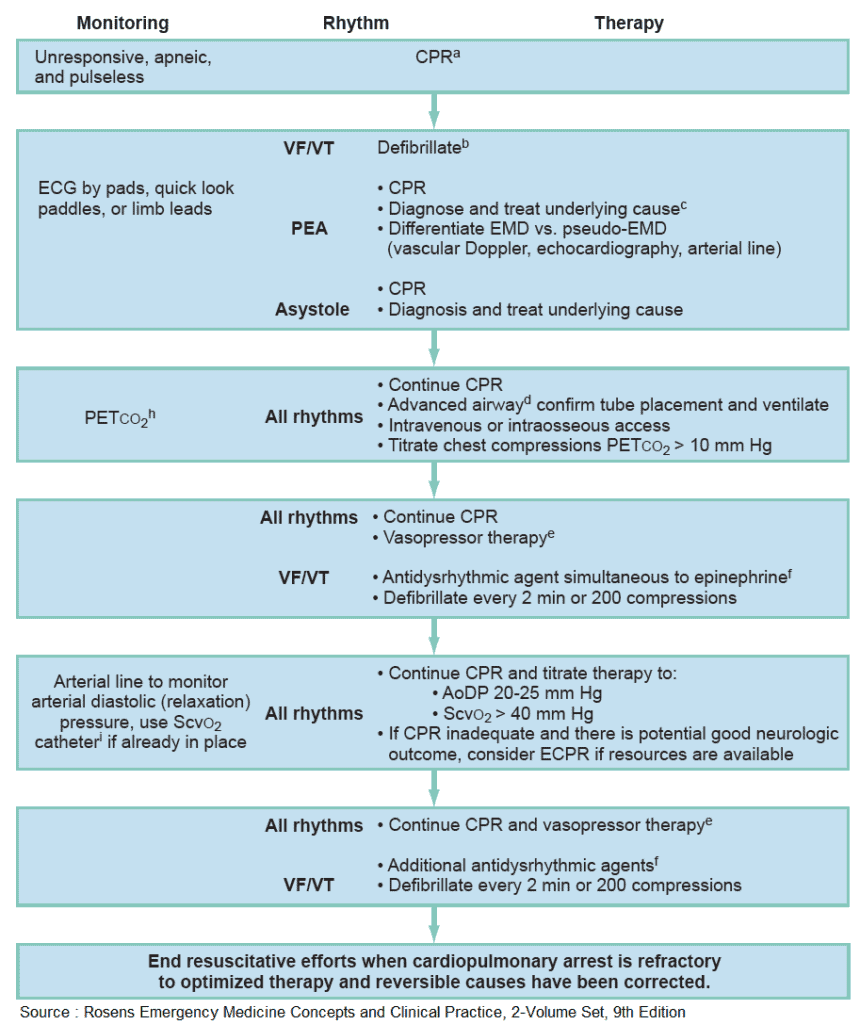
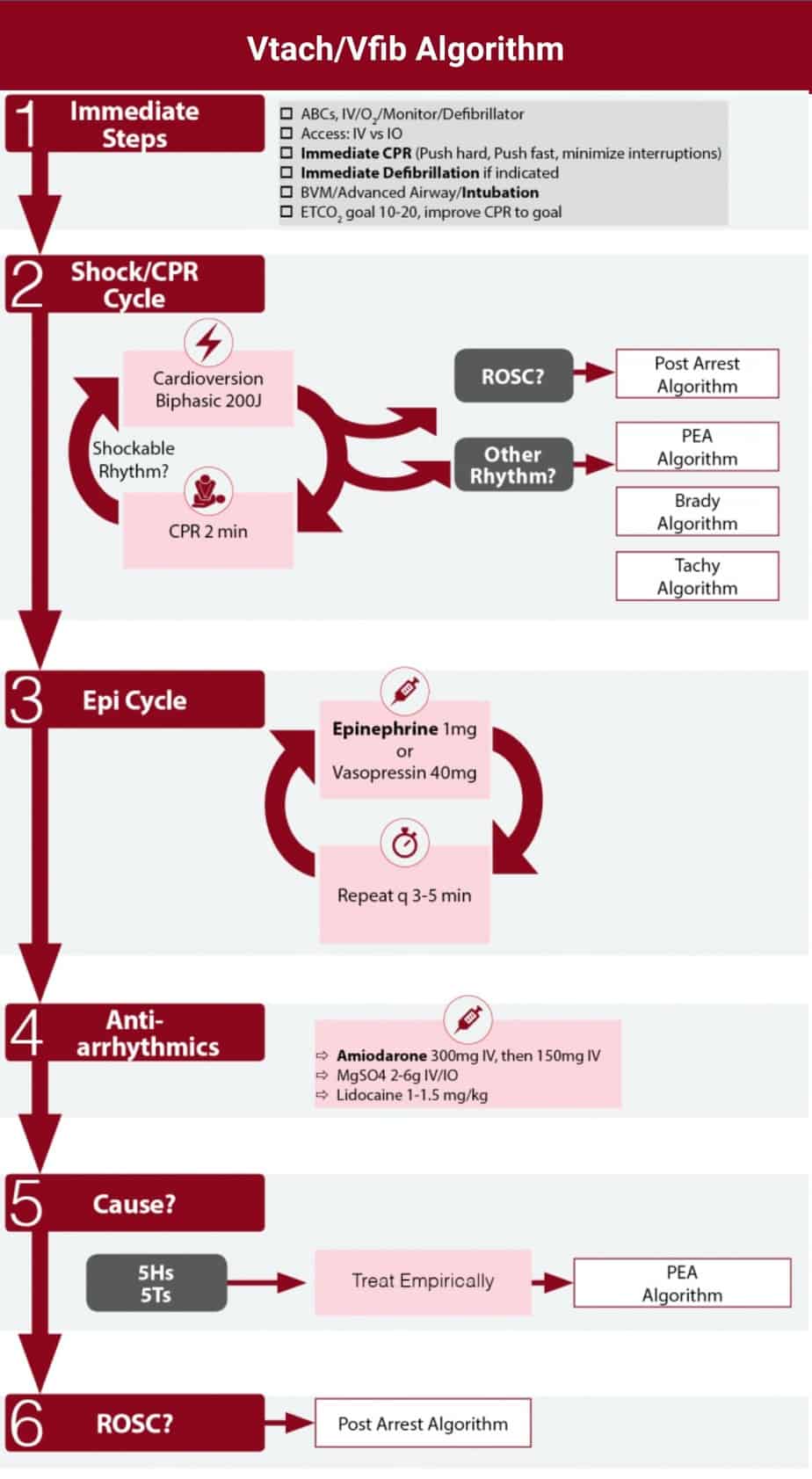
(a) If arrest is witnessed and known to be of short duration, immediate rhythm assessment and defibrillation or ventricular fibrillation/ventricular tachycardia (VF/VT) precede cardiopulmonary resuscitation (CPR).
(b) Biphasic defibrillation should use manufacturer-recommended energy versus monophasic defibrillation (360J).
(d) Endotracheal intubation or supraglottic airway, when feasible, with minimal interruption in chest compressions.
(e) Epinephrine, initial dose of 1 mg IV or IO. Repeat every 3 to 5 minutes. Subsequent doses may be increased up to 0.1 mg/kg. An alternative to epinephrine is vasopressin, 40 U, via IV push. The dose (40 U) can be repeated once in 3 minutes, followed by the administration of epinephrine every 3 to 5 minutes.
(f) Amiodarone, 300 mg via IV push, followed by 150 mg every 30 minutes. Lidocaine is an alternative antidysrhythmic if amiodarone is not available; magnesium sulfate, 1 to 2 g via IV push in torsades de pointes or known hypomagnesemia, may be given.
(h) Changes in the partial pressure of end-tidal carbon dioxide (PETCO2) may not be predictive of myocardial blood flow in the setting of high-dose vasopressor therapy.
(i) Invasive monitoring should be performed only if adequate personnel are available and if it would not delay therapeutic interventions. AoDP, Aortic diastolic pressure; ECG, electrocardiogram; EMD, electromechanical
dissociation; PEA, pulseless electrical activity; ScvO2, central venous oxygen saturation.
Whether occurring at home, in the public setting, or in the hospital, prompt recognition of Cardiac arrest is key. Early activation of emergency response systems, initiation of high-quality cardiopulmonary resuscitation (CPR), and expedient use of automated external defibrillators (AEDs) are absolutely paramount. Swift deliverance of high-quality CPR can prevent progression of shockable rhythms to nonshockable rhythms and increase successful defibrillation rates, chances for survival, and neurologic integrity.
There is much more to high-quality CPR than simply pushing on a patient’s chest. This is critical because even though high-quality CPR is one of the few interventions that has been shown to improve CA outcomes, it is still performed ineffectively in many cases. The most frequent deficits in high-quality CPR are inadequate rate and depth of chest compressions. With hands positioned on the lower half of the patient’s sternum, compressions should be performed :
- at a rate of 100 to 120 per minute
- at a minimum depth of 2 inches (5 cm) and no >2.5 inches (6 cm).
- Compressors should allow for full chest wall recoil in between compressions and avoid leaning on the chest.
Appropriate ventilation rates are also important. A single resuscitator should follow a
- 30:2 compressions-to-rescue breath ratio.
- When additional personnel are available, one breath every 6 seconds (10 per minute) should be given.
Medications used in Cadiac arrest
EPINEPHRINE
In 2014, a large systematic review of the literature was able to identify only one randomized controlled trial (RCT) comparing epinephrine to placebo that showed higher rates of return of spontaneous circulation (ROSC) and survival to admission after out-of-hospital cardiac arrest, in favor of epinephrine. However, the trial showed no difference in long-term neurologic outcome and survival to discharge.
- Currently, the AHA still recommends administering a 1-mg dose of epinephrine (1:10,000 concentration) via the intravenous (IV) or intraosseous (IO) route, or 2 to 2.5 mg endotracheally, every 3 to 5 minutes during cardiac arrest.
VASOPRESSIN
Due to its equivalence to epinephrine, the AHA has simplified its algorithms and no longer recommends the use of vasopressin.
AMIODARONE
- Amiodarone is a class 1, 2, and 4 antiarrhythmic, and its use is currently recommended for refractory shockable rhythms, namely, ventricular tachycardia (VT) and VF.
- A systematic review in 2013 showed no benefit of amiodarone compared to placebo with respect to survival to hospital discharge, but showed higher rates of ROSC and survival to admission.
- The 2010 ACLS guidelines recommend an initial dose of 300 mg amiodarone IV/IO followed by one dose of 150 mg for refractory ventricular fibrillation or pulseless VT.
MAGNESIUM SULFATE
Magnesium sulfate may be used for special situations in cardiac arrest.
- For torsades de pointes (polymorphic VT associated with prolonged QT interval)
- Magnesium sulfate can be administered as an IV/IO bolus at a dose of 1 to 2g diluted in 10 mL D5W.
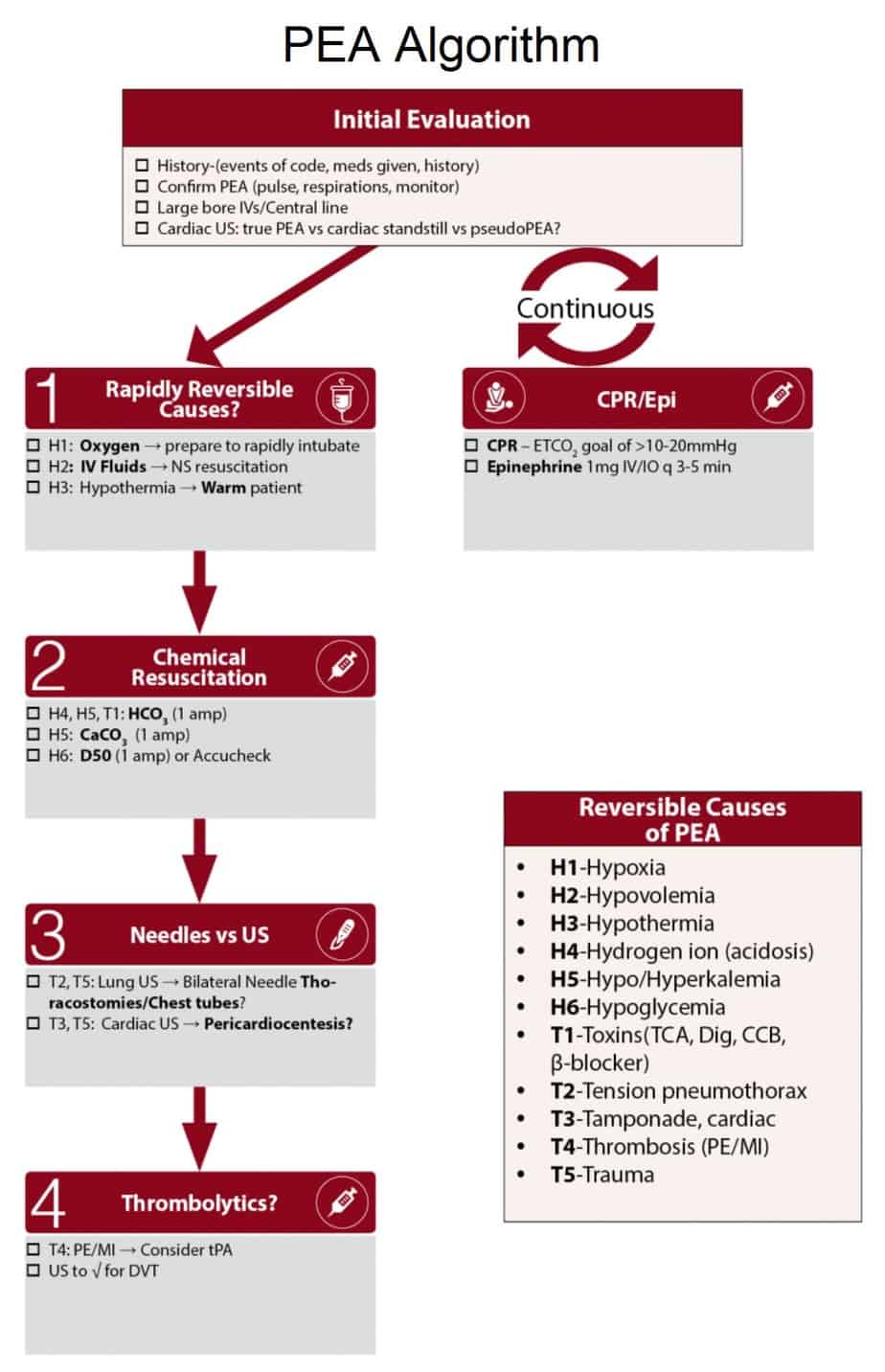
SODIUM BICARBONATE
Sodium bicarbonate is recommended for:
- Severe acidosis,
- Hyperkalemia
- TCA overdose.
Key Points
- Early recognition of Cardiac Arrest with prompt implementation of high-quality CPR is critical and can improve survival outcomes.
- High-quality CPR includes ensuring adequate rate and depth of chest compressions, allowing for chest wall recoil, avoiding excessive ventilation, and limiting compression pauses to no more than 10 seconds with a minimum total time of chest compressions during a resuscitation of 60%.
- Early defibrillation for ventricular fibrillation and pulseless ventricular tachycardia improves survival outcomes and should not be delayed.
- Epinephrine is still the most widely used drug in cardiac arrest, regardless of presenting rhythm.
- Vasopressin is no longer recommended due to its equivalent nature to epinephrine.
- Amiodarone may be used in cardiac arrest with VT or VF refractory to defibrillation.
- Magnesium is recommended for polymorphic VT, also known as torsades de pointes.
- Sodium bicarbonate is recommended for severe acidosis, hyperkalemia, and TCA overdose.