Achieving return of spontaneous circulation (ROSC) after a cardiac arrest is one of the most satisfying and encouraging experiences in emergency medicine. It can be easy to forget that work yet remains to maximize the patient’s likelihood of neurologic recovery. Though research in the field is limited, there is literature to support objectives that every provider should consider when caring for a patient who has been resuscitated after an arrest.
Maximize Perfomance
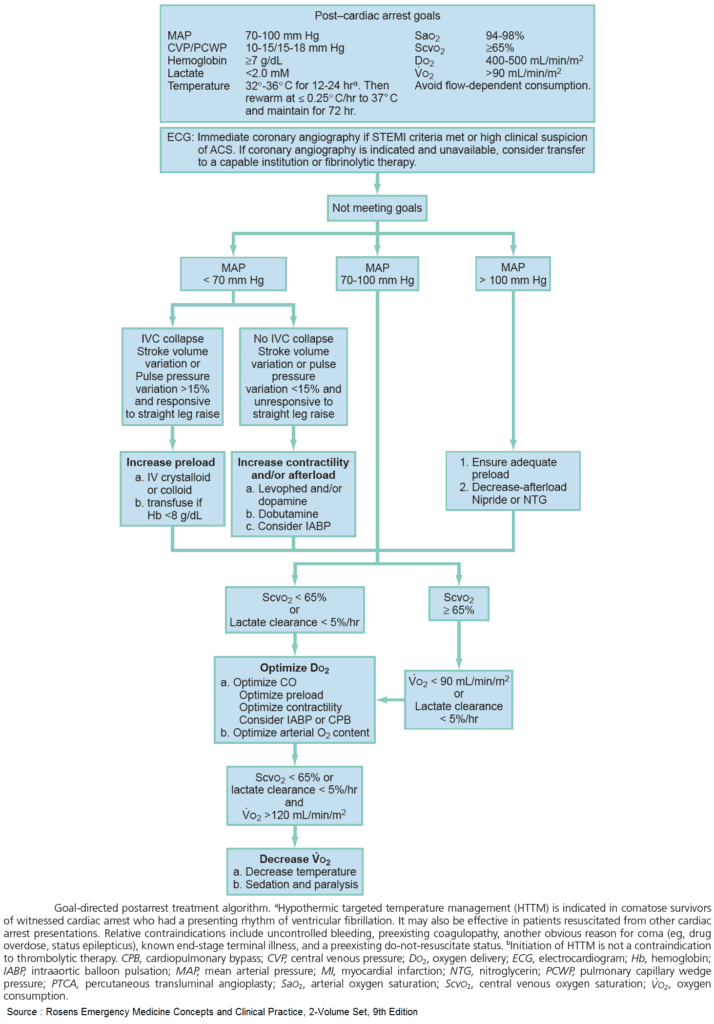
The first objective is to optimize cardiopulmonary function and, by consequence, end organ perfusion. Hypotension, typically defined as a meanarterial pressure (MAP) < 65 mm Hg or systolic blood pressure < 90 mm Hg, should be avoided. Starting with a crystalloid bolus is reasonable in all cases,although those who have arrested as a result of hemorrhage are likely tobenefit more from blood products. Vasopressors and inotropes should be added when hypotension persists. This scenario is more likely when impaired cardiac function (i.e., myocardial infarction, severe sepsis) is the likely primary etiology of the arrest.
Similarly, hypoxia should be avoided. If there is a concern for ongoing hypoxia and only a supraglottic ventilation strategy was employed, consider conversion to a definitive airway using an endotracheal tube. Place the patient on a ventilator with a full respiratory support, particularly if the patient is not following commands. With respect to oxygenation, start with a fraction of inspired oxygen (FiO2) of 100% and peak end-expiratory pressure (PEEP) of 5 mm Hg. Titrate to keep the oxygen saturation above 94% and perhaps not >98%. The upper parameter has no basis in the literature and only serves as a reminder of the danger of hyperoxia. The associated freeradical formation may worsen neurologic outcomes.
Either from chest compressions or as a result of the process that caused the arrest—or both—the patient may develop acute lung injury (PaO2/FiO2 < 300) or acute respiratory distress syndrome (ARDS, PaO2/FiO2 < 200).
Therefore, consider lung protective ventilation strategies. Specifically, the goal tidal volume should be 6 mL/kg of predicted body weight. Caution should also be taken against hyperventilation as it may decrease cerebral perfusion. In healthy brain tissue, one can expect a decrease in cerebral perfusion of 2% to 4% for every mm Hg decrease of PaCO2. Ventilation should be titrated to a goal PaCO2 of 40 to 45 mm Hg. It is important to remember that tachypnea may also be mediated by anxiety, pain, and/or agitation, which are all likely in the postresuscitated period. Consequently, analgesics and sedatives should be considered for patients who are not completely comatose.
Determine the Etiology
The second objective is to ascertain and treat the cause of the arrest, if it can be identified. This will typically involve a broad range of bedside, laboratory, and radiographic tests. Obtain an electrocardiogram (EKG) as soon as the patient is stabilized to look for signs of ischemic heart disease. Evidence of an acute coronary syndrome (ACS) should prompt consideration for immediate treatment, including percutaneous intervention. Fibrinolysis or embolectomy can be performed when pulmonary embolism is the suspected etiology of the arrest. The remainder of the “H’s and T’s” should be considered and addressed based on clinical scenario. They include hypoxia,
hypoglycemia, hyper-/hypokalemia, hydrogen ion (meaning acidosis of any etiology), hypovolemia, hypothermia, tamponade (pericardial), toxins, trauma, tension pneumothorax, and thrombosis, as discussed.
When ascertaining the cause of the arrest, consider whether an abnormal finding reflects the cause of the arrest or simply its sequela. For instance, severe acidosis—demonstrated by a high lactic acid, low pH, and low bicarbonate—may simply reflect the prolonged state of hypoperfusion rather than the etiology of the arrest. Therefore, treatment with a bicarbonate drip or with hyperventilation would not be appropriate; optimizing cardiopulmonary function and thus restoring perfusion would be expected to provide more benefit.
Optimize Neurologic Recovery
The third objective is to maximize the environment for neurologic recovery. The literature behind this is not as definitive, but there are certainly common practices that ought to be considered. Hypothermia is perhaps the most discussed therapy. While the literature is equivocal on its benefit with respect to normothermia, it is clearly favorable when compared to hyperthermia. Hyperthermia, which may be related to ambient temperature or release of inflammatory cytokines, has a deleterious effect on the brain and should be actively avoided. Cold crystalloid infusion and external cooling are typically effective, and more invasive measures are seldom required. A reasonable target temperature is 36°C as it is just as effective as 32°C and has fewer associated complications (i.e., infection, coagulopathy, and cold diuresis).
Hyperglycemia has also been found to be associated with poorer outcomes and worse neurologic recovery. Treating it, however, needs to be balanced against the more precipitous threat of hypoglycemia. As such, moderate glycemic control is typically preferred, usually defined as a glucose level between 144 and 180 mg/dL.
Routine administration of neuroprotective pharmacologics has not demonstrated clear benefit and should be avoided. This includes but is not limited to coenzyme Q10, corticosteroids, thiopental, and magnesium sulfate. The one possible exception is antiepileptic therapy as the harm of sustained epileptiform activity on brain tissue is clear. However, without an electroencephalogram, diagnosis of seizure is not easily made.
The ultimate disposition of the resuscitated patient postarrest is the intensive care unit. There, intensivists along with various other subspecialists can optimally manage the patient, hopefully affording him or her the best possible outcome. The patient’s family or other surrogate decision-makers should be involved early and often. As patients obtain ROSC and stay in the emergency department for at least a short period of time, it is the responsibility of the emergency medicine clinician to initiate the best possible postarrest care early on.
Key Points
- Perfusion should be maximized by focusing on cardiac output and tissue oxygenation.
- After ROSC is achieved, search for the underlying etiology of the cardiac arrest.
- Various approaches exist to maximize the most meaningful outcome, neurologic recovery.
- Care should be coordinated among various subspecialists as well as the patient’s family or other surrogate decision-makers.