Table of Contents
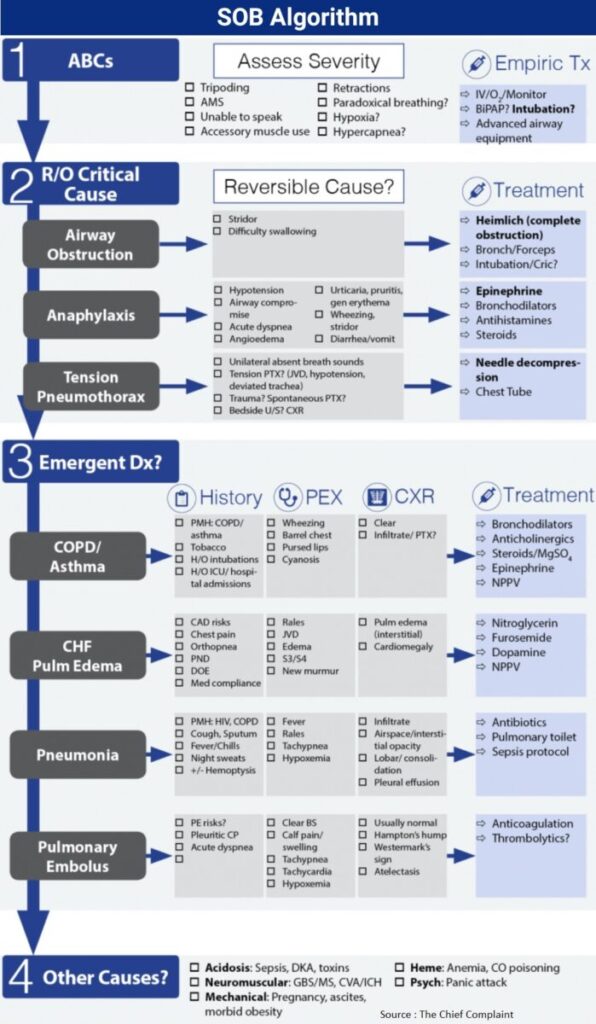
- Assess severity of dyspnea, including need for intubation/airway management based on physical examination
- Emergent intubation indicated regardless of cause if severe respiratory distress/arrest
- Consider Critical diagnoses → may be able to cure patient and avert intubation if the underlying cause is corrected (i.e. chest tube insertion, foreign body removal…)
- Then think of emergent diagnoses and begin specific treatment
ABCS: Emergent Rapid Sequence Intubation
Indication
- No absolute set criteria → decision to intubate based on physician assessment and comfort
- General Indications:
- Failure of Noninvasive Positive Pressure Ventilation (NPPV)
- Hemodynamic instability
- Patient fatigue
- Acute/progressive respiratory acidosis
- Hypoxia not responsive to supplemental oxygen
- Rapid decline in level of consciousness
RSI Steps
- Preparation
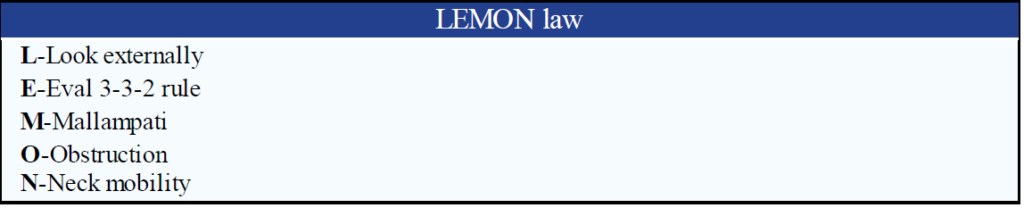
- Difficult airway?
- Use LEMON law, have back-up devices (LMA, bougie, cricothyrotomy kit) handy, check equipment, have drugs drawn up
- Failed airway algorithm: Difficult to intubate? Oxygenate and ventilate? Obtain a surgical airway?
- First pass success is goal, complication rate of 47% with second pass
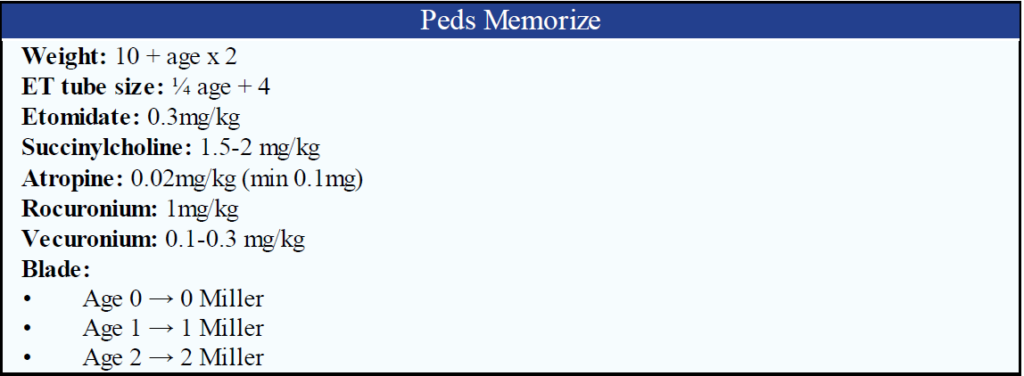
- ET tube size:
- Adult →usually 7.5 ETT
- Peds →[Age (years)/4] + 4
- Blade:
- Adult→usually Mac 4 (varies depending on comfort)
- Difficult airway?
- Pre-oxygenation
- Goal: establish O2 reservoir in lungs to prevent desaturation
- 100% O2 for 5 minutes or 8 Vital Capacity breaths
- Goal: establish O2 reservoir in lungs to prevent desaturation
- Pretreatment
- Goal: administer drugs to treat adverse effects associated with intubation, generally not used
- Lidocaine (1.5mg/kg IV) →for ↑ICP or reactive airway disease (controversial)
- Fentanyl (3mcg/kg IV) → for ↑HR or ↑BP in ICP, CAD, Aortic dissection, AAA
- Atropine (0.02mg/kg IV, minimum 0.1 mg) → Have at bedside or consider pretreatment in peds <1yr (controversial)
- Goal: administer drugs to treat adverse effects associated with intubation, generally not used
- Paralysis with Induction
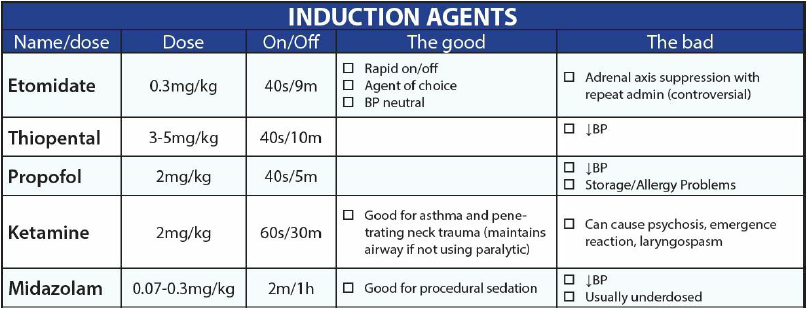
- Induction:
- Etomidate 0.3mg/kg IV
- Onset→20-30sec; Duration→ 7-14min
- Adverse effects: N/V, myoclonic activity, pain at injection site, adrenal insufficiency (controversial)
- Paralysis
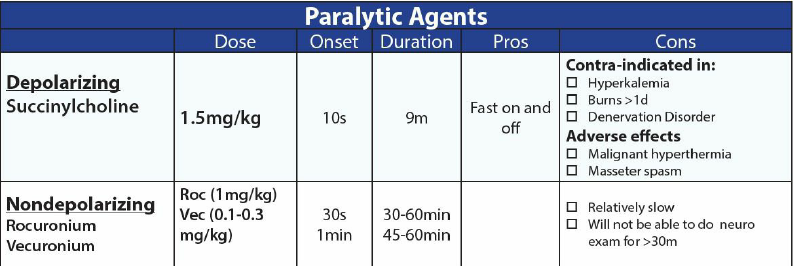
- Types: Noncompetitive depolarizing (succinylcholine) vs Competitive nondepolarizing (Rocuronium) neuromuscular blockers
- Succinylcholine
- i. Type: Noncompetitive Depolarizing
- ii. Dose: 1.5-2mg/kg IV
- iii.Onset → 45-60 sec; Duration →3-5min
- iv. Contraindications: Hyperkalemia, Hx malignant hyperthermia, Burn>24h,
- Crush/denervation > 7days, Neuromuscular disease
- Rocuronium,
- i. Dose: high dose 1mg/kg; Onset→60sec; Duration→40-60min
- Vecuronium
- i. Dose: 0.1 mg/kg vs high dose 0.3mg/kg: Onset →0-90sec; Duration → 100min
- Induction:
- Protection and Positioning
- Avoid BVM (unless hypoxic)
- Sniffing position (unless contraindicated →C-spine)
- External laryngeal manipulation to improve view of epiglottis/cords
- Placement and Proof
- EtCO2, Bilateral breath sounds, pulse oximetry, no gastric sounds, fog in ETT, US?
- Post-intubation management:
- Secure tube, sedation, Vent management, CXR, ABG
Critical Diagnoses
1. Airway Obstruction
Assessment
- Partial: Stridor, wheeze, SOB →assess cause and prepare for airway management
- Complete: chest movement without air movement → emergent intubation
- Clear obstruction immediately (complete obstruction)
- Heimlich maneuver (for complete foreign body obstruction)
- Forceps
- Bronchoscopy
2. Anaphylaxis
General
- Acute systemic allergic or hypersensitivity reaction that is rapid and may cause death
- Airway compromise:
- Upper airway → laryngeal edema
- Lower airway → bronchospasm
- Most commonly: Skin manifestations
- Other manifestations: Diarrhea (may be only presenting symptom)
- Cause: Unknown (40%), food (shellfish, peanuts), medication, blood products, latex
Presentation
- Skin: Flushing, urticaria, angioedema
- Eyes: Lacrimation, injection, edema
- Respiratory: Rhinorrhea, stridor, cough, wheeze
- CV: Tachycardia, hypotension, cardiac arrest
- GI: N/V, diarrhea
- CNS: Dizzy, syncope
Diagnosis
- Criteria 1: Acute skin/mucosa illness (hives, pruritis, flushing) + 1 of the following:
- Respiratory compromise (dyspnea, wheeze, bronchospasm, stridor, hypoxia)
- Reduced BP (SBP < 90 or end organ dysfunction → syncope, shock)
- Criteria 2: Exposure to LIKELY allergen + 2 or more:
- Skin-mucosa involvement
- Respiratory compromise
- Reduced BP
- Persistent GI symptoms (Intestinal anaphylaxis → vomiting, crampy abdominal pain)
- Criteria 3: Reduced BP after exposure to KNOWN allergen for patient
Treatment:
Read Also : Use of Epinephrine in Anaphylaxis
- General
- Speed of symptom progression determines severity of reaction
- Stop inciting agent (antibiotic, remove venom sac…)
- Epinephrine
- First line/Primary treatment for life threatening anaphylaxis!
- Indication:
- Laryngeal edema, severe bronchospasm, respiratory arrest, shock.
- NO absolute contraindications to Epi in Anaphylaxis
- Use with caution in CV disease, antidepressants (slow epi metab), recent surgery
- IM Dosing:
- Adult: 0.3-0.5ml of 1:1000 IM
- Peds: 0.01mg/kg of 1:1000 IM
- IM is route of choice: IM has shown better absorption and ↑plasma levels vs SC
- IV Dose:
- 0.1 mg IV = 100 mcg IV = 1ml of 1:10,000 (need to dilute to 10 or 100ml→ see below!)
- Dilution options:
- Option #1: add 1 ml of 1:10,000 epinephrine solution to 9ml NS →10 ml of 1:100,000 dilution (10mcg/ml) over 5-10 min →10-20mcg/min
- Option #2: add 1ml of 1:10,000 (crash cart epi) to 100ml NS (1mcg/ml) and run over 5-10min
- Pediatrics: 0.1 mcg/kg/min (diluted to 1:100,000 solution) and titrate to response
- Epinephrine gtt
- Same dilution as option #2 → (1mcg/ml), to run at 1-4 ml/min (1-4 mcg/min)
- Caution in elderly and cardiac disease
- Oxygen: 100% O2
- IV Fluids:
- May need large volume if persistently hypotensive
- Antihistamines:
- H1 blocker: Diphenhydramine 25-100 mg IV/SC/PO
- H2 blocker: Famotidine 20mg IV; Ranitidine 50mg IV or 150 mg po
- Steroids: Solumedrol 125 mg IV (2mg/kg)
- Special Case: Patient taking Beta-blockers?
- Glucagon 1- 3mg IV q 5min
- Special Case: Cardiac arrest
- Aggressive fluid resuscitation (4-8L)
- High-dose epinephrine (1mg → 3mg → 5mg)
- Usual care: Antihistamines IV, Steroids IV
- Prolonged CPR (anaphylaxis may resolve)
Disposition
- Minor allergic reaction (no hypotension/resp sx)
- Diphenhydramine, Prednisone 40-60mg x 5-7days, H2 blocker
- Consider observation x 4h?
- Be certain to discharge home with EpiPen x 2
- Severe Anaphylaxis: → ICU
- Anaphylaxis that resolves?
- Biphasic Reaction?
- Previously, incidence in literature between 3-20% ((Journal of Emergency Medicine 2005;28:381)
- Grunau et al, (Ann Emerg Med. 2014;63:736)
- Biphasic reaction only occurred in 0.18% of patients
- Bouncebacks are possible though (5.25% in 7 days)
- Conclusion:
- Biphasic reactions are rare and most anaphylaxis that resolves will unlikely need routine monitoring
- Consider admission for severe anaphylaxis, even if patient improves
- Consider admission vs observation, depending on severity
- D/C Plan:
- Reliable pt?
- H1/H2, Steroids
- EpiPen x 2
- Allergist/Immunologist f/u
- Biphasic Reaction?
3. Angioedema
General
- Incidence ~ 0.5%
- Almost always secondary to ACE Inhibitors.
- Not related to dose or frequency, can happen any time (even months to years after starting medication)
- Mechanism is bradykinin release (ACE-I inhibits bradykinin breakdown)
- Most commonly seen in African American
Treatment
- No proven benefit with Epi, H1/H2 blockers, or steroids
- Severe Angioedema
- Consider early intubation in patient with tongue involvement
- Prepare for nasotracheal intubation
- Fiberoptic laryngoscopic intubation (ENT vs anesthesia)
- Sedation: Ketamine
- Anticipate surgical airway
- Consider FFP (C1 esterase deficiency)
- 2-3 Units ASAP
- Case reports of effectiveness
- Minor lip edema
- Course is unpredictable; observe for 4-6 hours at least, consider admission
4. Tension Pneumothorax
Clinical Signs
- Unilateral absent breath sounds
- Beck’s triad (JVD, hypotension, deviated trachea)
- Trauma vs Spontaneous PTX?
Diagnosis
- US-look for sliding lung, comet tail
- CXR
Treatment-depends on severity and primary vs secondary
- Immediate needle decompression vs
- Chest tube vs
- Observation (O2, repeat CXR)
Emergent Diagnoses
1. Asthma
Assess severity of exacerbation
- Mild:
- Clinical: Dyspnea only with activity
- FEV1 or PEF >70% predicted
- Moderate:
- Clinical: Dyspnea interferes/limits activity
- FEV1 or PEF 40-69% predicted
- Severe:
- Clinical: Dyspnea at rest, interferes with conversation, accessory muscle use, chest retraction
- FEV1 or PEF <40% predicted
- Life threatening
- Clinical: Too dyspneic to speak, diaphoretic, no air movement, impending intubation
- PEF < 25% predicted
Medication
- β-agonists
- Mechanism of Action:
- Potent bronchodilators that act on β-receptors → relax bronchial smooth muscle
- Dosing
- Depending on patient severity, can be given as MDI, intermittent nebulizer or continuous nebulizer
- Albuterol 2.5-5mg nebulizer q 20min x3 in 1st hour or can use MDI
- Journal club
- Cochrane review: (Cochrane Database Syst Rev 2009:CD001115)
- Continuous nebs better than intermittent nebs for preventing hospital admission (NNT =10)
- Cochrane review: (Cochrane Database Syst Rev 2009:CD001115)
- Mechanism of Action:
- Anticholinergics
- Mechanism of Action:
- Decrease vagally mediated smooth muscle contraction in the airways → bronchodilation
- Works synergistically with β-agonists
- Dose:
- Ipatropium 0.5mg q 20min x 3 in 1st hour or MDI
- Usually given concomitant with Albuterol
- Journal Club:
- Cochrane review: (Cochrane Database Syst Rev 2008:CD000060)
- i. Anticholinergics decreased hospital admission by 25%
- ii. NNT = 12 to prevent hospital admission
- Cochrane review: (Cochrane Database Syst Rev 2008:CD000060)
- Mechanism of Action:
- Steroids
- Indication:
- Moderate or severe asthma
- β-agonists do not fully correct the decline in pulmonary function
- Dosing
- PO:
- i. Prednisone 40-60 mg po (1-2 mg/kg)
- ii. PO preferred and equivalent to IV, if patient is able to tolerate
- iii. Continue steroids x 5-7 days if d/c
- IV:
- i. Indication: Moderate/severe asthma or not tolerating po
- ii. Dose: Methylprednisolone 40-125mg IV
- IM: IM steroids just as effective as IV (Chest 2004;126(2):362)
- PO:
- Journal club
- Cochrane review: (Cochrane Database Syst Rev 2001;1:CD002178)
- i. Decreased hospital admission if steroids given within 1 hour of ED presentation
- ii. Absolute risk reduction 12.5% (NNT = 8)
- Cochrane review: (Cochrane Database Syst Rev 2001;1:CD002178)
- Indication:
- Magnesium sulfate
- Mechanism of Action:
- Inhibits the influx of calcium into smooth muscle cells → causing bronchodilation
- Dosing: MgSO4 2g IV over 15 min
- Indication
- Life-threatening exacerbations or
- If the exacerbation remains severe (PEF <40%) after 1 hour of conventional therapy
- Journal club
- Cochrane review: (Cochrane Data- base Syst Rev 2009:CD001490)
- MgSO4 significantly improved pulmonary function and ↓admission rates for severe asthma
- Meta-analysis (Ann Emerg Med 2000;36(3):18)
- i. Improvements seen only in severe asthma exacerbation subgroups
- ii. Severe asthma: ↓Admission rates and improved pulmonary function (PEFR and FEV1)
- Cochrane review: (Cochrane Data- base Syst Rev 2009:CD001490)
- Mechanism of Action:
Treatment (aggressiveness depends on severity)
- Mild (Tune up and go home?)
- O2 for hypoxia, all patients
- β-agonists
- Albuterol (2.5-5mg nebulizer q 20min x3 in 1st hour) or MDI
- Anticholinergics
- Ipatropium 0.5mg q 20min x3 in 1st hour) or MDI
- Steroids
- Prednisone 1-2mg/kg po (Solumedrol if not tolerate PO), continue x 5-7days
- Moderate (“They look kinda bad”)
- Albuterol/Ipatropium continuous nebulizer
- Steroids: Solumedrol 2mg/kg (125mg) IV q6
- Magnesium sulfate 2g IV over 15 min
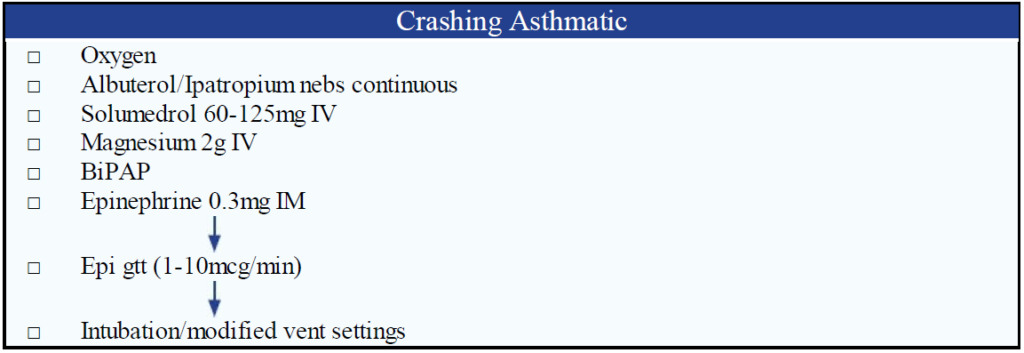
- Severe (Status Asthmaticus)
- General: impending intubation, need maximal therapy to prevent intubation because of ↑risk of lung injury with ventilation
- Moderate therapies +
- Epinephrine
- IM: 0.3mg IM or
- Terbutaline 0.25mg SC q 20min x 2
- Caution in elderly, cardiac disease
- Epinephrine gtt:
- 2.5 mls of 1:10,000 epi in 250mlNS (1mcg/ml) and run over 25 min (10mcg/min)
- Epinephrine IV:
- 0.25ml of 1:10,000 and flush (25mcg)
- Heliox:
- 80:20 or 70:30 helium to oxygen ratio used
- Questionable efficacy, worth trying
- BiPAP:
- Reduces work of breathing and need for intubation
- Start low and titrate up: IPAP 7-15, EPAP 3-5
- Ketamine – consider sub dissociative dose 0.1-0.5 mg/kg
- Intubation (goal is to prevent intubation)
- RSI: ketamine vs etomidate? awake-nasal vs oral intubation
- Most experienced practitioner, patients desaturate rapidly
- Pretreatment with lidocaine to reduce bronchospasm is not proven therapy
- Ventilator strategies:
- General
- Prolong expiratory time, avoid barotrauma
- Do not hyperventilate →breath stacking, barotrauma, ptx, ↓venous return, cardiac arrest
- Settings:
- PRVC, RR: 6-8, Vt: 5-7ml/kg; Insp flow: 100l/min; PEEP : 5; I:E ratio: 1:3- 4
- Keep Pplat <35 and auto-peep <15
- Sedation (ketamine, lorazepam) and paralysis (Vecuronium, but try not to re-paralyze)
- Complications
- Barotrauma, PTX, Cardiovascular collapse
- Hypotension/Arrest →disconnect from vent & push on chest →forced expiration, IVF bolus, bilateral chest tubes?
- General
2. COPD Exacerbation
General
- Definition: Acute worsening of symptoms including cough, wheeze, SOB, sputum production and fever
- “Characterized by a worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication” (GOLD 2014)
Cause
- Infection (bacterial, viral, both)
- Airway inflammation from non-infectious source (air pollution, occupational)
- Alternative pathology (PTX, PE, CHF, mucus plug, anxiety/depression, cold)
- Unknown in 1/3 of cases
Diagnosis
- COPD diagnosis:
- Clinical Sx: chronic cough, chronic sputum production, dyspnea at rest or with exertion
- Physical exam: Cyanosis, barrel chest, pursed lip breathing, wheezing, right heart failure
- History of COPD risk factors (exposure to tobacco smoke, occupational dust, and chemicals)
- Acute exacerbation of COPD
- Increasing dyspnea, worsening exercise tolerance, worsening sputum purulence, and
- increased sputum production in a patient with known or likely COPD
Work-up
- ABG
- Guidelines recommend ABG for mod/severe exacerbation, SaO2 < 92% follow pH, PO2 and PCO2 before and after NPPV/intubation (GOLD 2014)
- Caution with ABGs: painful, associated with complications and often not necessary
- EKG: Rule out ischemia/arrhythmia and evaluate for right heart strain/hypertrophy
- CXR:
- Evaluate for cause, alternative diagnosis and complication (ie PTX) of COPD
Treatment
- Similar to asthma exacerbation (see above)
- Oxygen
- Judicious use to keep SaO2 88-92%
- ↑O2 causes CO2 retention and respiratory acidosis → cardiac depression (arrhythmias) and neurologic depression (AMS)
- Increased mortality with high flow O2 in COPD patients (BMJ. 2010 Oct 18;341:c5462)
- Mortality 9% (high flow O2) vs 4% (O2 titrated to SaO2 88-92%)
- Bronchodilators
- ß-agonist (Albuterol)
- First line therapy (used for the reversible component of COPD)
- MDI and nebulizer equivalent efficacy
- Anticholinergics (Ipatropium)
- Combination with ß-agonist shown superior to either alone
- ß-agonist (Albuterol)
- Steroids
- Improves PaO2, FEV1, dyspnea improvement and ↓relapse
- Journal club (Cochrane Data- base Syst Rev 2009;1:CD001288)
- Cochrane review: Steroid use resulted in decreased treatment failures, shorter hospitalization and improved pulmonary function
- NNT = 10 to avoid treatment failure
- Antibiotics
- ↑resolution of symptoms
- Indication: (GOLD 2014)
- COPD exacerbation with 3 cardinal symptoms (↑dyspnea, ↑sputum volume, ↑purulence)
- Only 2 cardinal symptoms if one of them is ↑purulence
- Mechanical ventilation (NPPV/Invasive)
- Antibiotic choice (empiric)
- Mild exacerbation: β-lactam, Tetracycline or TMP/SMX
- Moderate: β-lactam/ β-lactamase inhibitor
- Severe: Fluoroquinolone
- Journal club
- Cochrane review (Cochrane Database Syst Rev. 2012;12:CD010257)
- Antibiotics reduced treatment failure in severe exacerbations/ICU patients
- Magnesium sulfate (MgSO4)
- Improves pulmonary function in severe exacerbations
- NPPV
- Benefit: better outcome, ↓intubation rates, ↓mortality rates, ↓hospital stay
- Indications: mod/severe dyspnea, respiratory acidosis, ↓oxygenation,
- Contraindications: respiratory arrest, medically unstable, unable to protect airway, ALOC, ↑secretions, improper fit of mask
- Journal club Cochrane review (Cochrane Database Syst Rev 2004;3)
- NPPV resulted in ↓mortality (NNT = 10)
- Decreased need for intubation (NNT = 4)
- Reduction in treatment failure (NNT = 5)
- Mechanical ventilation
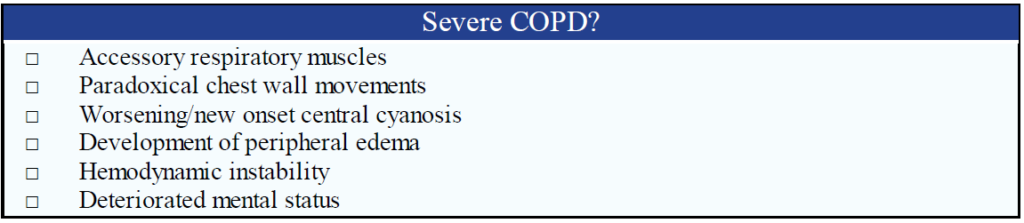
- Indications:
- Failed/not tolerate NPPV
- Hypoxia
- Resp failure (PCO2 > 60; pH < 7.25; RR > 35; )
- Respiratory arrest
- Somnolence, AMS
- Other complications (Shock, sepsis, pneumonia, metabolic abnormalities)
- Technique
- Pre-oxygenate to 100%
- Pt can desaturate quickly
- Use NPPV with increased settings
- Delayed sequence intubation?
- Use in pt with AMS/combative and unable to pre-oxygenate
- Consider Ketamine for sedation prior to intubation to assist in oxygenation?
- Nasal canula with ↑O2 flow before and during intubation
- IVF: NS bolus to avoid peri-intubation hypotension
- Pre-oxygenate to 100%
- Ventilator strategy
- Avoid DHI (Dynamic hyperinflation)
- COPD pts require prolonged expiratory time to exhale all air
- If next breath given too soon before lungs fully evacuated → breath stacking → DHI
- DHI causes ↑intra-thoracic pressure → hypotension → obstructive shock → PEA arrest
- DHI can also cause barotrauma (PTX, pneumomediastinum, etc.)
- Ventilator settings
- PRVC, RR: 6-8, Vt: 5-7ml/kg; Insp flow: 100l/min; PEEP:5; I:E ratio: 1:3-4
- Permissive hypercapnea
- Vent settings lead to ↓ventilation → ↑CO2 → Acidosis
- Can allow pH to go down to 7.15
- May need to give supplemental HCO3 (controversial)
- Need adequate sedation to avoid barotrauma and over breathing ventilator
- Measure DHI
- Auto-PEEP:
- i. Elevated alveolar pressure at end of expiration
- Plateau pressure
- i. Airway pressure during inspiratory pause
- ii. DHI = Plateau pressure > 30 cm
- Auto-PEEP:
- DHI Treatment (emergent)
- Bronchodilators, sedation, ↓RR, ↓TV
- Disconnect from ventilator and manually squeeze chest to decompress
- Check for tension PTX
- Avoid DHI (Dynamic hyperinflation)
- Indications:
3. Congestive Heart Failure
General
- Causes (acute exacerbation): Arrhythmia, MI, medication non-compliance, PE, pneumonia, pleural effusion, acute valvular emergency
Presentation
- History/Physical
- History: Orthopnea, PND, dyspnea
- Physical: Rales, S3, JVD, increased body weight, pitting edema, wheezing (cardiac asthma), tachycardia, hypotension, new onset murmur (valvular emergency)
- CXR
- Findings
- ✓ Pulmonary edema, cardiomegaly, Kerley B lines
- ✓ Cephalization, interstitial edema, alveolar edema (highly specific findings)
- Normal CXR does not exclude acute CHF (Ann Emerg Med. 2006;47:13)
- ✓ Almost 20% of patients in one series had CHF with a negative CXR (sensitivity 81%)
- Rule out other conditions: Pneumonia, pneumothorax etc.
- Findings
- EKG
- R/O ischemia, infarction, arrhythmia (e.g. atrial fibrillation), and LVH
- Labs
- Troponin elevated from acute injury/ischemia or increased LV pressures causing demand ischemia
- BNP (Circulation 2002;105:2328)
- BNP < 100 pg/ml essentially rules out CHF
- BNP > 400 pg/ml rules in CHF
Special Case: “Flash” pulmonary edema
- Define: Rapid increase in fluid in pulmonary alveola or interstitium
- Cause: Acute ischemia, hypertensive crisis, acute severe MR, stress induced (takotsubo) cardiomyopathy, bilateral renal artery stenosis (Pickering syndrome)
- Treatment: Similar to Acute CHF, except must treated quicker
Treatment
- Oxygen:
- Correct hypoxia
- Nitrates
- 1st line therapy→↓preload, ↓afterload, ↑CO
- Use: only in hypertensive/normotensive patients
- Nitroglycerin dose:
- Mild: PO, SL→ 400 mcg
- Moderate: 1-2 inches trans-dermal
- Severe: IV gtt→ start at 10mcg/min and titrate up quickly to 200-250 mcg/min
- Caution in preload dependent states: RV infarct, PDE-5 inhibitors (Sildenafil)
- Adverse effects: hypotension, headache, tolerance
- Diuretics:
- Dose:
- Furosemide (20-100 mg IV, equal to or greater than maintenance dose up to 2x maintenance)
- Mechanism of Action: Decrease preload → diuretic effect
- However pulm edema pts have ↓renal blood flow → leads to delayed effect (30-120min)
- Fluid restriction on arrival if hyponatremic (<130 meq/L)
- Caution: severe hypotension, shock
- Dose:
- Morphine:
- Use: decrease preload (histamine effect)?, anxiolysis
- Do not use to treat CHF (little evidence, may increase morbidity/mortality)
- Positive Inotropes
- Use: avoid if possible (JAMA. 2002;287(12):1541)
- Use only for cardiogenic shock or severe hypotension
- Bridge therapy until cath lab
- Increases incidence of arrhythmias, hypotension, and VT
- Use: avoid if possible (JAMA. 2002;287(12):1541)
- NPPV (CPAP, BiPAP)
- Mechanism of Action: ↓preload (increases intrathoracic pressure), ↓Work of breathing (WOB), improves gas exchange, ↓afterload
- Decreases need for intubation, ↓Length of stay (LOS)
- Journal Club: 3CPO Trial (N Engl J Med 2008;359:142)
- No mortality difference between O2 and NPPV
- NPPV associated with improvement (at 1h) in dyspnea, HR, acidosis, and hypercapnea
- ACE-Inhibitors
- Mechanism of Action: Downregulate RAA system, ↓adrenergic tone, improve LV relaxation→ ↓preload and afterload
- Use: Early initiation on ACE-I in CHF not recommended, avoid in hypotension
- No good comparisons to nitrates
- Dose: Captopril 25mg SL (12.5mg if SBP<110) or Enalaprilat 0.625-1.25mg IV Intubation/Vent
- Indication: Hypoxia SaO2 <90%, unable to tolerate NPPV
- Cardiogenic Shock
- SBP ≈ 90 → Dobutamine 2-3 mcg/kg/min
- SBP < 70 → Dopamine (5mcg/kg/min and ), if fails→Intra-aortic balloon pump, ultrafiltration, NE gtt
- Treatment algorithm
- NTG→ 1st line agent (IV NTG excellent single agent)
- NPPV→ 1st line agent for severe CHF (use early and often)
- Furosemide → 2nd line agent (AFTER preload and afterload reduction)
- ACE-I → 2nd line agent
- Do not use: β-blockers, morphine, Nesiritide
4. Pneumonia
Classical Presentation
- Typical pneumonia
- Most common organism: S. pneumoniae (60%)
- Presentation: High fever, rigors, cough with rust-colored sputum, leukocytosis
- CXR: lobar consolidation
- Atypical pneumonia
- Organisms: Mycoplasma, Legionella, and Chlamydophila
- Presentation: more gradual onset, dry cough, well appearing, ambulatory
- CXR: interstitial pattern
Classification
- Community Acquired Pneumonia (CAP)
- Definition:
- Acute infection of pulmonary parenchyma, occurring outside the hospital, with clinical symptoms accompanied by the presence of an infiltrate on CXR
- Patient has not been hospitalized or in a nursing home in the previous 14 days
- Organisms
- Streptococcus pneumoniae, Mycoplasma pneumoniae, Hemophilus influenzae, Clamydophilia sp, and viruses
- Definition:
- Hospital Acquired Pneumonia (HAP)
- Define
- New respiratory infection that presents > 48 hours after hospital admission
- Organisms
- Pseudomonas, MRSA, Legionella, Klebsiella, H influenzae, Moraxella catarrhalis
- Define
- Ventilator Associated Pneumonia (VAP)
- Define
- Pneumonia diagnosed > 48 hours after a patient has been intubated on ventilator in the ICU
- Organisms
- Pseudomonas, MRSA, Legionella, Klebsiella, H influenzae, Moraxella catarrhalis, Acinetobacter
- Define
- Health-Care Associated Pneumonia (HCAP)
- Define:
- Pneumonia in patients hospitalized for 2 or more days in the previous 90 days
- Includes dialysis, chemotherapy, chronic wound care, home IV antibiotics, immunocompromised and patients from nursing home facilities
- Organisms
- Pseudomonas, MRSA, Legionella, Klebsiella, H influenzae, Moraxella catarrhalis
- Define:
Work-up
- Labs (CBC, BMP, lactate etc.)
- Blood Cultures
- Studies show consistent low sensitivity and results do not alter management
- ACEP Guidelines: “Do not routinely obtain blood cultures in patients admitted with CAP”
- IDSA/ATS recommend blood cultures in the following:
- Admission to the intensive care unit
- Cavitary infiltrates
- Leukopenia
- Chronic severe liver disease
- Asplenia
- Pleural effusion
- A positive pneumococcal urinary antigen test
- Active alcohol abuse
- Sputum culture (Clinical Infectious Diseases 2007; 44:S27–72)
- Recommended in:
- ICU admission;
- Failure of outpatient antibiotic management
- Cavitary infiltrates
- Active alcohol abuse
- Severe obstructive or structural lung disease
- Positive Legionella urinary antigen test (UAT)
- Positive pneumococcal UAT
- Pleural effusion
- Recommended in:
- CXR
- Standard used to make diagnosis of pneumonia and r/o other pathology
Antibiotics
- Empiric antibiotics based on pneumonia classification, severity of illness and most likely organisms
- Outpatient
- Healthy, no risk factors:
- Macrolide or
- ✓ Doxycycline
- Comorbidity:
- Respiratory fluoroquinolone or
- β-lactam plus macrolide
- Healthy, no risk factors:
- Inpatient Ward
- Respiratory fluoroquinolone or
- β-lactam plus macrolide
- Inpatient ICU
- Minimum treatment:
- β-lactam plus macrolide
- Antipseudomonal coverage:
- Antipseudomonal β-lactam (piperacillin-tazobactam, cefepime, imipenem, or meropenem) plus either
- i. Ciprofloxacin or levofloxacin (750-mg dose) or
- ii. Aminoglycoside and azithromycin or
- iii. Aminoglycoside and a respiratory fluoroquinolone
- Antipseudomonal β-lactam (piperacillin-tazobactam, cefepime, imipenem, or meropenem) plus either
- CA-MRSA coverage (consider)
- Add vancomycin or linezolid
- Minimum treatment: