Table of Contents
Thyroid storm is an extreme version of hyperthyroidism with a mortality rate that approaches 30%, even with treatment. The recognition and management of thyroid storm can be difficult in the emergency department (ED).
Often, patients present with nonspecific symptoms that can easily be misdiagnosed as more common ED conditions (i.e., sepsis).
Physiology
Recall that the pituitary gland secretes thyroid-stimulating hormone (TSH), which prompts the thyroid gland to secrete thyroid hormone. Most thyroid hormone is released from the thyroid gland as thyroxine (T4), the physiologically inactive form, while the remainder is released as triiodothyronine (T3), the active form.
T4 is converted to T3 in the peripheral tissues. When enough thyroid hormone is present, further release of TSH is inhibited. Under normal circumstances, this feedback mechanism remains in balance. When this balance becomes interrupted, the thyroid gland can become over- or underactive.
Symptoms and Signs of Thyroid Storm
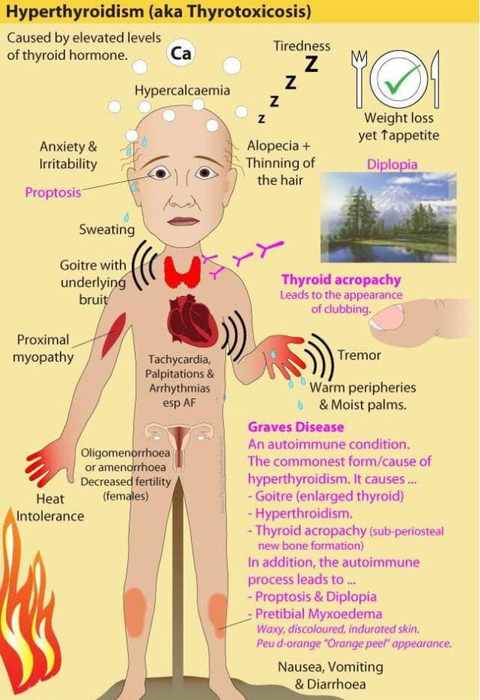
Thyroid storm typically presents with:
- Elevated Temperature
- Hypertension
- Tachycardia (often beyond that expected for the elevated temperature)
- Altered sensorium (hyperactivity and can vary anywhere from feelings of anxiety to coma)
- Tremors
- Diaphoresis
- Thinning hair
- Exophthalmos
- Goiter
- Signs and symptoms of high-output Congestive Heart Failure, such as pulmonary edema, jugular venous distention, and increased dyspnea on exertion.
These signs and symptoms can be easily overlooked, especially in the evaluation of a patient with vague complaints. Some would call thyroid storm the “great imitator,” as it can present similarly to other more common ED diagnoses.
Diagnosis of Thyroid Storm
The diagnosis of thyroid storm should be based on the clinical presentation. Scoring tools for thyroid storm have been published, but no tool has been shown to be superior and these tools are not commonly utilized in the ED. The diagnosis is confirmed with thyroid function testing; TSH, free T3, and free T4 levels should be obtained.
Patients with thyroid storm usually have a low TSH level and elevated T3, T4, or both. Though exceedingly rare, a TSH-producing tumor can demonstrate a normal, or elevated, TSH level in conjunction with a high T4 and T3. This tumor should be considered in patients with these lab findings and signs and symptoms of thyrotoxicosis.
Management of Thyroid Storm
The ED management of thyroid storm includes:
- Decreasing circulating thyroid hormone levels
- Reducing the effects of thyroid hormone
- Treating the presumed etiology
- Providing supportive care
These treatment steps should be initiated prior to the results of confirmatory laboratory tests in patients with thyroid storm.
Medications used in Thyroid Storm include:
- Beta Blockers
- Nondihydropyridine calcium channel blockers
- Antithyroid medications:
- Propylthiouracil (PTU)
- Methimazole
- Iodine
- Glucocorticoids
Beta Blockers and Calcium Channel Blockers
Initial management begins with the administration of beta-blocker medications. During thyroid storm, there is an increased expression of beta1-adrenergic receptors, which results in many of the clinical manifestations. Though any beta-blocker can be used, propranolol is generally the medication of choice, as it also blocks the peripheral conversion of T4 to T3.
The emergency provider should target a heart rate <100 bpm with the use of a beta-blocker agent. Heart rate control will also improve hemodynamics in patients with high-output heart failure due to thyroid storm.
If patients are intolerant to beta-blockers, nondihydropyridine calcium channel blockers may be used with similar efficacy. Importantly, these agents will not block the peripheral conversion of T4 to T3.
Antithyroid Medications
Antithyroid medications (i.e., thionamides, iodine) should be administered after a beta-blocker agent has been given. The thionamides, propylthiouracil (PTU) and methimazole, block new thyroid hormone synthesis and should be administered before iodine. Both are administered orally and have been shown to be equally effective. Similar to propranolol, PTU blocks the peripheral conversion of T4 to T3.
Iodine will further inhibit thyroid hormone synthesis but should be given at least 1 hour after the administration of a thionamide medication. If iodine is administered before a thionamide agent, it will provide substrate for new hormone synthesis and increase hormone levels.
Glucocorticoids
Lastly, glucocorticoid medications block the peripheral conversion of T4 to T3 and should be administered to patients with life-threatening features of thyroid storm.
Temperature Management
A critical component in the ED treatment of thyroid storm is temperature management in the setting of fever. A common pitfall is to provide active cooling through the use of cooling blankets, cooled intravenous fluids, and ice packets. However, active cooling methods are contraindicated in thyroid storm. Active cooling will precipitate peripheral vasoconstriction and can worsen hypertension.
Temperature management in thyroid storm should consist only of passive cooling techniques, such as a reduction in room temperature and the removal of clothing.
Key Points
- Consider thyroid storm in the patient with altered mental status and fever.
- Begin treatment for thyroid storm while awaiting confirmatory lab test results.
- Propranolol is the recommended beta-blocker agent of choice and can inhibit the peripheral conversion of T4 to T3.
- Provide iodine therapy at least 60 minutes after the administration of PTU or methimazole.
- Passive cooling is the preferred method for temperature management in patients with thyroid storm.