Table of Contents
Thyrotoxicosis results from an excess of circulating free T4 and free T3. It affects about 10 in 1000 women and 1 in 1000 men. Hyperthyroidism indicates thyroid gland overactivity, resulting in thyrotoxicosis.
Etiology of Hyperthyroidism
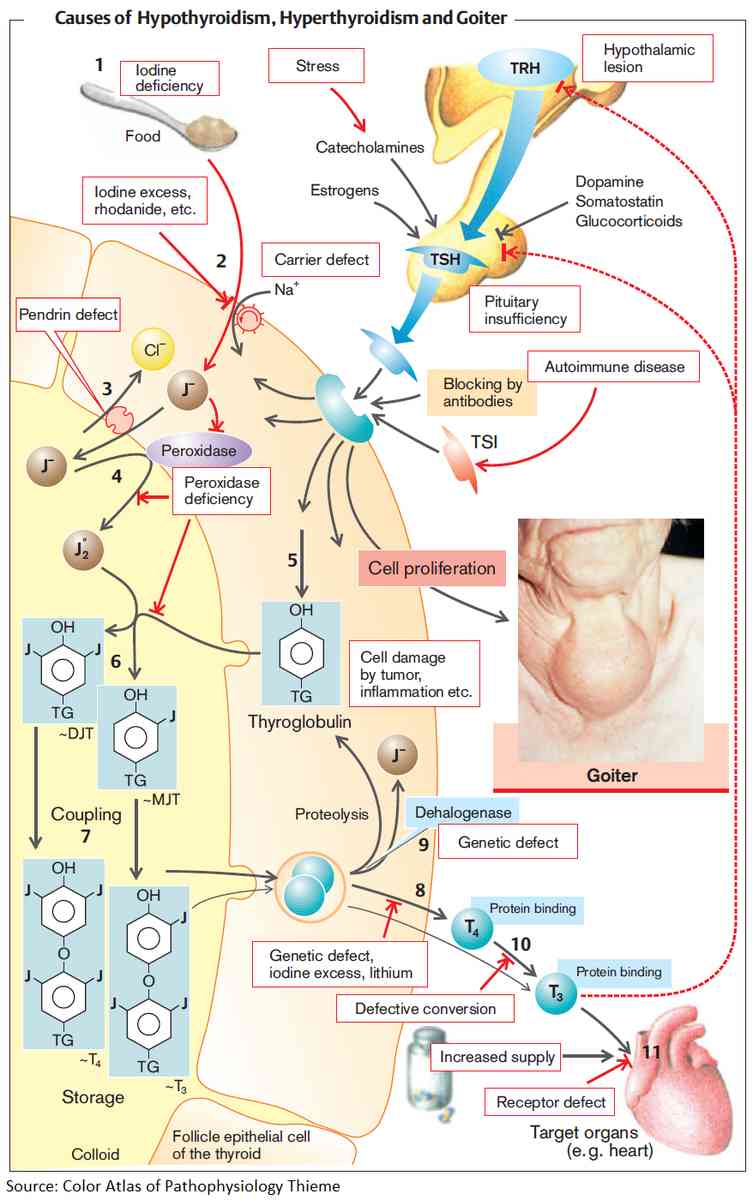
1. Primary Hyperthyroidism
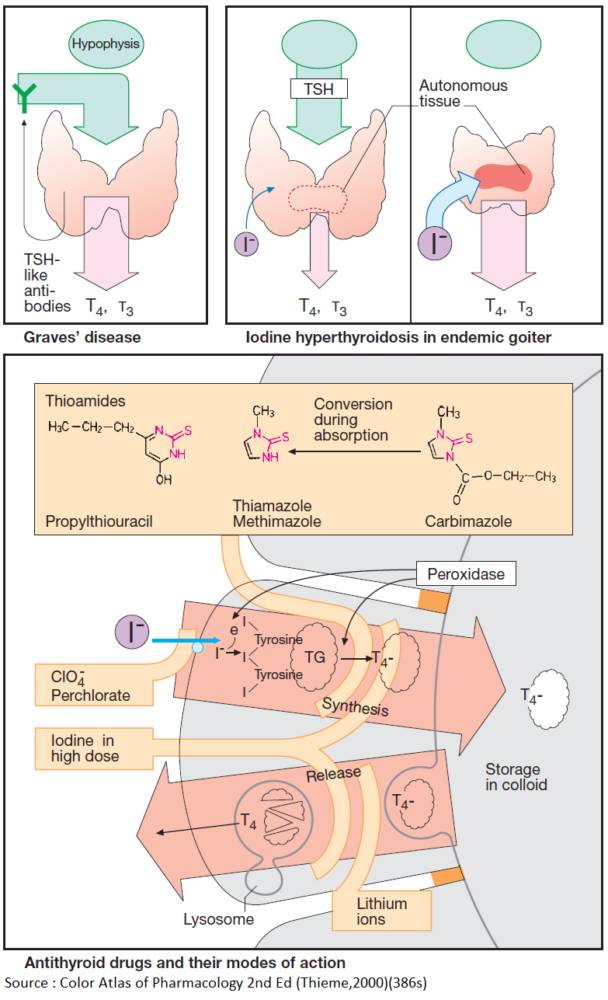
Graves’ Disease
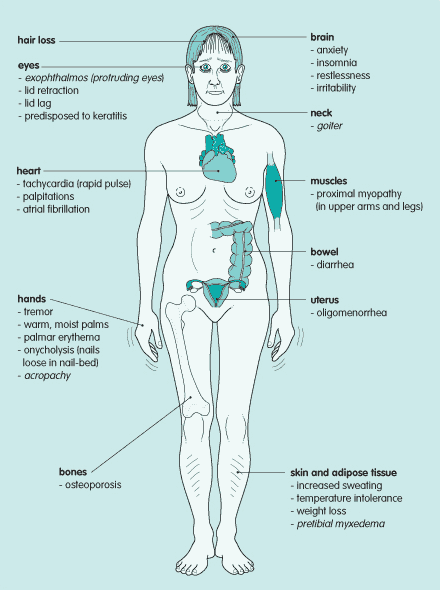
This accounts for 70-80% of all cases of hyperthyroidism. It is caused by the production of autoantibodies that stimulate the TSH receptor. There is a painless diffuse goiter in more than 90% of patients. In addition to the general features of thyrotoxicosis, pathognomonic features include ophthalmopathy, pretibial myxedema, and thyroid acropachy.
The ophthalmopathy includes grittiness and increased tear production, periorbital edema, conjunctival edema (chemosis), proptosis, diplopia, impaired visual acuity, and corneal ulceration. It is clinically obvious in 60% of patients with Graves’ disease but subclinical ophthalmopathy can be detected in more than 90% by CT scan or MRI, revealing fusiform enlargement of the extraocular muscles caused by lymphocytic infiltration, edema, and later fibrosis.
Pretibial myxedema occurs in 1-5% of patients with Graves’ disease and comprises of painless thickening of the skin in nodules or plaques, generally over the shin.
Thyroid acropachy occurs in less than 1% of patients and resembles finger clubbing.
Other causes of primary hyperthyroidism
- Toxic multinodular goiter and toxic adenoma account for most of the remaining causes
- Metastatic thyroid cancer
- Genetic causes such as the McCune-Albright syndrome and TSH receptor mutations
- Ectopic thyroid tissue (e.g., struma ovarii)
2. Secondary Hyperthyroidism
This is very uncommon. Causes include:
- Pituitary adenoma-secreting TSH,
- Trophoblastic tumors secreting human chorionic gonadotrophin
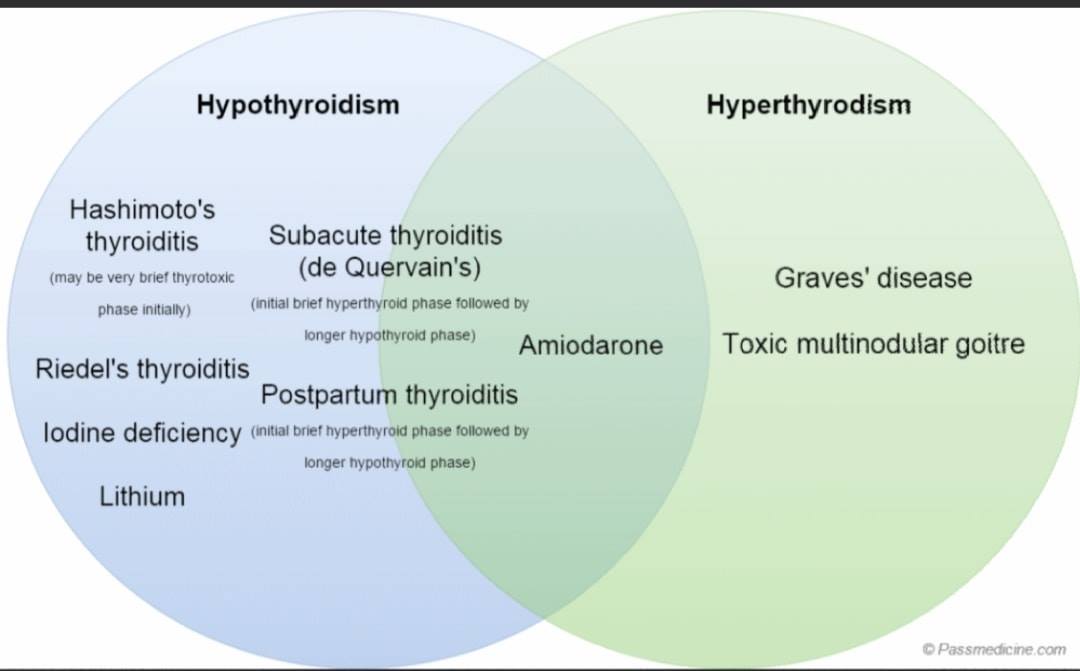
3. Thyrotoxicosis without hyperthyroidism
This may occur with:
- Destructive thyroiditis, such as in postpartum thyroiditis
- Subacute (de Quervain’s) thyroiditis
- Amiodarone-induced thyroiditis, and with
- Excessive thyroxine administration, or self-administered thyroxine, particularly in doctors and nurses
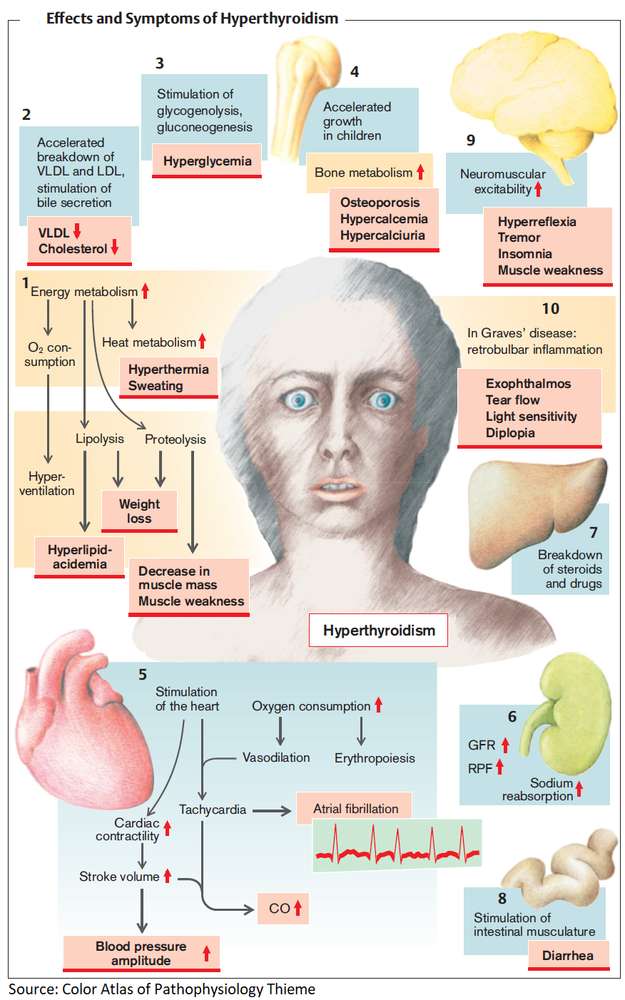
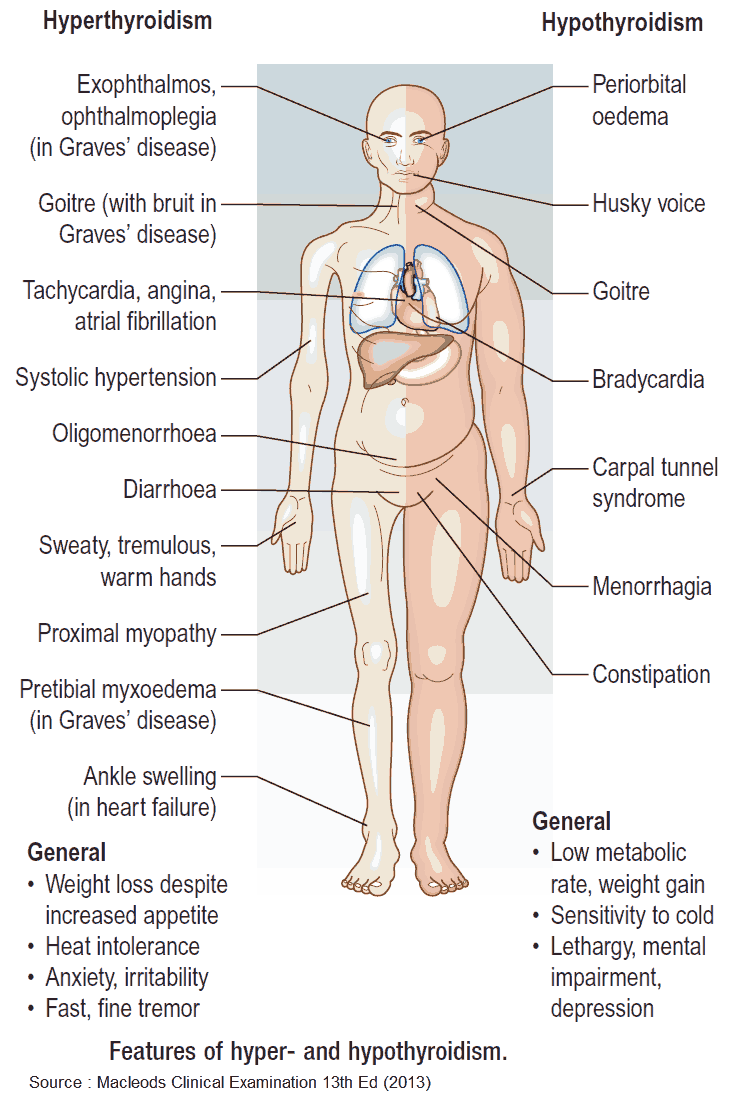
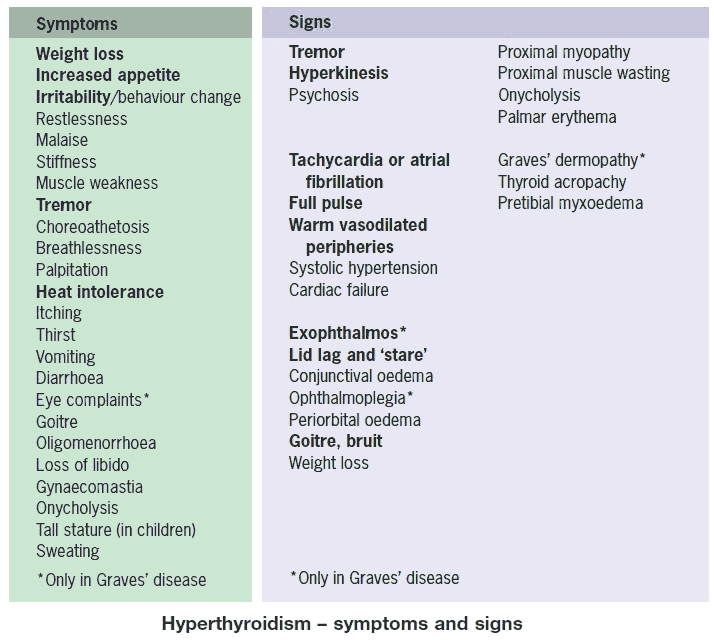
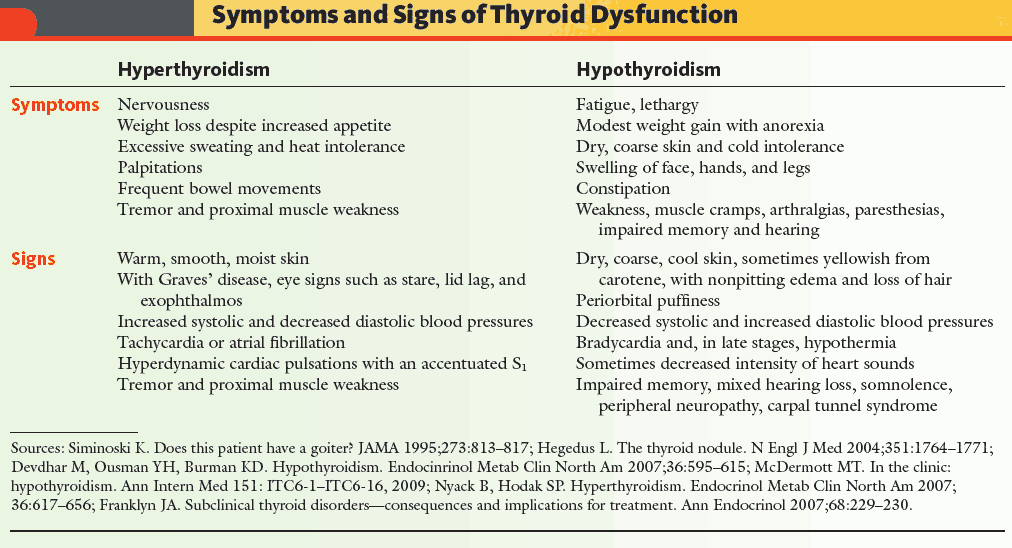
Clinical Presentation of Hyperthyroidism
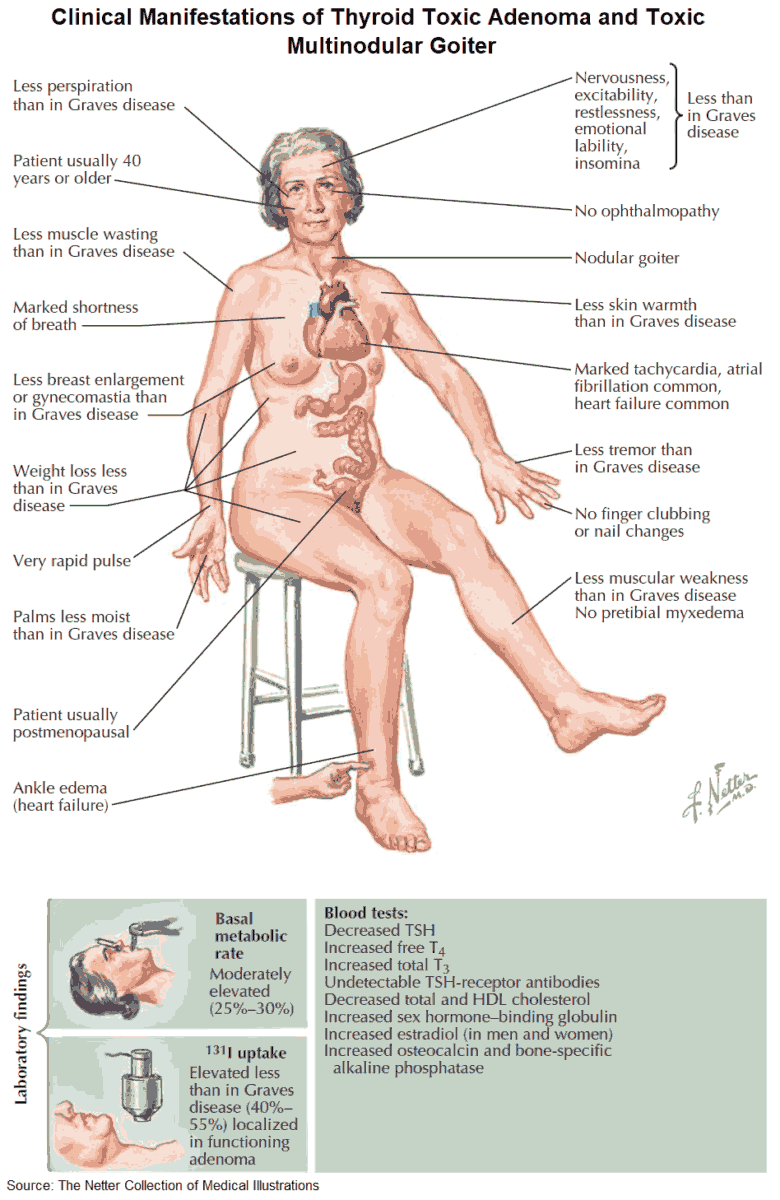
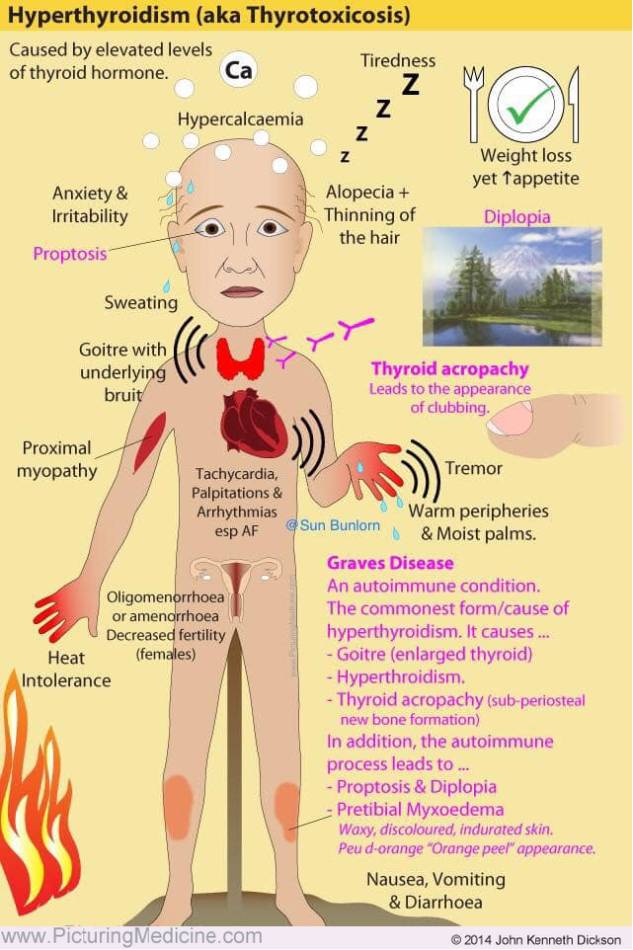
General symptoms include:
- Weight loss.
- Increased appetite.
- Heat intolerance and sweating.
- Fatigue and weakness.
- Hyperactivity, irritability.
- Tremor.
- Depression.
- Oligomenorrhea.
- Pruritus.
- Diarrhea.
- Polyuria.
Signs include:
- A goiter, possibly with a murmur over it.
- Tremor.
- Tachycardia and atrial fibrillation.
- Warm moist skin.
- Lid retraction and lid lag.
- Muscle weakness.
- Proximal myopathy.
- Cardiac failure.
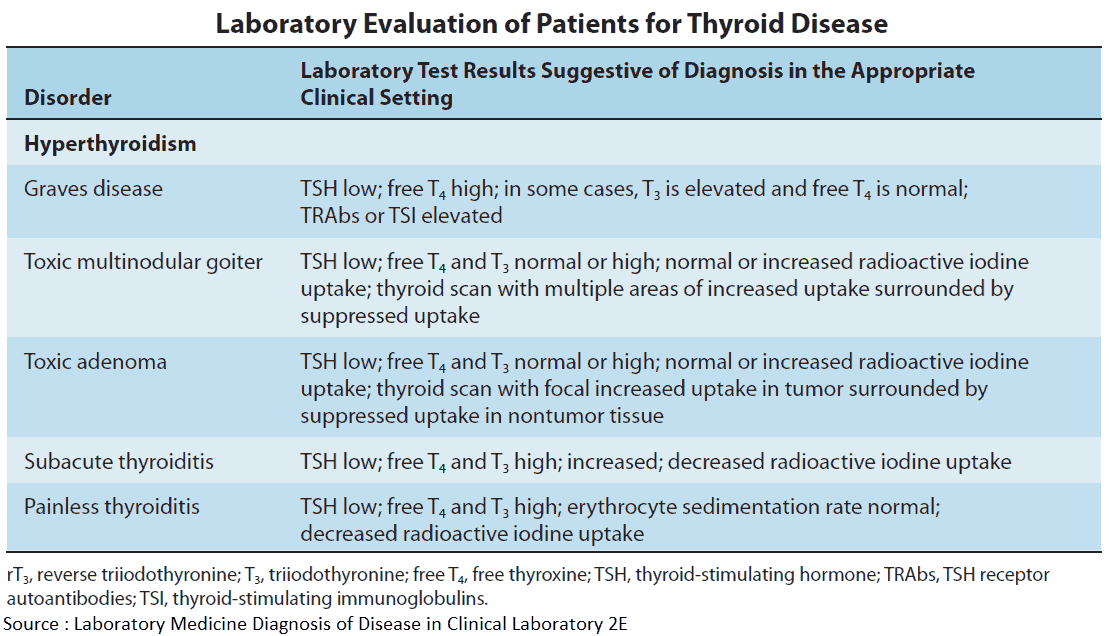
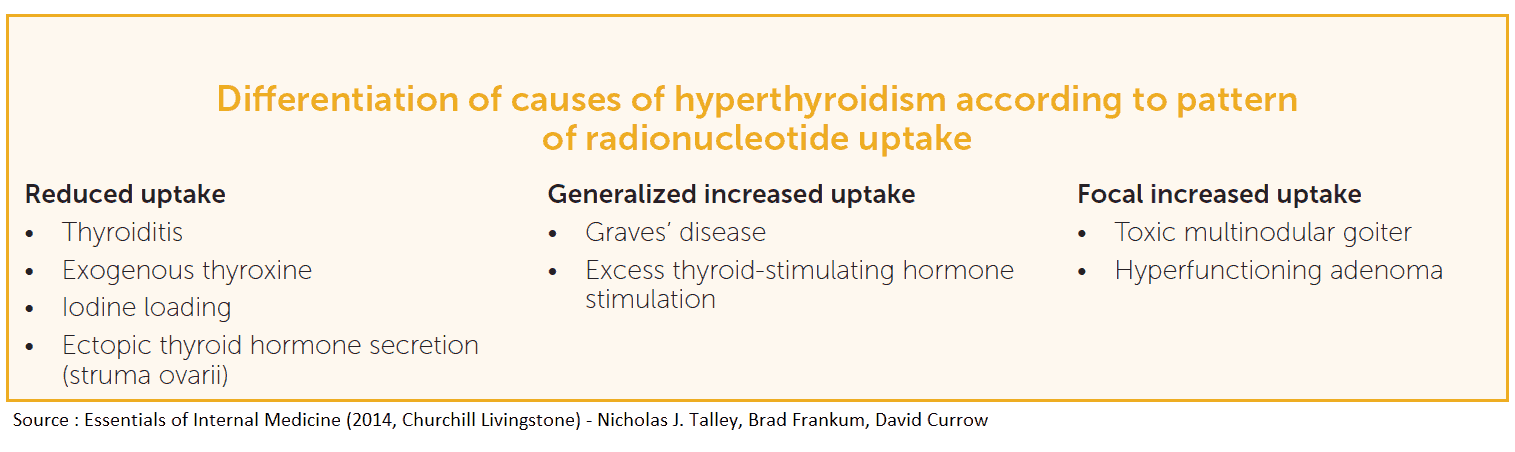
Investigations and Diagnosis of Hyperthyroidism
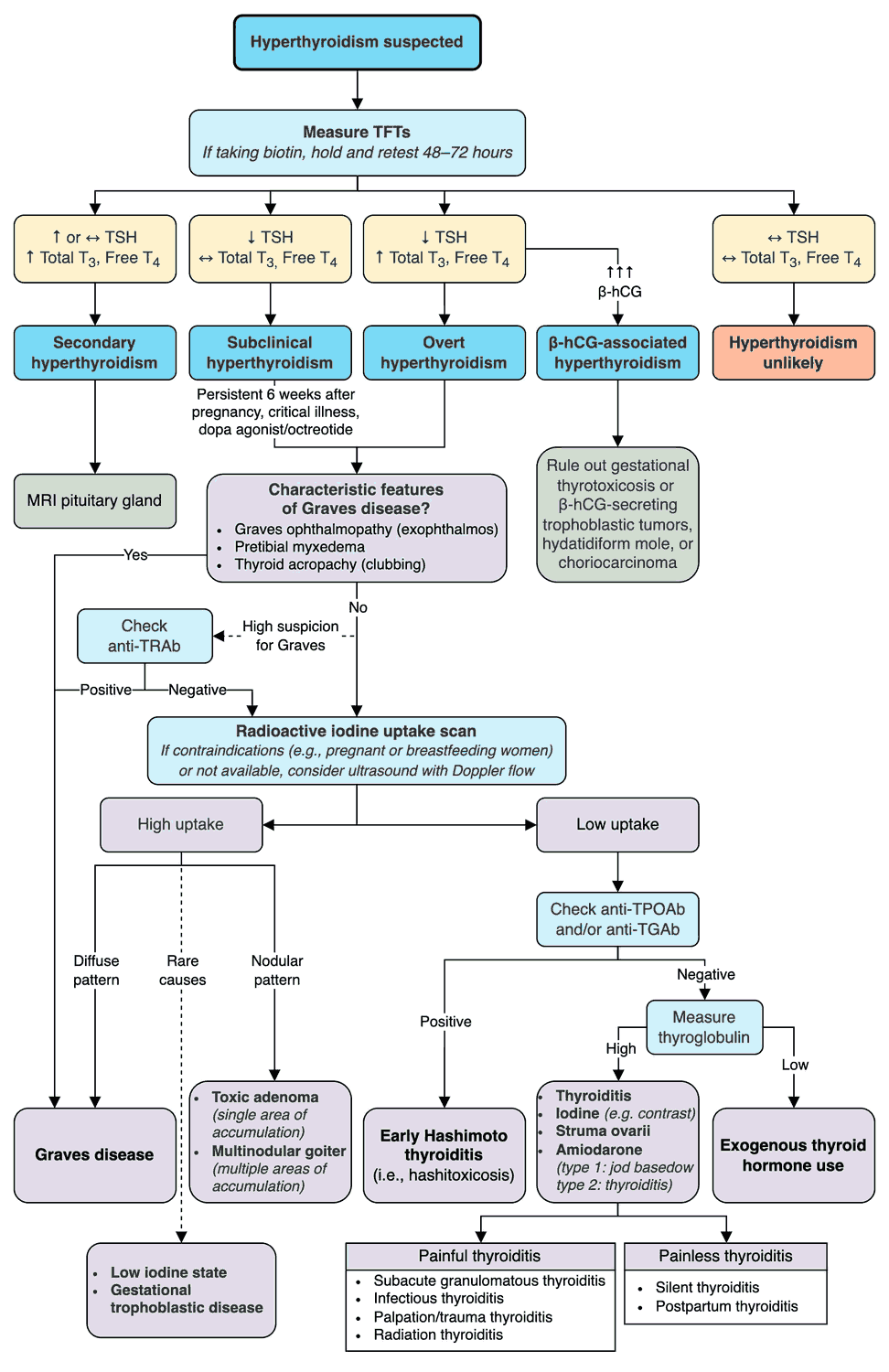
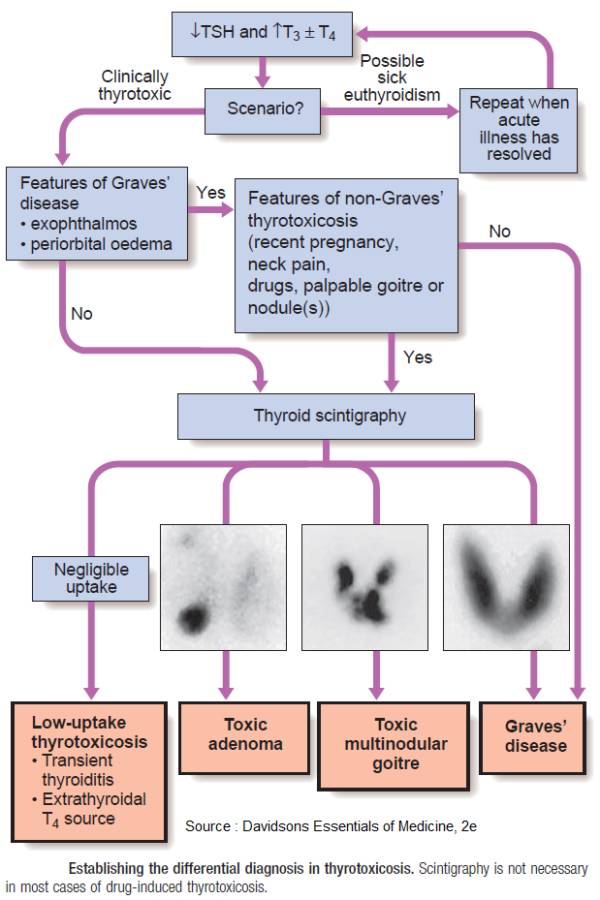
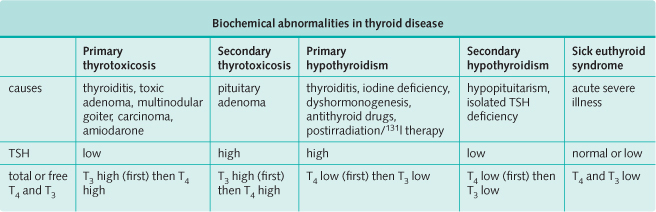
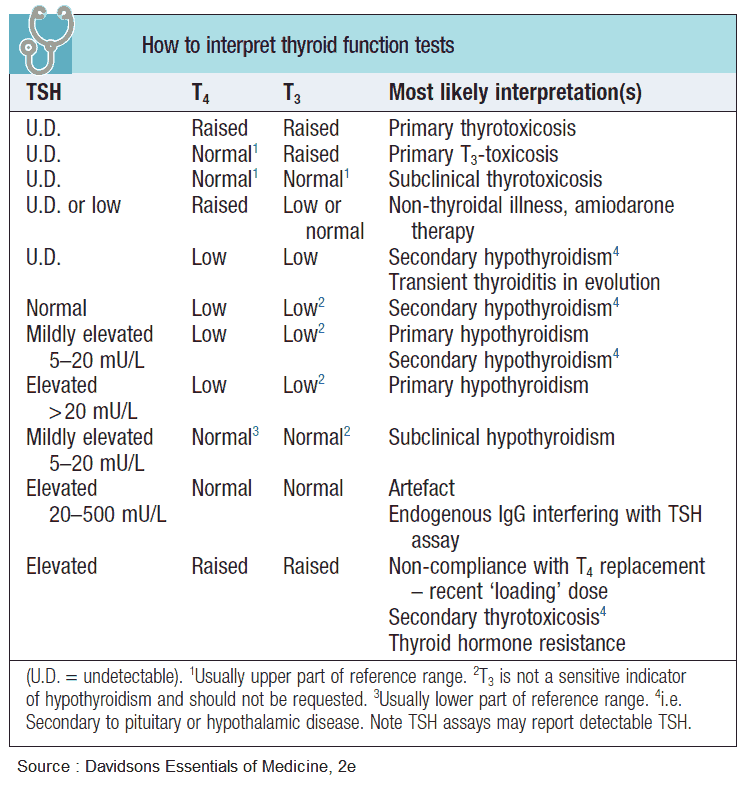
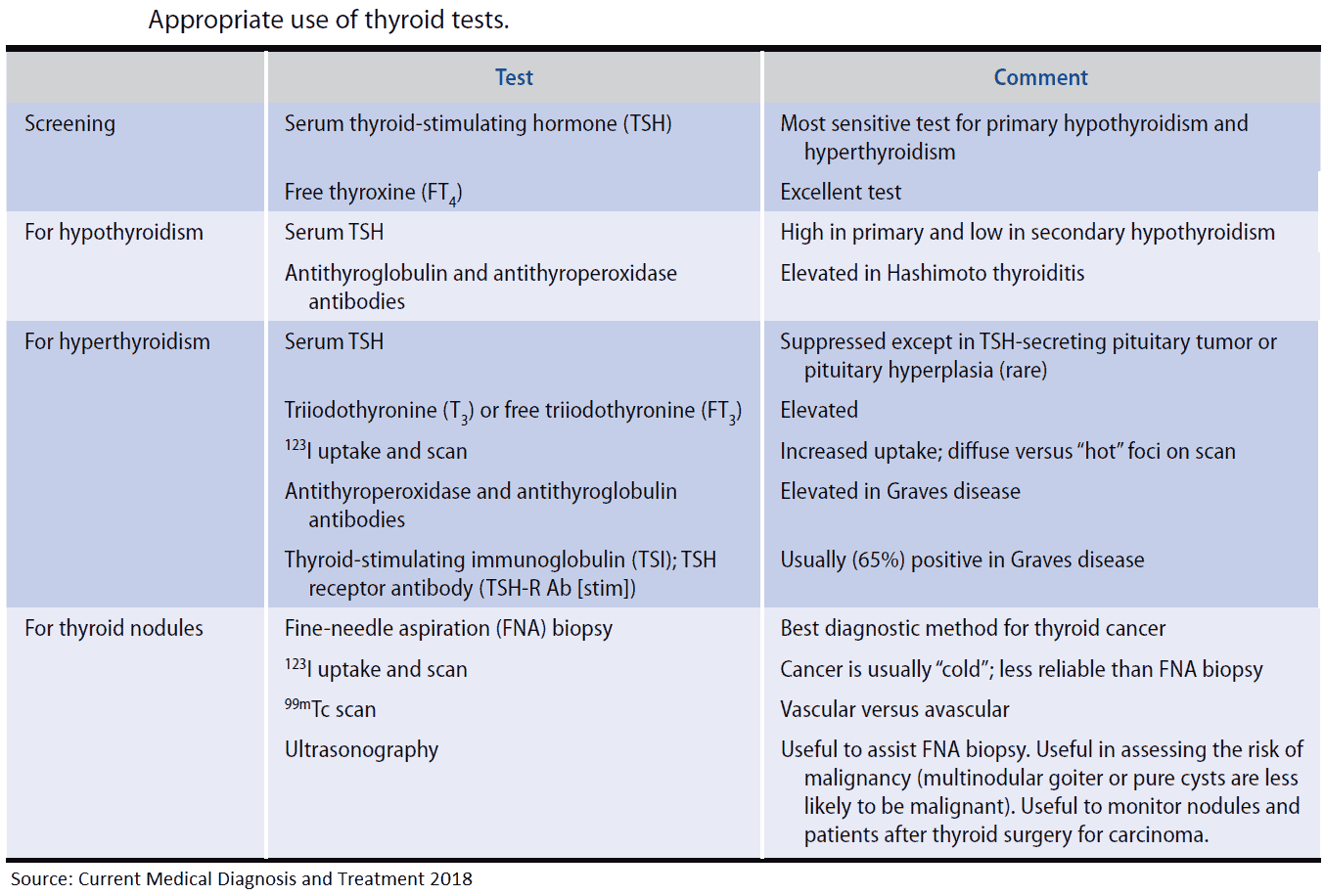
Thyroid status can now be easily assessed by the measurement of:
- Thyroid-stimulating hormone (TSH)
- Total thyoxine (T4)
- Total tri-iodothyronine (T3)
Around 99% of circulating T4 and T3 is bound to protein (mostly thyroxine-binding globulin-TBG). It is the free T4 and T3 that is physiologically active and can be measured separately. The TRH stimulation test, which used to be important in the diagnosis of hyperthyroidism, is now almost never necessary
TSH is suppressed in thyrotoxicosis. It can also be suppressed in euthyroid patients with Graves’ ophthalmopathy, large goiters, recent treatment for thyrotoxicosis, or severe nonthyroid illness.
T4 is raised although excess estrogens, protein-losing states, drugs, and hereditary abnormalities can alter the binding of T4 to thyroxine-binding globulin, making total T4 levels inaccurate in these situations. Free T4 assays are therefore preferable. If the TSH is suppressed and free T4 is normal, T3 should be measured to diagnose T3 toxicosis.
In Graves’ disease, 80% of people have serum autoantibodies against thyroglobulin and thyroid peroxidase/microsomal antigen. However, these also occur in autoimmune thyroiditis, and in 15% of healthy women and 5% of healthy men.
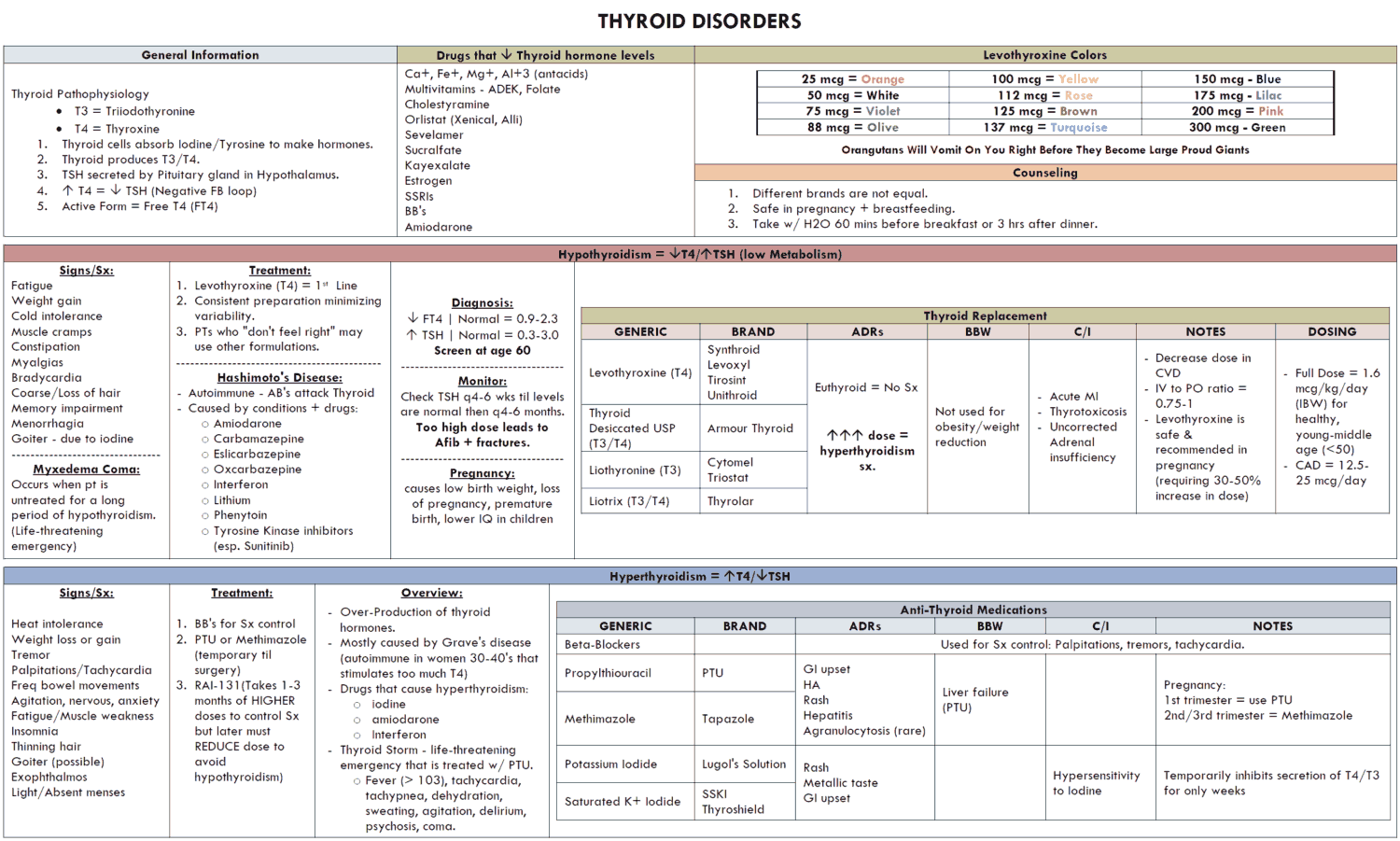
Management and Treatment of Hyperthyroidism
Treatment options include:
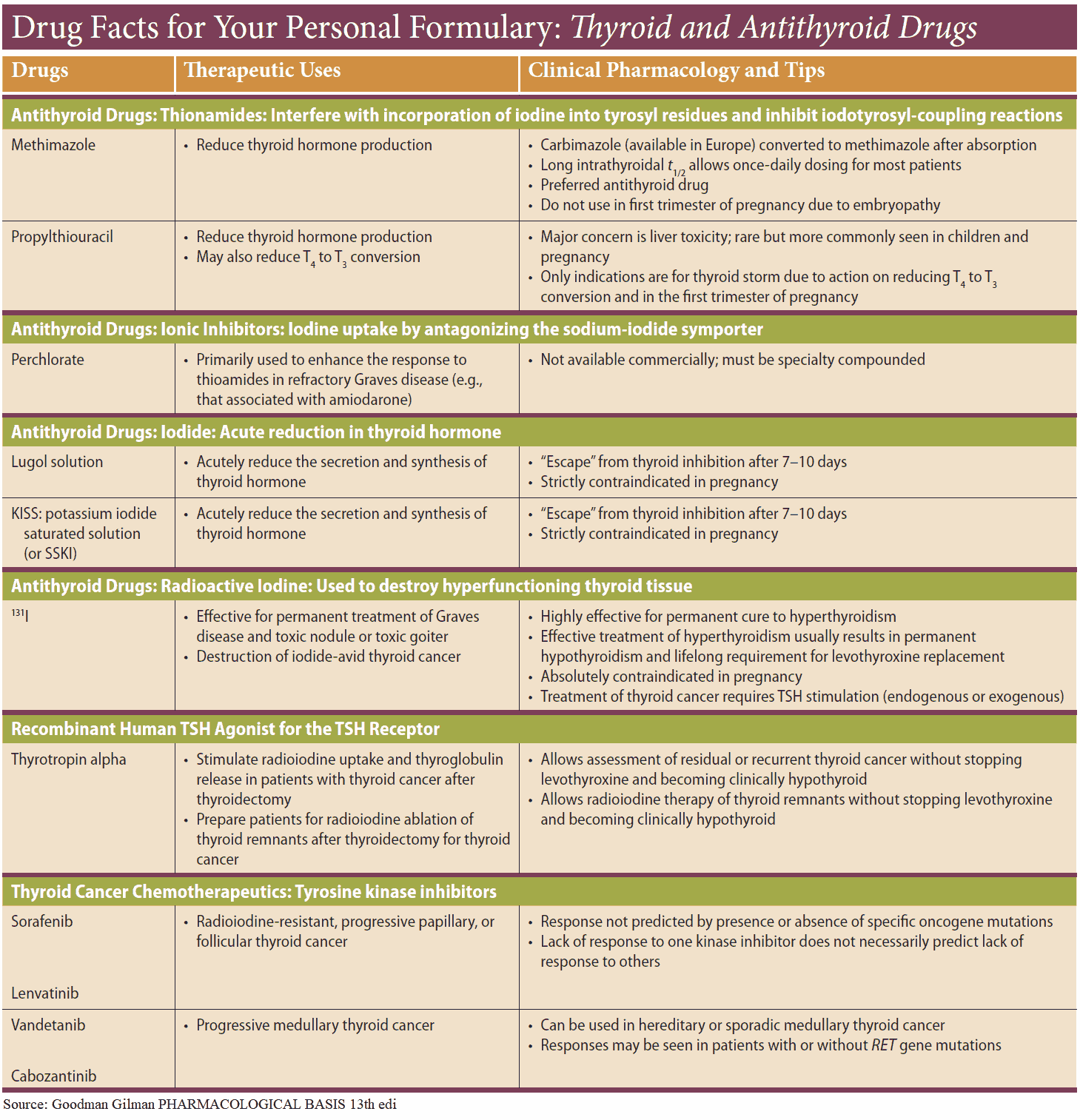
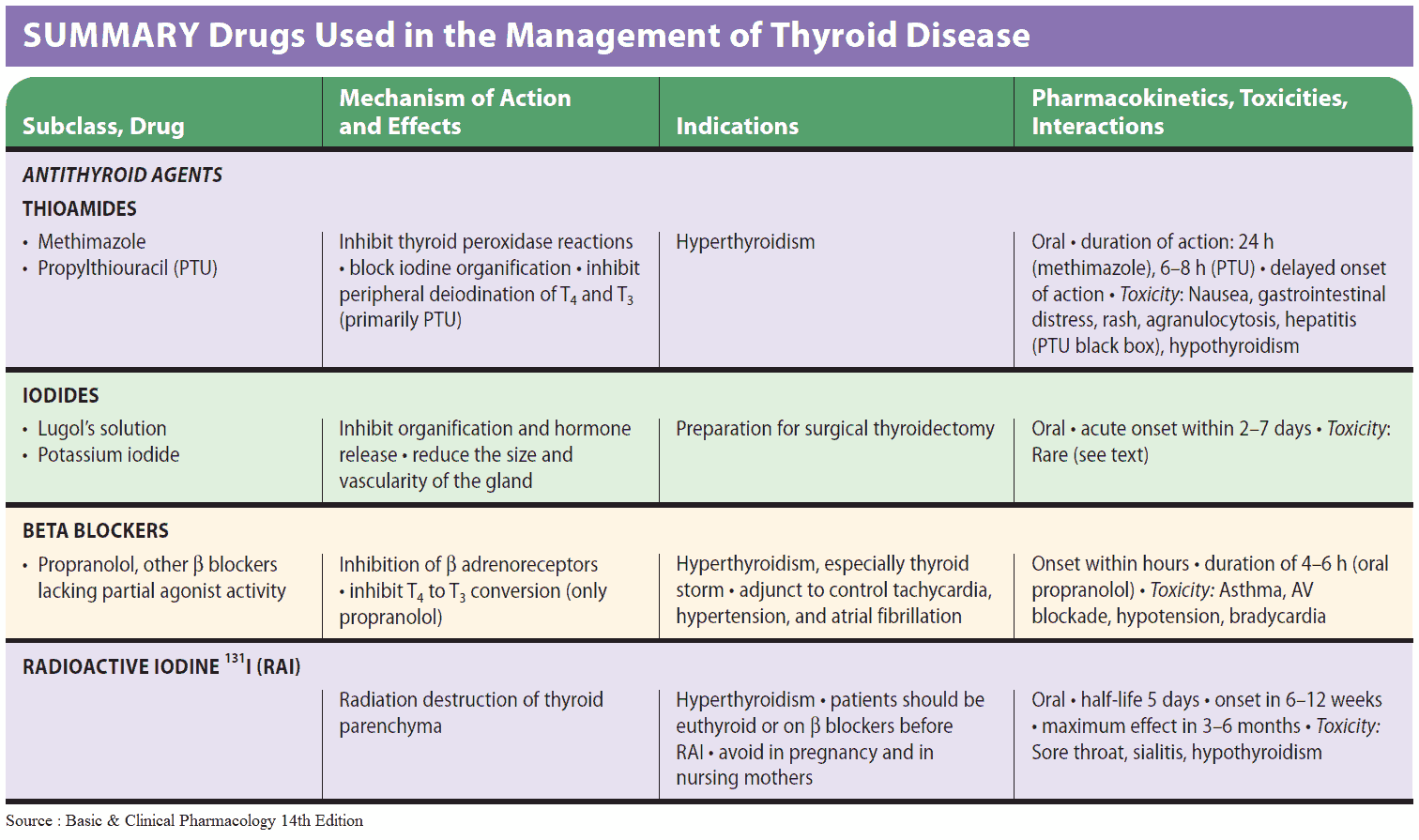
- Antithyroid Drugs
- Propylthiouracil (PTU)
- Methimazole, Thiamazole, Carbimazole
- Radioiodine (131I)
- Surgery (thyroidectomy)
Most patients under 50 years old receive a course of antithyroid drug as initial treatment. Patients with large goiters usually relapse after antithyroid drugs. Relapse after a period of drug therapy should be treated with 131I or subtotal thyroidectomy; 131I is generally given to older patients in whom recurrent thyrotoxicosis may be dangerous.
Subtotal thyroidectomy is often recommended in young patients with large goiters to remove the neck swelling. All options should be discussed with the patient and a joint decision should be arrived at.
Antithyroid Drugs
In the U.S. methimazole is the most commonly used drug. Propylthiouracil (PTU) may be used in patients who suffer sensitivity reactions to methimazole. Both drugs act primarily by interfering with the synthesis of thyroid hormones.
Methimazole is given in a daily dose of 30-40 mg and maintained at this dose until the patient becomes euthyroid, usually after 4-8 weeks. The dose may then be progressively changed to a maintenance dose of 5-15 mg daily, adjusted according to response. Rashes are common and PTU may then be substituted. Pruritus and rashes can also be treated with antihistamines without discontinuing therapy, although patients should be advised to report any sore throat immediately because of the rare complication of agranulocytosis.
Propylthiouracil (PTU) is given in a dose of 450 mg every 8 hours and maintained at this dose until the patient becomes euthyroid. The dose is then lowered to a maintenance dose of 50-150 mg daily.
A combination of methimazole, 20-60 mg daily, with thyroxine, 50-150 μg daily, may be used in a blocking replacement regimen. Treatment is usually for 18 months-this regimen is not suitable during pregnancy. Iodine may be given 10-14 days before surgery in addition to carbimazole to assist control and to reduce vascularity of the thyroid.
Propanolol is useful for the rapid relief of thyrotoxic symptoms because antithyroid drugs may take several weeks to produce an improvement in symptoms. They are also useful for the control of supraventricular arrhythmias secondary to thyrotoxicosis.
Radioiodine
Radioactive sodium iodide (Na131I) is concentrated by the thyroid and causes cell damage and cell death. Hypothyroidism may therefore develop at any stage after treatment, and so the patient should be under regular follow-up.
It is used increasingly for the treatment of thyrotoxicosis at all ages, particularly where medical therapy or compliance is a problem, in patients with cardiac disease, and in patients who relapse after thyroidectomy. Contraindications include pregnancy and breastfeeding. Pregnancy is safe 4 months or more after treatment.
Subtotal Thyroidectomy
The aim of surgery is to remove sufficient thyroid tissue to cure hyperthyroidism. One year later about 80% of patients are euthyroid, 15% hypothyroid, and 5% have relapsed. Complications include hypoparathyroidism, recurrent laryngeal nerve damage, and bleeding into the neck causing laryngeal edema.
READ MORE: Hyperthyroidism and Antithyroid Drugs
Treatment of Thyrotoxic crisis (thyroid “storm”)
This is an uncommon, life-threatening exacerbation of thyrotoxicosis with a mortality of 50%. Precipitating factors include thyroid surgery, radioiodine, withdrawal of antithyroid drugs, iodinated contrast agents, and acute illnesses (e.g., stroke, infection, trauma, and diabetic ketoacidosis).
It requires emergency treatment with oxygen, intravenous fluids due to profuse sweating, propanolol (5 mg IV) for control of tachycardia, hydrocortisone (100 mg 6 hourly IV), which inhibits T4 conversion to T3 in the tissues, as well as oral iodine solution, which may need to be administered by nasogastric tube. PTU is also given at doses of 300-400 mg every 8 hours to block any further synthesis of thyroid hormones.
READ MORE: Recognizing and Treating Thyroid Storm
Subacute (de Quervain’s) thyroiditis
Various viruses (e.g., enterovirus or coxsackievirus) can cause subacute thyroiditis. Patients present with a small, tender goiter and initially thyrotoxicosis caused by release of stored thyroid hormones. There may be a history of preceding “flu-like” illness. Some weeks later there is a period of hypothyroidism followed by the recovery of normal thyroid function 3-6 months after onset. The erythrocyte sedimentation rate is raised and there is low radioisotope uptake by the thyroid. Treatment is with NSAIDs for mild symptoms, and with high-dose prednisone for moderate or severe thyroiditis. The dose is gradually tailed off in subsequent weeks.