Table of Contents
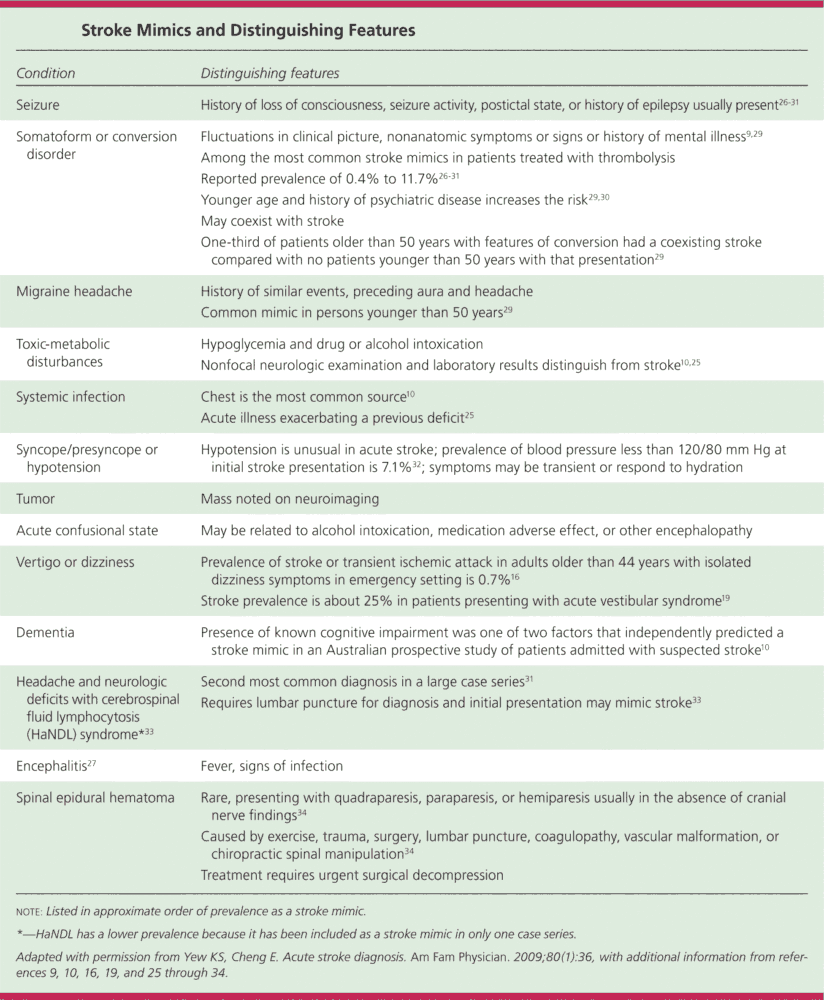
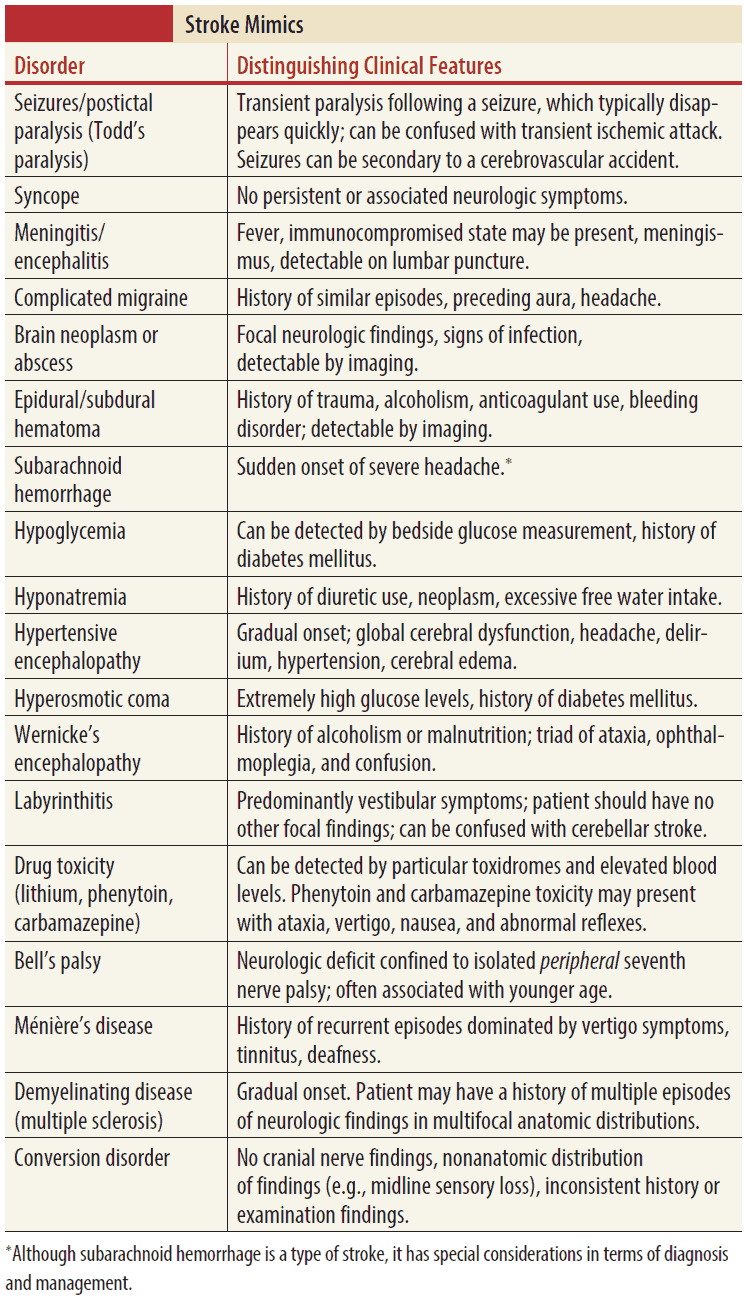
- Acute Stroke mimics, or nonvascular disorders that produce focal neurologic deficits, often confound the diagnosis of acute ischemic stroke.
- As many as 20% to 25% of suspected acute stroke presentations can be attributed to nonvascular disease processes. In an age of new interventional stroke therapies that include endovascular treatment and fibrinolysis, it is increasingly important to identify stroke imitators and avoid potential harm from secondary stroke prevention therapies.
- Common stroke imitators include, but are not limited to:
- Todd paralysis
- Hypoglycemia
- Cerebral neoplasm
- Hemiplegic migraine
- Functional hemiparesis
Todd Paralysis
- Todd paralysis is a transient neurologic condition that is most commonly characterized by focal paresis following a seizure.
- Reversible, nonstructural alterations in neuronal function that occur in the postictal period may cause focal neurologic deficits that simulate the presentation of acute stroke.
- While the duration of these deficits is generally transient, focal findings can last up to 1 to 2 days.
- Postictal weakness is primarily seen after partial motor seizures but can also follow generalized seizures.
- Often, this stroke mimic is only identified after witnessing further seizure activity or inquiring about a history of seizure disorder.
Hypoglycemia
- Hypoglycemia can be defined as a serum glucose level below normal and is considered severe when levels fall below 45 mg/dL (2.5 mmol/L) .
- It is the quintessential stroke mimic as it is the most rapidly identifiable and easily reversible nonvascular cause of neurologic deficits.
- Hemiplegia, cortical blindness, and aphasia have all been reported as common stroke-like presentations of hypoglycemia.
- While it is essential for physicians to obtain a rapid serum glucose level in any patient suspected of having an acute stroke, it must also be noted that neurologic deficits may occasionally persist for hours after IV glucose administration.
- Other metabolic imbalances such hyperglycemia, hypernatremia, hyponatremia, and hepatic encephalopathy can present similarly.
Cerebral Neoplasm
- Though primarily indolent in presentation, intracerebral mass lesions can cause rapidly progressive visual changes, aphasia, and other focal neurologic deficits that mimic acute stroke.
- As many as 6% of patients with brain tumors present with symptoms that are <1 day in duration.
- This stroke-like clinical picture can be attributed to a variety of mechanisms including:
- Obstructive hydrocephalus
- Vascular compression
- Tumor apoplexy
Hemiplegic Migraine
- Primary headache disorders account for 9% of stroke mimics. One rare migraine variant, the familial hemiplegic migraine (FHM), is defined as migraine with aura consisting of fully reversible motor weakness.
- Autosomal dominant in inheritance, FHM most commonly affects young females and shows high familial penetrance.
- Though FHM is a diagnosis of exclusion, a careful family history or evidence of prior similar recurrent episodes may raise suspicion of this migraine subtype.
Functional Hemiparesis
- Conversion disorder, or functional neurologic symptom disorder, is characterized by neurologic symptoms that are inconsistent with a medical etiology but not intentionally produced by the patient.
- Weakness can be seen in up to 30% of these individuals, and though most commonly unilateral or hemiparetic, can also be bilateral or affect only a single limb.
- Key to identifying conversion disorder as a stroke mimic is an inconsistent exam, where the extent of the impairment is often found to be task dependent.
- On physical examination, Hoover sign, or weakness with hip extension in the affected leg that disappears during contralateral flexion of the unaffected leg against resistance, can suggest a functional etiology of paresis.
Todd paralysis, hypoglycemia, cerebral neoplasm, hemiplegic migraine, and functional hemiparesis constitute just a few of the many disease processes that can present with a stroke-like clinical picture.
Other stroke mimics include:
- Infection,
- Syncope,
- Peripheral vestibular disorders,
- Dementia, and
- Intoxication.
Given the extensive list of stroke mimics as well as the diagnostic limitations in detecting ischemic strokes in the emergency department, it is important to keep a broad differential and perform a thorough history in any patient who at first glance appears to be suffering a stroke.
Key Points
- Twenty to twenty-five percent of suspected stroke presentations are attributable to nonvascular etiologies.
- In an era of invasive and potentially harmful secondary stroke prevention therapies, it is increasingly important to rapidly identify stroke mimics.
- Common stroke mimics include hypoglycemia, Todd paralysis, primary headache disorders, cerebral neoplasm, and functional hemiparesis.
- Obtain a rapid serum glucose level, and consider nonvascular disease processes in any patient with acute neurologic impairment.