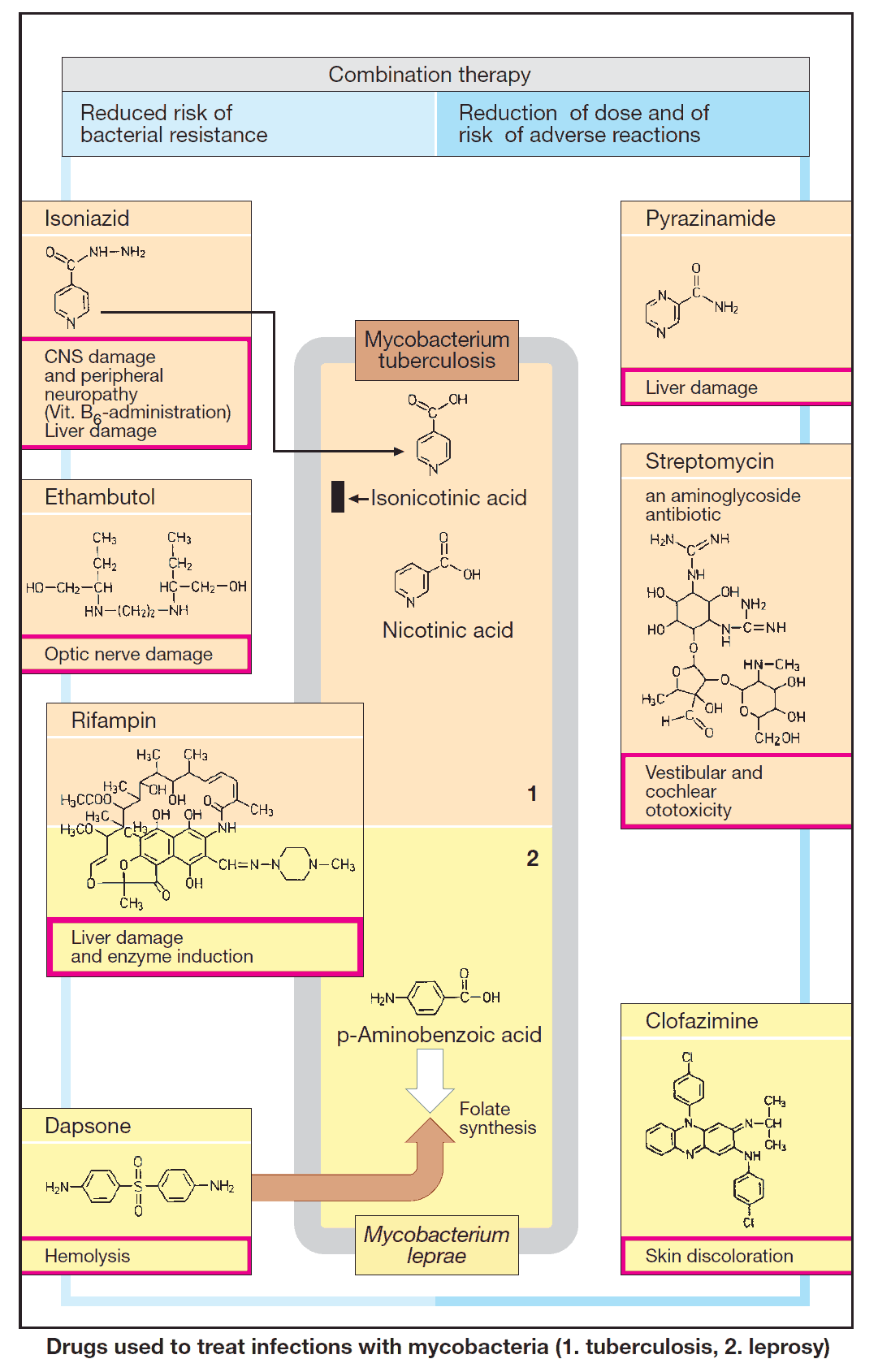
Mycobacteria are responsible for two diseases:
- Tuberculosis, mostly caused by M. tuberculosis
- Leprosy due to M. leprae
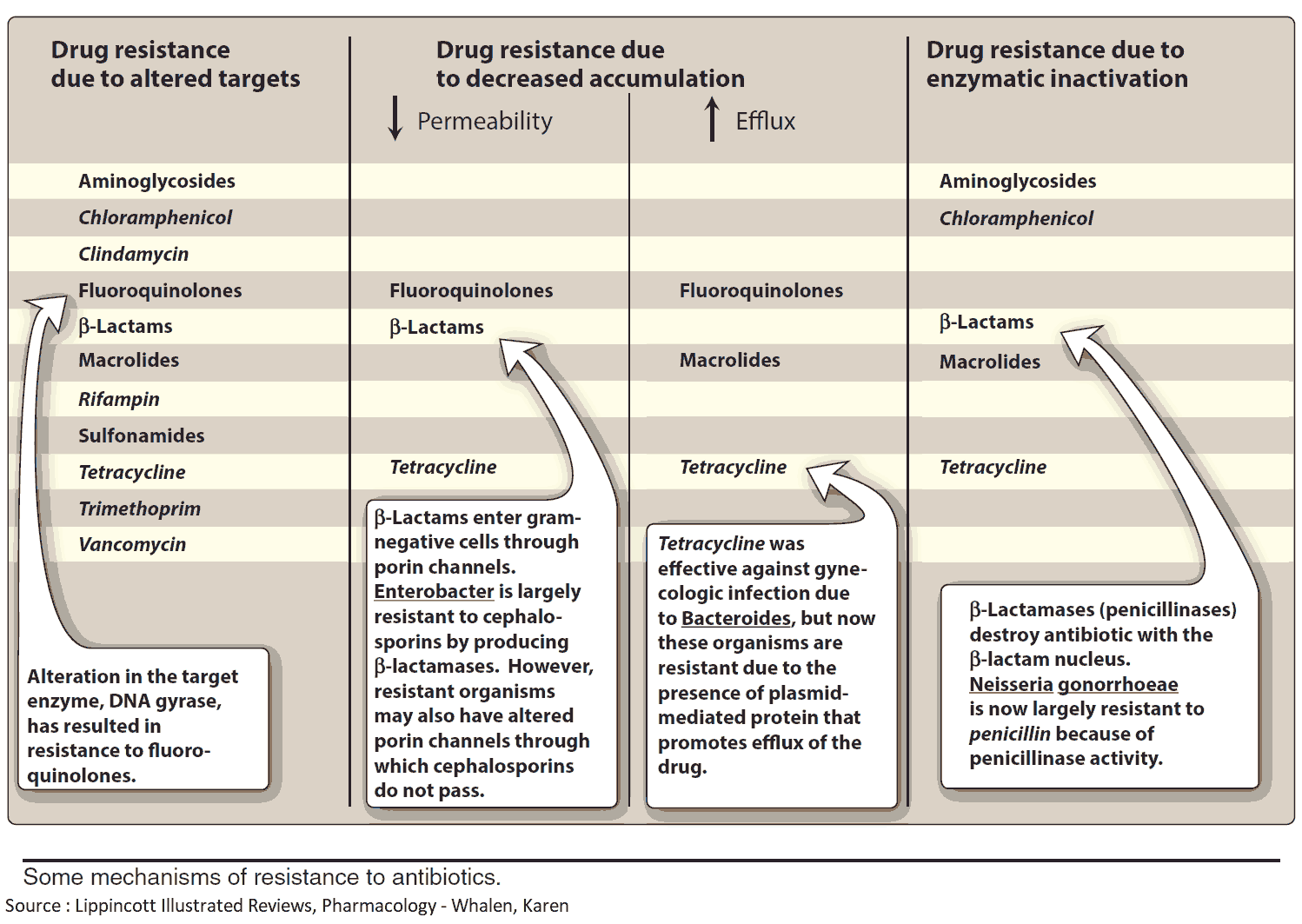
The therapeutic principle applicable to both is combined treatment with two or more drugs. Combination therapy prevents the emergence of resistant mycobacteria.
Because the antibacterial effects of the individual substances are additive, correspondingly smaller doses are sufficient. Therefore, the risk of individual adverse effects is lowered. Most drugs are active against only one of the two diseases.
Antitubercular Drugs
Drugs of choice for Tuberculosis are:
- isoniazid
- rifampin
- ethambutol
- streptomycin
- pyrazinamide
Less well tolerated, second-line agents include: p-aminosalicylic acid, cycloserine, viomycin, kanamycin, amikacin, capreomycin, ethionamide.
Isoniazid
Isoniazid is bactericidal against growing M. tuberculosis. Its mechanism of action remains unclear. (In the bacterium it is converted to isonicotinic acid, which is membrane impermeable, hence likely to accumulate intracellularly.)
Isoniazid is rapidly absorbed after oral administration. In the liver, it is inactivated by acetylation, the rate of which is genetically controlled and shows a characteristic distribution in different ethnic groups (fast vs. slow acetylators).
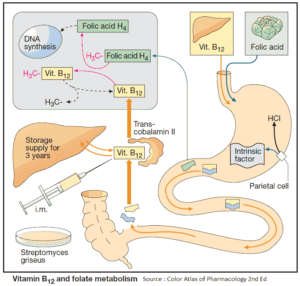
Notable adverse effects of Isoniazid are:
- peripheral neuropathy
- optic neuritis preventable by administration of vitamin B6 (pyridoxine)
- hepatitis
- jaundice
Rifampin
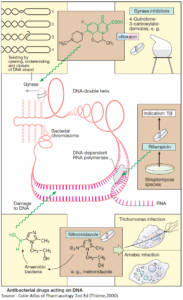
Rifampin inhibits the bacterial enzyme that catalyzes DNA template-directed RNA transcription, i.e., DNA-dependent RNA polymerase. Rifampin acts bactericidally against mycobacteria (M. tuberculosis, M. leprae), as well as many gram-positive and gram-negative bacteria.
It is well absorbed after oral ingestion. Because resistance may develop with frequent usage, it is restricted to the treatment of tuberculosis and leprosy.
Rifampin is contraindicated in the first trimester of gestation and during lactation. Rifabutin resembles rifampin but may be effective in infections resistant to the latter.
Adverse effects of Rifampin:
- hepatic damage
- hypersensitivity with flu-like symptoms
- disconcerting but harmless red/orange discoloration of body fluids
- enzyme induction (failure of oral contraceptives)
Ethambutol
The cause of its specific antitubercular action is unknown. Ethambutol is given orally. It is generally well tolerated, but may cause dose-dependent damage to the optic nerve with disturbances of vision (red/green blindness, visual field defects).
Pyrazinamid
Pyrazinamide exerts a bactericidal action by an unknown mechanism. It is given orally. Pyrazinamide may impair liver function; hyperuricemia results from inhibition of renal urate elimination.
Streptomycin
Streptomycin must be given i.v. like other aminoglycoside antibiotics. It damages the inner ear and the labyrinth. Its nephrotoxicity is comparatively minor.
Antileprotic Drugs
Rifampin is frequently given in combination with Dapsone and/or Clofazimine.
Dapsone
Dapsone is a sulfone that, like sulfonamides, inhibits dihydrofolate synthesis. It is bactericidal against susceptible strains of M. leprae. Dapsone is given orally. The most frequent adverse effect is methemoglobinemia with accelerated erythrocyte degradation (hemolysis).
Clofazimine
Clofazimine is a dye with bactericidal activity against M. leprae and antiinflammatory properties. It is given orally, but is incompletely absorbed.
Because of its high lipophilicity, it accumulates in adipose and other tissues and leaves the body only rather slowly (t1/2 ~ 70 d). Red-brown skin pigmentation is an unwanted effect, particularly in fair-skinned patients.