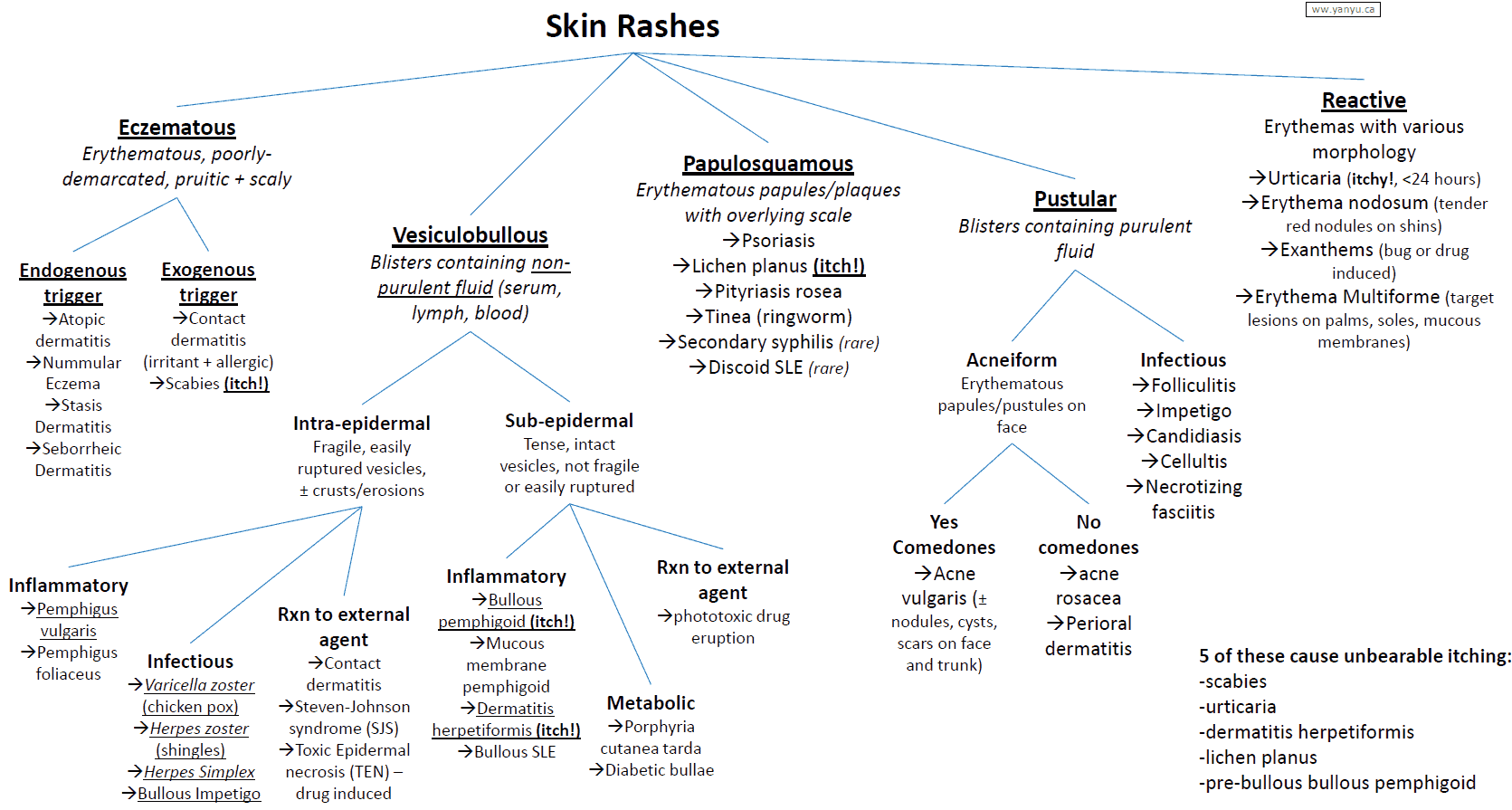
Differential Diagnosis of Skin Rashes and Lesions by Appearance
Pigmented lesions
- Freckles (ephelides): flat, brown spots.
- Lentigo: similar to freckles but darker and not affected by sunlight.
- Seborrheic keratosis: benign, beige/brown plaques, 3-20 mm in diameter, with a velvety or warty surface.
- Nevus: moles.
- Blue nevus: small, slightly elevated, blue-black lesions.
- Atypical (dysplastic) nevus: over 5 mm across, ill-defined, irregular border, irregularly distributed pigmentation with erythema and accentuated skin markings.
- Melanoma: flat or raised pigmented lesion with possibly a recent change in appearance. It has varying colors and typically irregular borders.
Scaly lesions
- Psoriasis: silvery, scaled, well-demarcated plaques on skin, usually over the extensor surfaces. It can be pustular and involve the nails (nail pitting).
- Dermatitis and eczema: a pruritic, exudative, or lichenified eruption on the face, neck, upper trunk, wrists, and hands, and in the antecubital and popliteal fossae.
- Xerosis: dry skin.
- Lichen simplex chronicus: chronic itching associated with pigmented, lichenified, skin lesions. Lichenified lesions exhibit exaggerated skin lines overlying thickened, well-circumscribed, scaly plaques.
- Tinea corporis: ring-shaped lesion with an advancing scaly border and central clearing or scaly patches with a distinct border.
- Tinea versicolor: pale or hyperpigmented macules, or velvety, tan, pink, whitish, or brown macules that scale with scraping.
- Secondary syphilis.
- Pityriasis rosea: oval, fawn-colored, scaly eruption following the cleavage lines of the trunk (“Christmas tree” pattern). It is commonly preceded by a herald patch.
- Discoid lupus erythematosus: red, asymptomatic, localized plaques, usually on the face and often in a “butterfly” distribution. There is scaling, follicular plugging, atrophy, and telangiectasia of involved areas.
- Exfoliative dermatitis: scaling and erythema over a large area of the body.
- Actinic keratoses: small, pink patches that feel like bits off sandpaper when the finger is drawn over them. They are premalignant.
- Bowen’s disease (intraepidermal squamous cell carcinoma): small, well-demarcated, slightly raised, pink-to-red, scaly plaques.
- Extramammary Paget’s disease: this resembles chronic eczema and may involve apocrine areas such as the genitals.
- Intertrigo: fissuring, erythema, and sodden epidermis, with superficial denudation in the body folds.
Vesicular lesions
- Herpes simplex: recurrent, small, grouped vesicles on an erythematous base, especially around the oral and genital areas; often described as “dew drops on a rose petal.”
- Herpes zoster: vesicular lesions in a dermatomal distribution.
- Pompholyx: pruritic “tapioca” vesicles or bullae on the palms, soles, and sides of fingers.
- Dermatophytid (allergy or sensitivity to fungi): pruritic, grouped, vesicular lesions involving the sides and flexor aspects of the fingers and palms.
- Dermatitis herpetiformis: pruritic papulovesicular lesions, mainly on the elbows, knees, buttocks, posterior neck, and scalp. It is associated with gluten-sensitive (i.e., sprue) enteropathy.
- Miliaria (heat rash): superficial, aggregated, small vesicles, papules, or pustules on covered areas of the skin.
- Scabies: pruritic vesicles and pustules especially on the sides of the fingers. Red papules or nodules on the penile glans and shaft are pathognomonic. Photosensitivity.
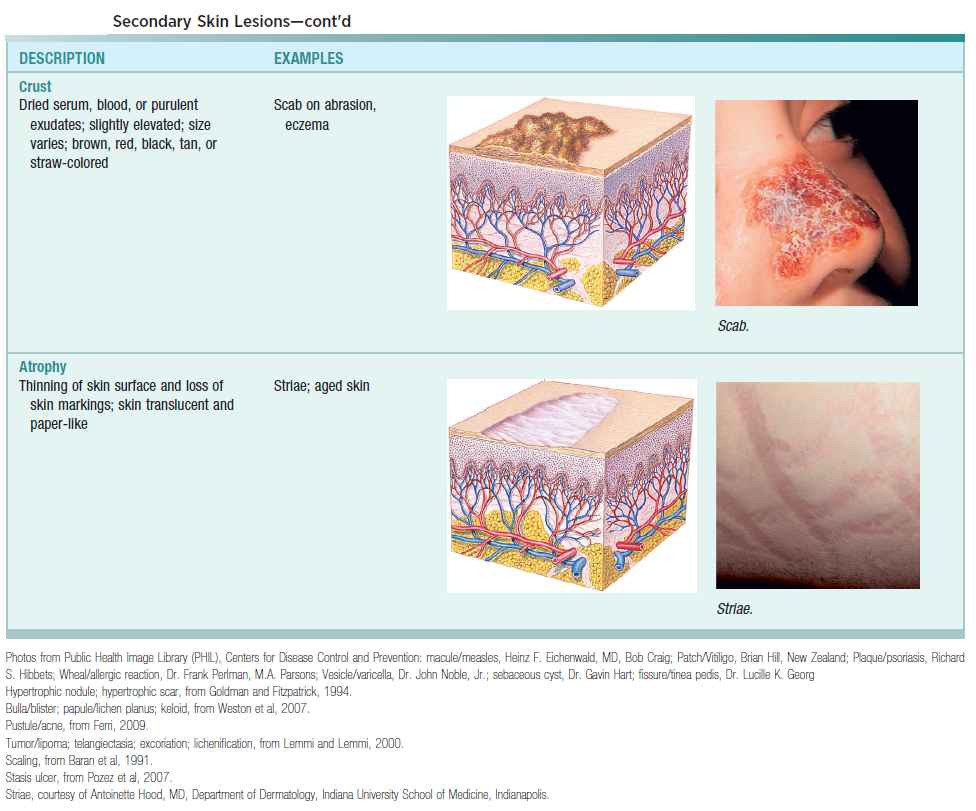
Weepy or encrusted lesions
- Impetigo: vesiculopustular lesions with thick, golden-crusted exudate associated with group A β-hemolytic streptococci or coagulase-positive Staphylococcus aureus, or bullous lesions associated with S. aureus.
- Acute-contact allergic dermatitis: erythema and oedema, with pruritus, often followed by vesicles and bullae in an area of contact with a suspected agent. They may later weep, crust, and become infected.
- Any vesicular dermatitis.
Pustular lesions
Any type of superficial skin infection (bacterial or fungal) can cause pustules.
- Acne vulgaris: the most common skin condition, characterized by open and closed comedones. It varies from purely comedonal to pustular inflammatory acne to cysts to nodules.
- Acne rosacea: erythema and telangiectasia and a tendency to flush easily. May have an acneiform component, or hyperplasia of the soft tissue of the nose (rhinophyma).
- Folliculitis: pustules in the hair follicles.
- Candidiasis: superficial, denuded, beefy-red areas with or without satellite vesicopustules. Whitish, curd-like concretions on the oral and vaginal mucous membranes.
- Miliaria.
- Any vesicular dermatitis.
Figurate erythema
Figurate erythema lesions look like rings or arcs.
- Urticaria: eruptions of evanescent wheals or hives.
- Erythema multiforme: symmetrical erythematous lesions on the extensor surfaces, palms, soles, or mucous membranes, which may be macular, papular, urticarial, bullous, or purpuric. Target lesions with clear centers and concentric erythematous rings may be present. This is often associated with drug rashes.
- Erythema migrans: a red expansion around an initial papule with an advancing border, which is usually raised, warm, and red. The center may clear or become indurated, vesicular, or necrotic. This is commonly associated with Lyme disease.
- Cellulitis: a hot, red, diffuse, spreading infection of the skin.
- Erysipelas: edematous, spreading, circumscribed, hot, erythematous area, with or without vesicle or bulla formation, frequently involving the face.
- Erysipeloid: purplish erythema, most often of a finger or the back of the hand, which gradually extends. Caused by Erysipelothrix insidiosa, it is often seen in fishermen and meat handlers.
Bullous lesions
- Impetigo: superficial bacterial infection caused by group A β-hemolytic streptococci or S. aureus.
- Pemphigus: relapsing crops of bullae appearing on normal skin, often preceded by mucous membrane bullae, erosions, and ulcerations. There may be superficial detachment of the skin after pressure or trauma (Nikolsky’s sign).
- Bullous pemphigoid: tense blisters in flexural areas. They may be preceded by urticarial or edematous lesions.
- Porphyria cutanea tarda.
- Erythema multiforme: “target” lesions, i.e., symmetrically distributed, circular lesions, often with a central blister.
- Toxic epidermal necrolysis: usually secondary to drugs (e.g., sulphonamides, penicillins, and anticonvulsants). This is a severe form of Steven-Johnson syndrome.
Papular lesions
- Hyperkeratotic: warts, corns, seborrheic keratoses.
- Purple: lichen planus-pruritic, violaceous, flat-topped papules with fine white streaks and a symmetrical distribution, commonly seen along linear scratch marks on the anterior wrists, sacral region, penis, legs, and mucous membranes; drug eruptions; Kaposi’s sarcoma-malignant skin lesions with dark plaques or nodules on cutaneous or mucosal surfaces, common in people with human immunodeficiency virus infection.
- Flesh–colored and umbilicated: molluscum contagiosum-a viral infection causing single or multiple, rounded, dome-shaped, waxy papules, 2-5 mm in diameter, which are umbilicated and contain a caseous plug.
- Pearly: basal cell carcinoma-most commonly papules or nodules with a central scab or erosion; intradermal nevi.
- Small, red, and inflammatory: acne, miliaria, candidiasis, intertrigo, scabies, folliculitis.
Nodular, cystic lesions
- Erythema nodosum: painful red nodules without ulceration on the anterior aspects of the legs; they may regress over weeks to resemble contusions. This is associated with inflammatory bowel disease.
- Furuncle (boils): painful inflammatory swellings of a hair follicle forming an abscess, caused by S. aureus.
- Cystic acne.
- Follicular (epidermal) inclusion cyst.
Photodermatoses
Painful erythema, edema, and vesiculation on sun-exposed surfaces, usually the face, neck, hands, and V of the chest. Causes include drugs (e.g., amiodarone, phenothiazines, sulphonamides, and related drugs), polymorphic light eruption, and systemic lupus erythematosus (SLE).
Maculopapular lesions
Viral causes and secondary syphilis.
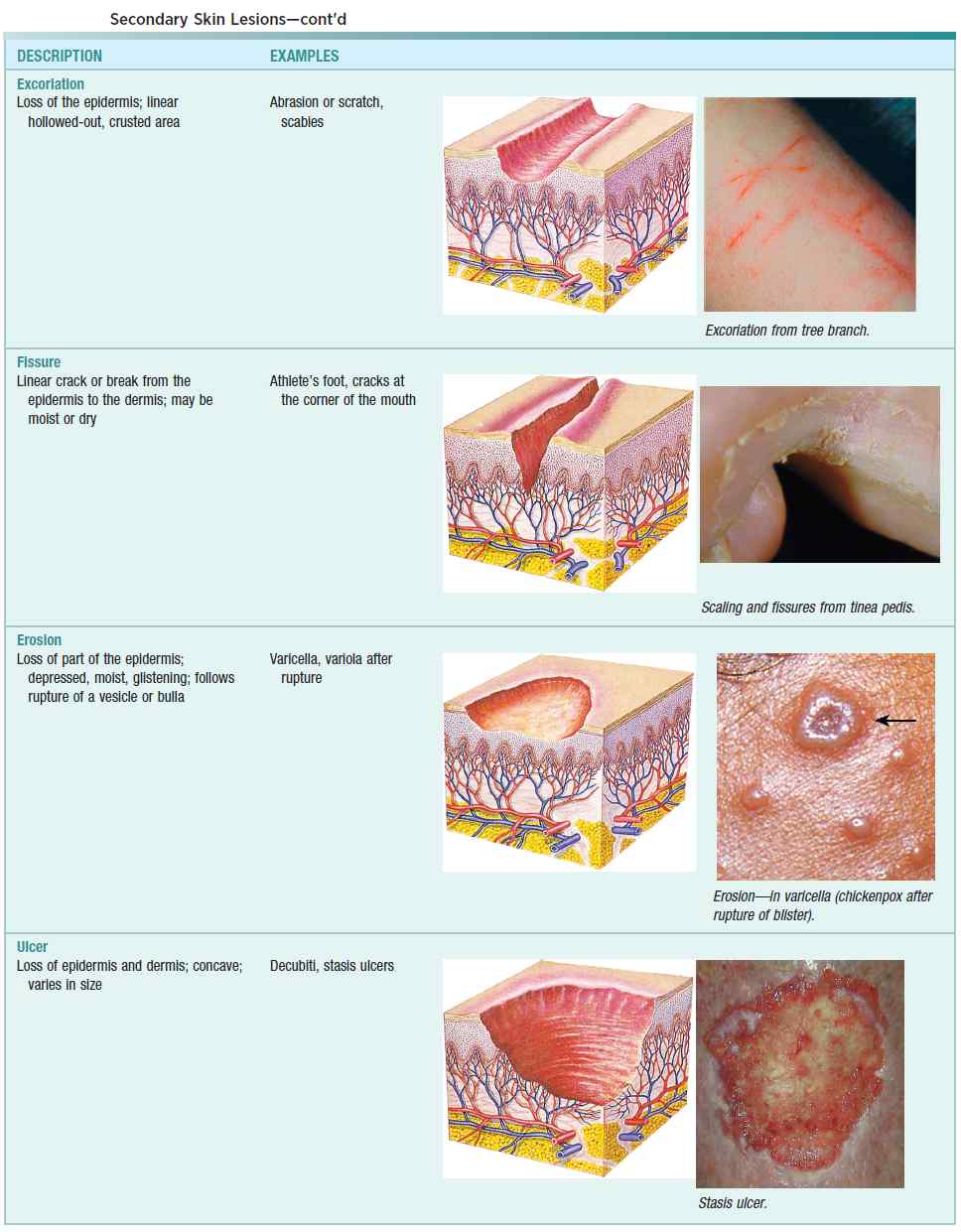
Erosive lesions
- Any vesicular dermatitis
- Impetigo
- Lichen planus
- Erythema multiforme
- Oral erosions
- Psychiatric disorders
Ulcerated lesions
- Decubiti: bed sores or pressure sores
- Herpes simplex
- Skin cancers
- Parasitic infections
- Syphilis: chancre
- Vasculitis
- Stasis
- Arterial disease
History in the Patient with Skin Rashes
The following long list of factors should be assessed when taking a history in the patient with skin rashes:
- Rash: onset, duration.
- Aggravating factors: physical or chemical agents; cold (cold urticaria or cryoglobulinemia); heat (worsens seborrheic conditions and superficial skin conditions).
- Precipitants: stress may lead to alopecia or eczema.
- Site of origin: contact dermatitis and pityriasis rosea (herald patch).
- Rate of progression.
- Timing of change in skin lesions, particularly for moles.
- Character: any alteration or progression in lesions.
- Hair and nails.
- Family history: eczema, psoriasis, inherited skin disorders.
- Infective agents: foreign travel (tropical infections), pets (papular urticaria or animal scabies).
- Farm animals: orf (poxvirus), ringworm.
- Occupation.
- Chemical exposure: at home or work, acting as antigens or direct irritants.
- Drugs taken: over-the-counter drugs, steroids may make the rash better (as in dermatitis) or worse (as in acne). How are the drugs being used?
- Foods: nuts and shellfish.
- Laundry detergent or soap.
- Contacts: family and friends.
- Light exposure: herpes simplex, SLE, and vitiligo.
- Hobbies: sportsmen are more prone to viral or fungal infections.
- General state of health and past medical history.
- Patient’s explanation for rash.
Systemic symptoms should be assessed and may take the following forms:
- Arthralgias, fever, malaise, fatigue, and weight loss should be considered danger signs and not taken lightly.
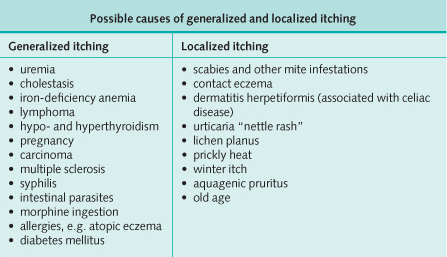
- Itching (image below): atopy or urticaria (e.g., scabies, which is worse in bed), eczema, dermatitis herpetiformis, lichen planus, flexural psoriasis.
- Pain: inflammatory conditions, skin tumors.
Finally, the mode of spread is significant and may take the form of an annular appearance (e.g., erythema annulare, erythema multiforme, and fungal infections) or irregular spread (e.g., pyoderma gangrenosum or malignancy).
Drug eruptions may mimic any inflammatory skin condition. They usually start abruptly and are a widespread, symmetrical, erythematous eruption. Constitutional symptoms such as malaise, arthralgia, headache, and fever may be present.
Examining the Patient with Skin Rashes
In the patient presenting with subcutaneous nodules, think of the following:
- Rheumatoid nodules
- Rheumatic fever
- Polyarteritis
- Xanthelasmata
- Tuberous sclerosis
- Neurofibromatosis
- Sarcoidosis
- Granuloma annulare
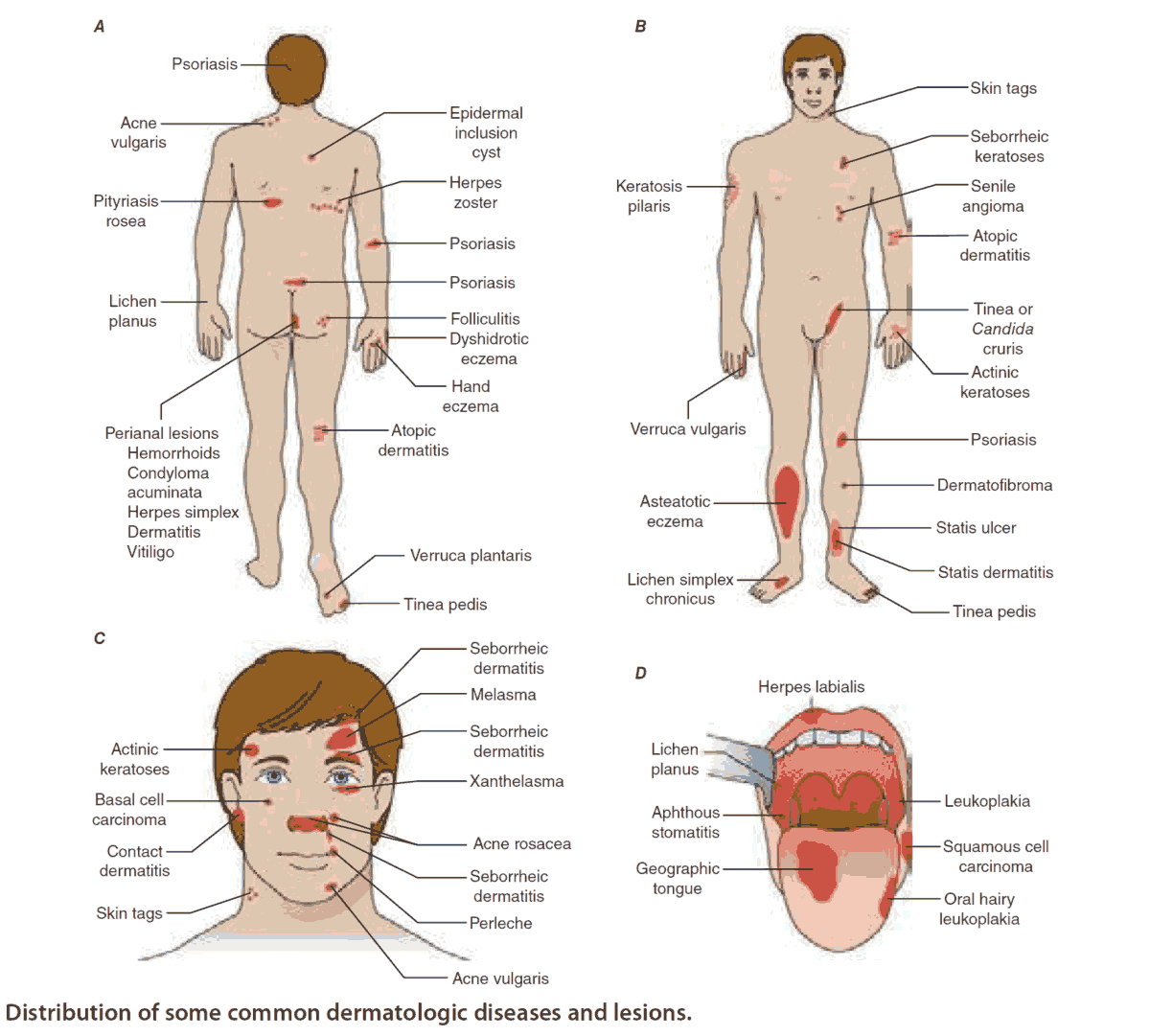
Always examine the entire skin and look in the mouth (e.g., with lichen planus, herpes simplex and zoster, and infective exanthemata). Rashes may change with time and become characteristic or diagnostic of common dermatoses, such as the infectious exanthemata. Look at the distribution of lesions:
- If widespread and symmetrical, suspect systemic disease.
- If only areas exposed to the sun are involved, suspect light sensitivity.
- Patterns involving a dermatome distribution suggest herpes zoster.
- Dermatitis involving the hands, face, axillae, ears, and eyelids suggests contact dermatitis.
- Dermatitis involving the axillae, groin, scalp, central chest and back, eyebrows, ears, and beard suggests seborrheic dermatitis.
- Dermatitis involving the popliteal and cubital fossae and the face suggests atopic dermatitis.
Describe the lesion:
- Bizarrely shaped lesions suggest that the cause is an external agent (e.g., caustic liquid, self-induced injury).
- Fungal infections are characterized by slow growth, a smooth outline, an active edge with a healing center, and asymmetry.
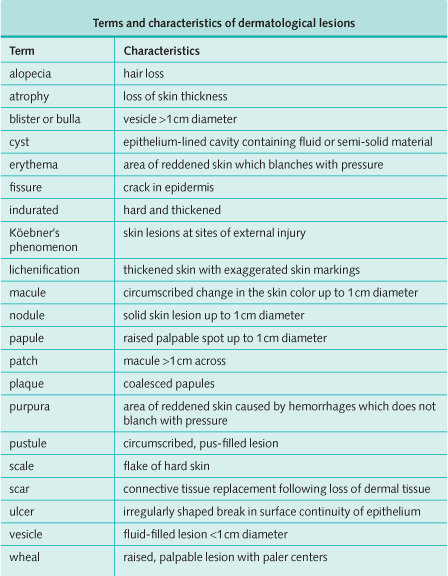
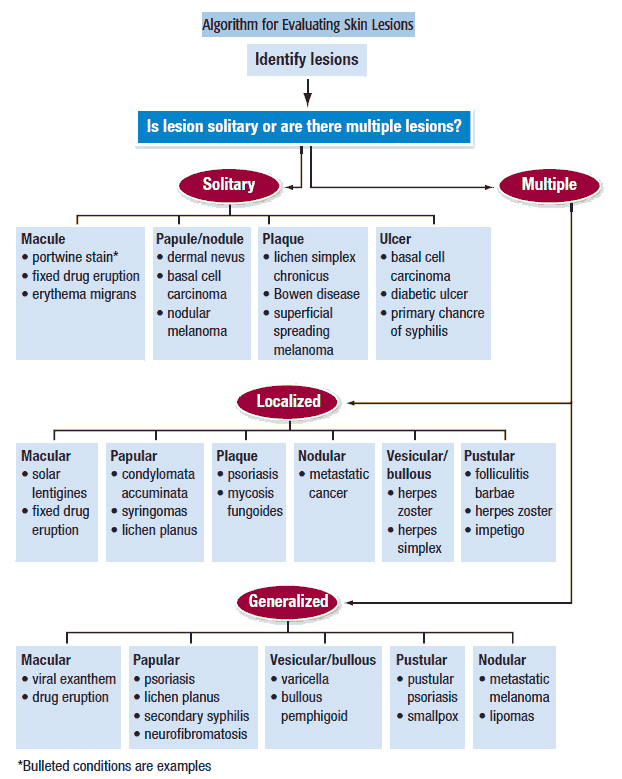
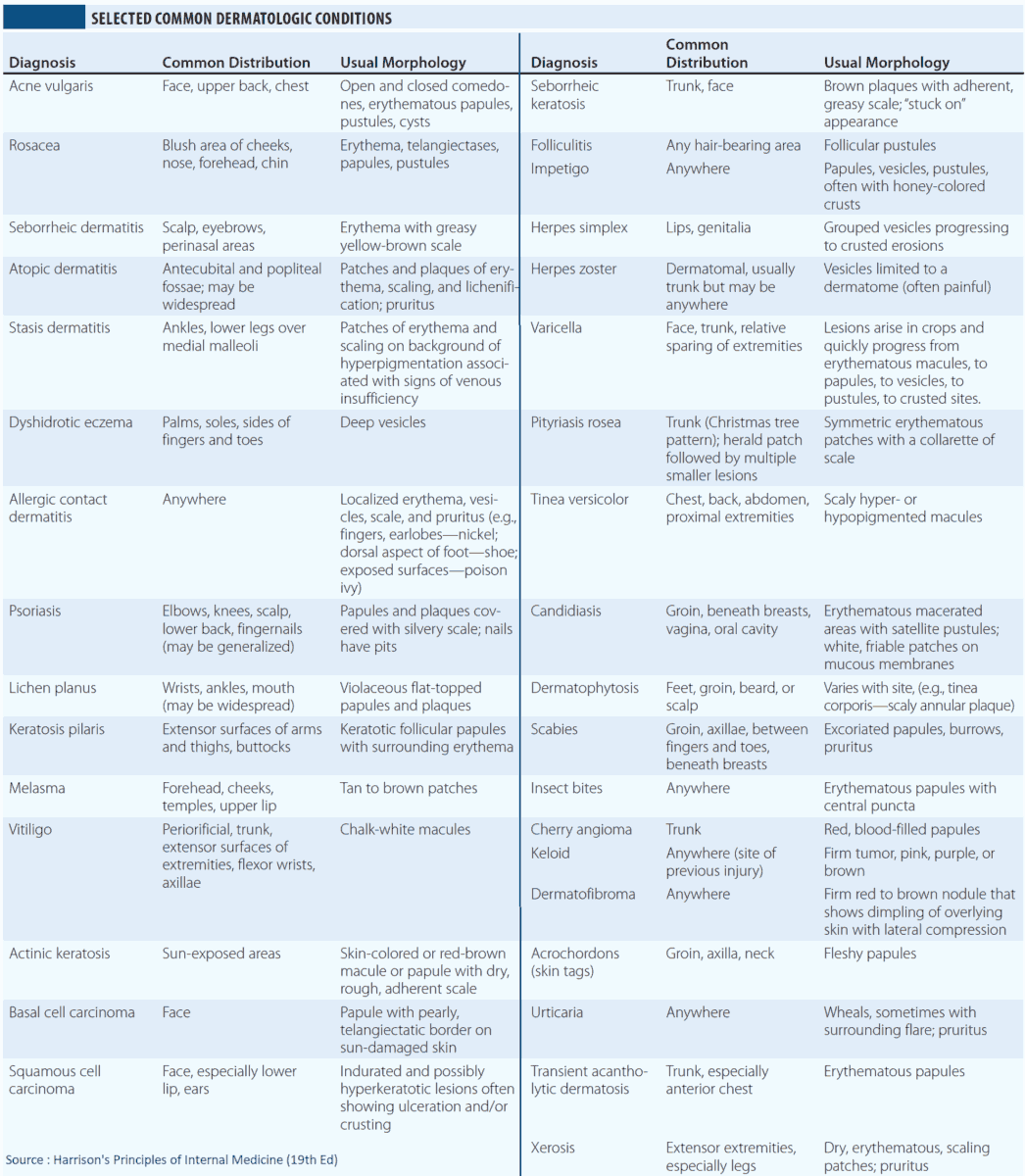
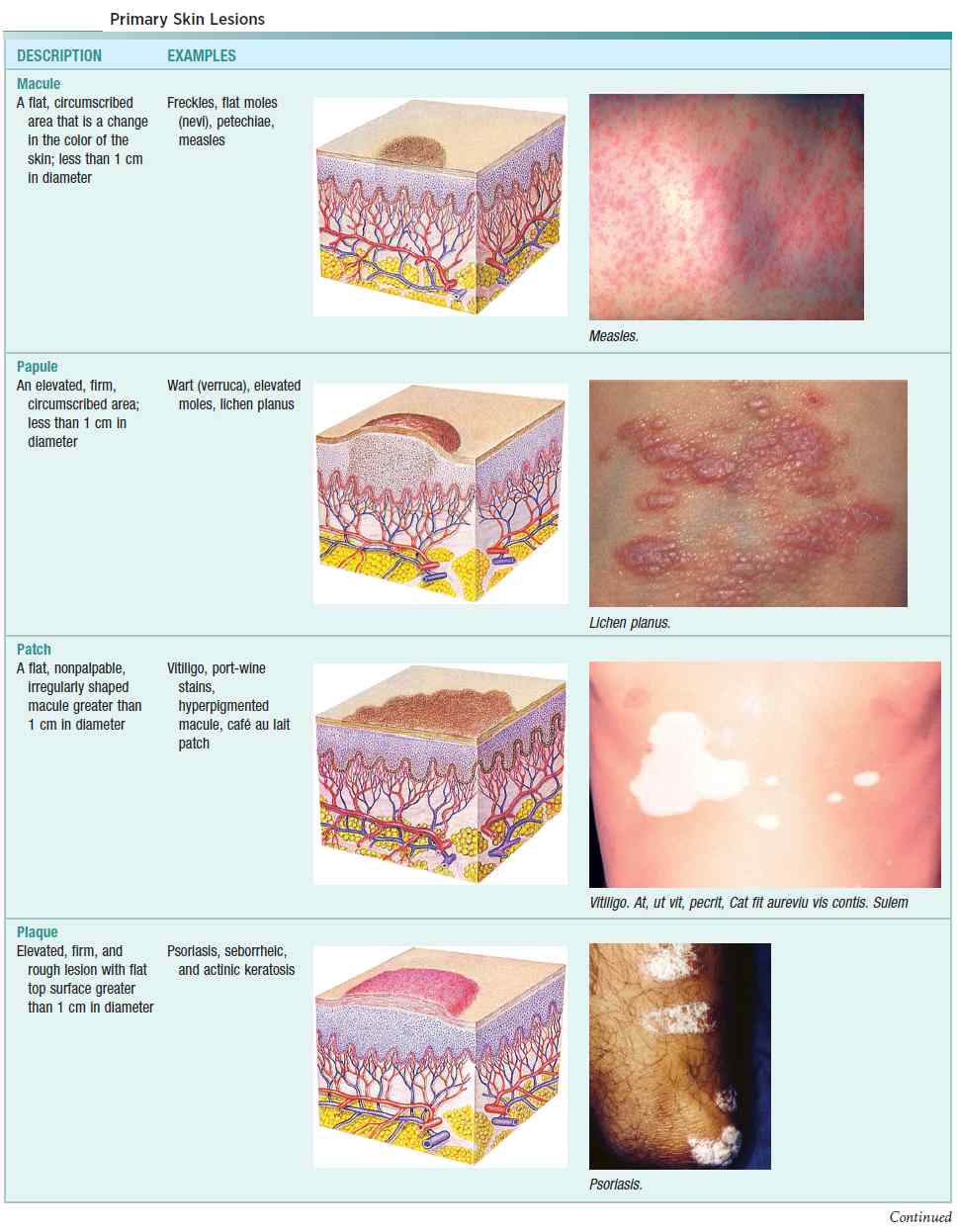
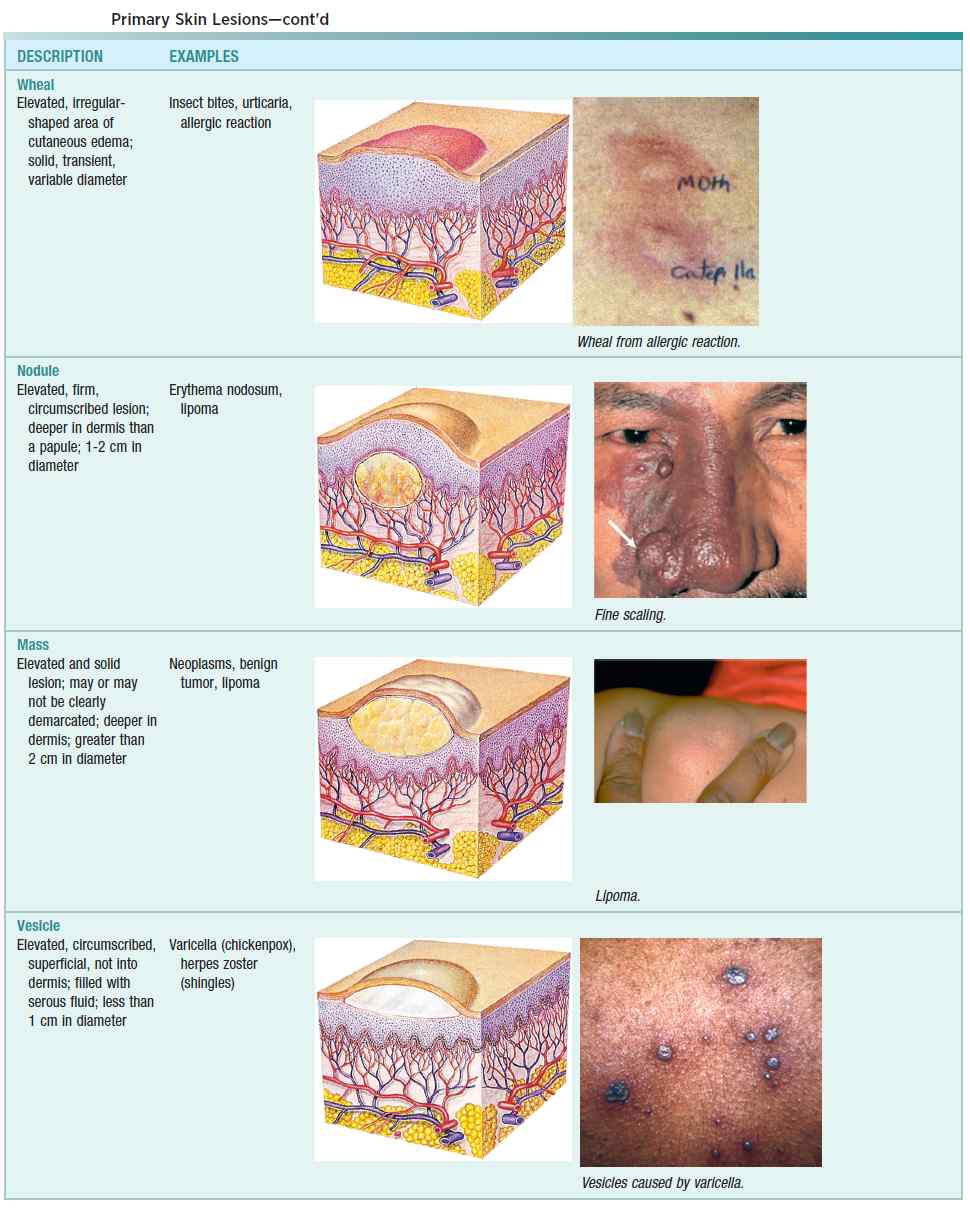
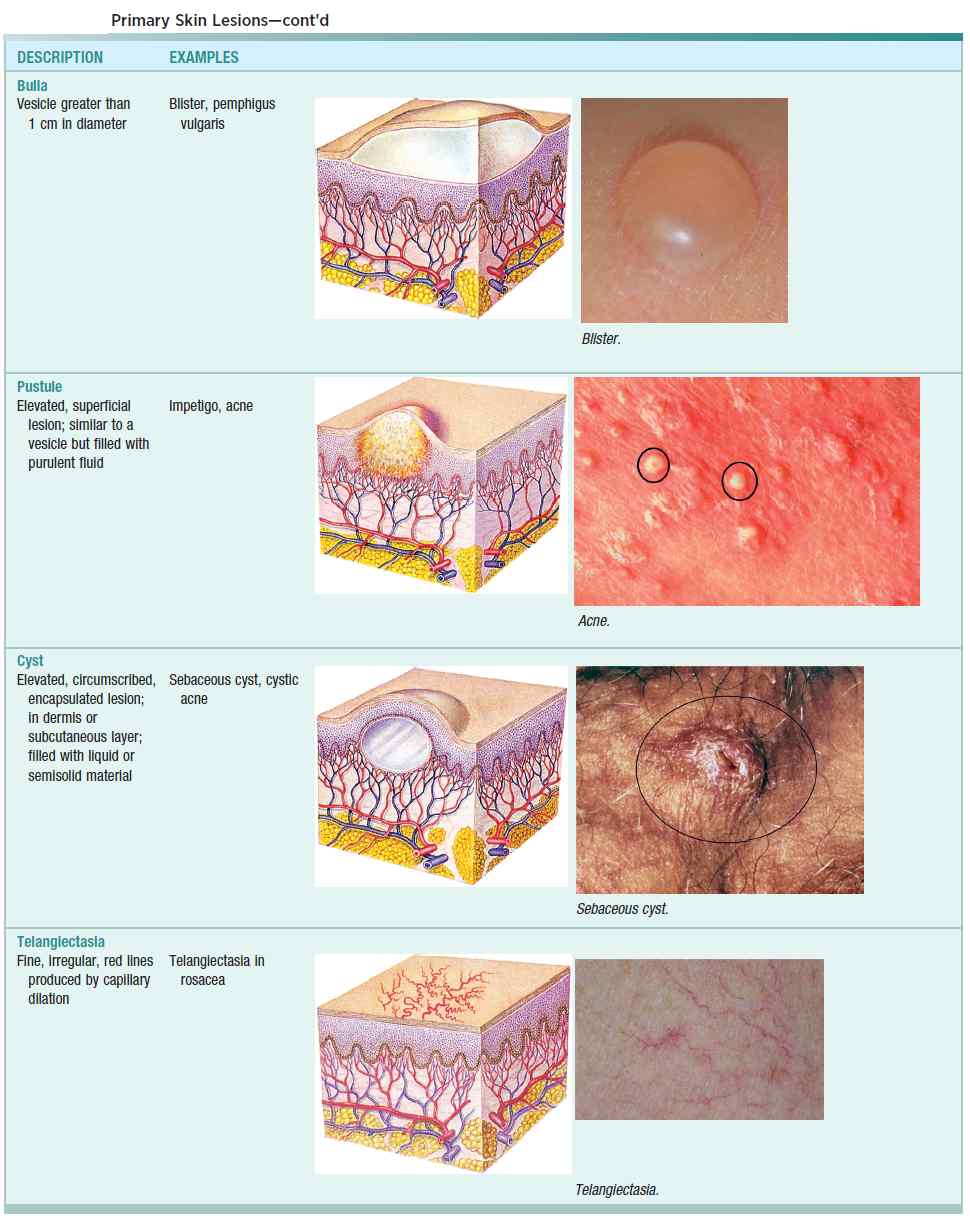
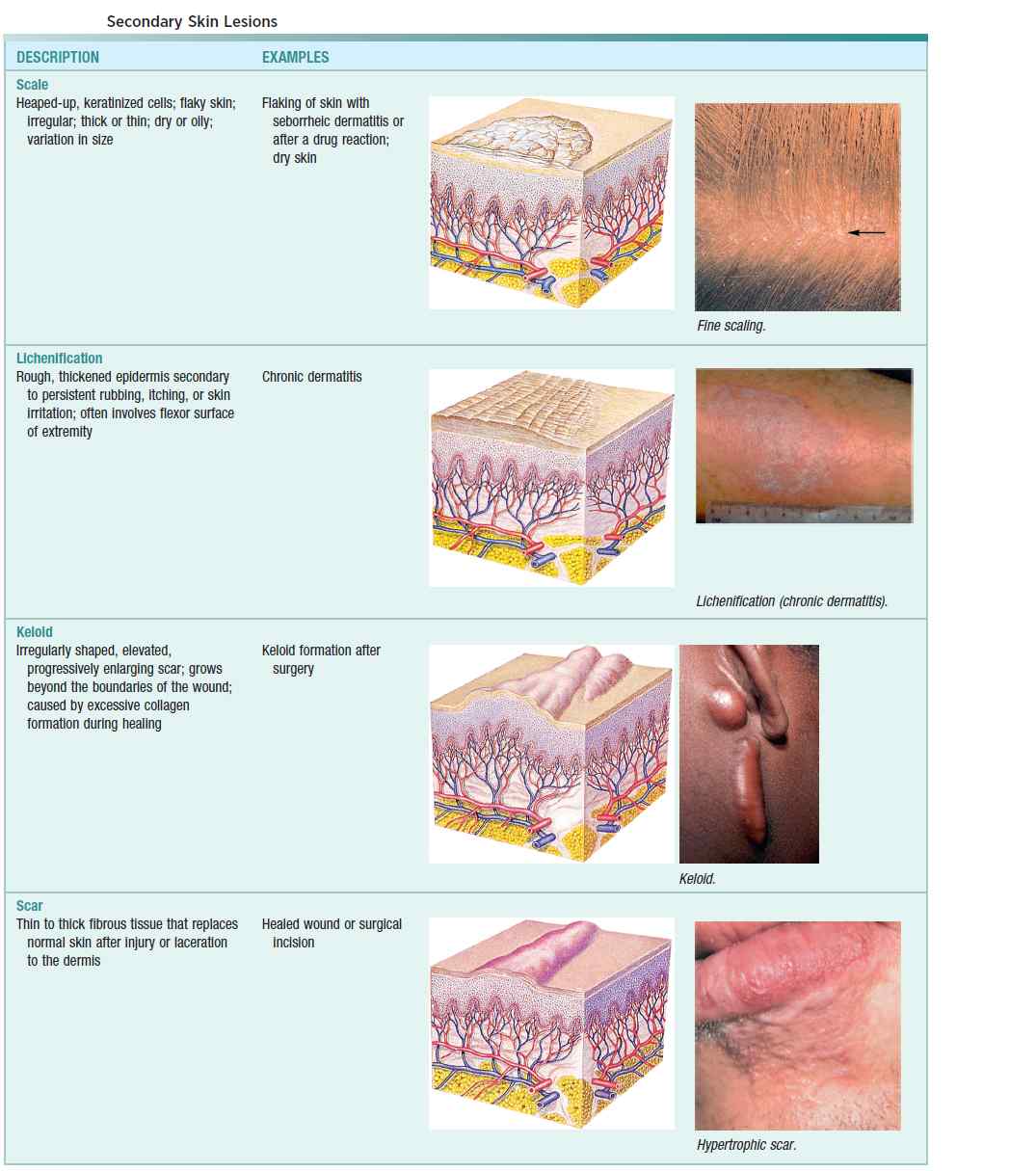
Terms and characteristics of dermatologic lesions are given in the image below.
For many skin lesions, multiple diagnoses may be possible. Often these diagnoses do not pose long-term complications, and topical steroids will be the treatment for both. Giving a trial of topical steroids with close follow-up is sometimes the best course of action.
Investigating the Patient with Skin Rashes
The history and examination may be enough to determine the diagnosis. If the patient is not unwell, it may be possible to examine for skin changes over time to allow for the development of possible characteristic lesions. The following investigations should be performed:
- Blood tests: complete blood count, urea and electrolytes, bacterial and viral titers with immunologic tests for tropical diseases if appropriate, and blood cultures.
- Skin scrapings and nail clippings: fungi.
- Examination of the skin under Wood’s light.
- Examination of brushings of household pets: mites.
- Culture of fluid-containing lesions.
- Skin biopsy.
- Biopsy of lesions in lymph nodes or other organs.
- Investigations for associated systemic diseases or malignancy.
Drug eruptions may mimic any inflammatory skin condition. They usually start abruptly and are a widespread, symmetrical, erythematous eruption. Constitutional symptoms such as malaise, arthralgia, headache, and fever may be present.