Table of Contents
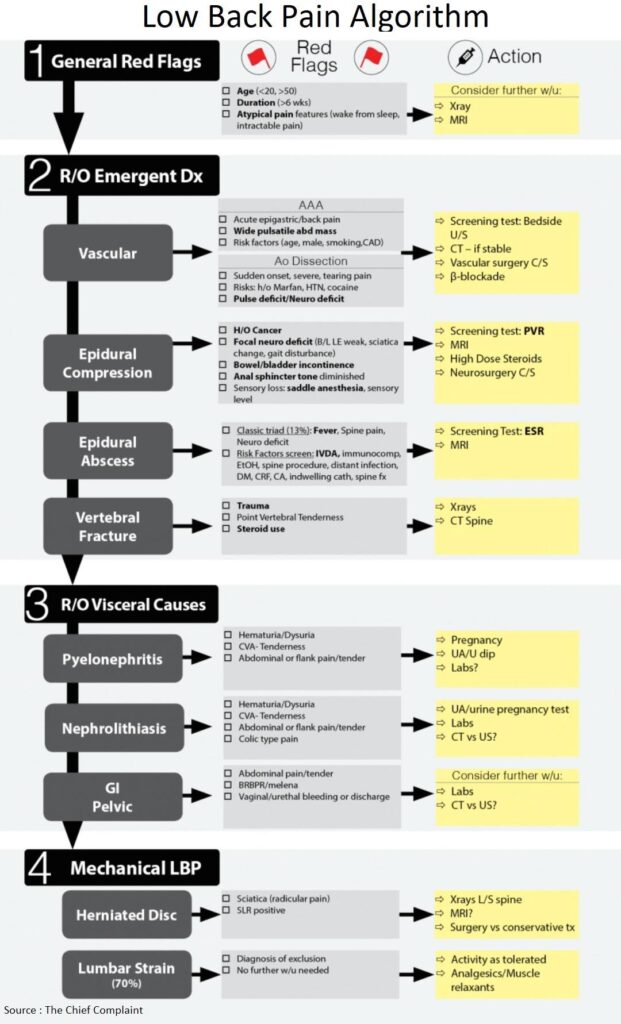
General Red Flags for Low Back Pain
General Approach
- Begin work-up by ruling out emergent/urgent conditions and evaluating/charting the absence of red flags that can signal the presence of an emergent condition
- Then consider other visceral causes of low back pain
- If no red flags are present and patient does not need further work-up, then the likely default diagnosis is benign mechanical (lumbar strain) LBP
Age
- <20 years old
- Increased incidence of congenital, developmental, bony abnormalities, and malignancy
- >50 years old
- Increased incidence of serious causes (AAA, vertebral fracture, pancreatitis…)
Duration of Symptoms
- Acute (0-6 weeks); Subacute (6-12 weeks); Chronic (>12 weeks), and recurrent
- Non acute (>6 weeks)
- Red flag because 80-90% symptoms should resolve by 4-6wks (Emerg Med Clin North Am 1999;17:877- 93)
Atypical pain features
- Awaken from sleep
- Intractable pain
- Consider: infection, tumor, fracture, nerve impingement, or non-musculoskeletal causes
Emergent Conditions of Low Back Pain
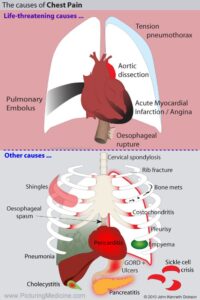
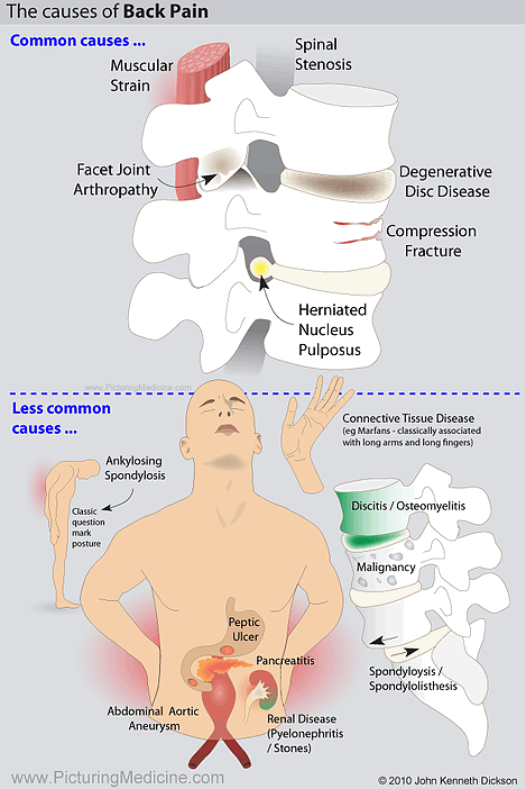
1. Abdominal Aortic Aneurysm (AAA) / Aortic Dissection
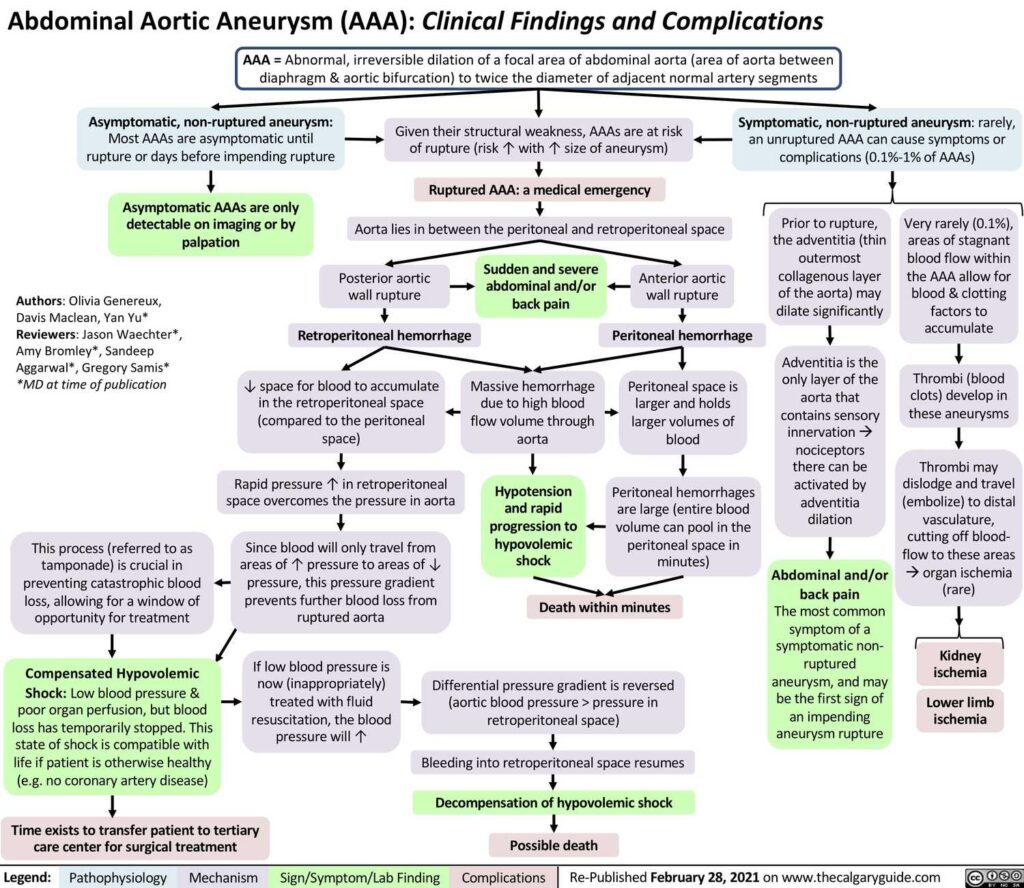
Abdominal Aortic Aneurysm (AAA)
- Presentation
- Usually asymptomatic until rupture
- Acute epigastric and back pain
- Wide pulsatile abdominal mass
- Renal colic mimic (back pain, hematuria)
- AAA Risk factors (age, male, smoking, CAD/PVD, Family History)
Aortic Dissection
- Presentation
- Sudden-onset, severe, “tearing” pain
- Pulse/neuro deficit
- New Aortic Insifficiency murmur
- Limb ischemia
- Risk factors: HTN (Hypertension), Marfan’s, vasculitis, pregnancy, coarctation, bicuspid aortic valve, trauma, cocaine/meth
2. Epidural Compression
Causes of Epidural Compression
- Spinal cord compression,
- Conus medullaris syndrome,
- Cauda Equina syndrome
Clinical Presentation of Epidural Compression
- History of cancer ?
- Multiple myotomes/dermatomes may be involved
- Focal Neurologic deficit:
- Bilateral Lower Extremity weakness, sciatica change, gait disturbance
- Bowel/bladder incontinence caused by urinary retention (PVR (post-void residual urine volume) >100-200ml)
- Decreased rectal tone
- Motor > Sensory loss
- Sensory loss: saddle anesthesia, sensory level
- Age (JAMA 1992;268;760-5)
- Age > 50 or history of Cancer or unexplained weight loss or failure of conservative therapy, Sensibility 100% for detecting metastasis to spine
Work-up for Epidural Compression
- Overflow incontinence
- Cause (J Bone Joint Surg Am 1986;68:386)
- Urinary retention (sensitivity 90%, specificity 95% for epidural compression)
- Abnormal PVR (post-void residual urine volume)
- Absence of large PVR (>100ml) has NPV (Negative predictive value) 99.99%
- In absence of significant neurologic deficit normal PVR rules out compression
- Post-void US: Volume = Length x Width x Height x (0.52)
- Anal sphincter tone diminished in 60-80%
- Saddle anesthesia has sensitivity 75%
- Cause (J Bone Joint Surg Am 1986;68:386)
- MRI
- Diagnose site of compression
Special Case: Patient with history of Cancer (Emerg Med Clin N Am 2010;28:811)
- Group I: New/progressive neurologic symptoms
- Steroids (Dexamethasone 10mg IV)
- Xrays, emergent MRI
- Group II: Stable neurologic symptoms
- Steroids
- Xrays, urgent MRI (24h)
- Group III: No neurologic signs/symptoms
- Conservative therapy
- Xrays, outpatient MRI
Treatment of Epidural Compression
- Emergent Neurosurgical Consult
- Steroids/Radiation if due to metastasis
3. Spinal Epidural Abscess (SEA)
Other infectious causes of low back pain
- Epidural abscess
- Osteomyelitis
- Discitis
- Transverse Myelitis
Clinical Presentation of Spinal Epidural Abscess
Spinal Epidural Abscess (SEA) Triad
Fever
Spine pain
Neurologic deficit
- Classic Triad (Fever, Spine pain, neuro deficit)
- Triad present in only 13% patients with SEA and is usually a late finding
- Must consider risk factor screening for rulling out epidural abscess. (J Emerg Med 2004;26:285-91)
- Progression of symptoms:
- Back pain → Radiculopathy → Sensory changes/motor weakness → Bowel-bladder dysfunction → Paralysis
- Risk Factors:
- Intravenous drug abuse
- immunocompromised
- alcohol abuse
- spine procedure
- distant infection
- Diabetes Mellitus
- Chronic Kidney Failure (CKD)
- Cancer
- indwelling catheter
- spine fracture
- Risk factor screening sensitivity 98%, for one or more risk factors
Work-up for Spinal Epidural Abscess
- ESR (Erythrocyte sedimentation rate) (J Neurosurg Spine 2011;14:765-770)
- Used as screening test for value of >20mm/h (sens 100%)
- Useful as screening tool for ED patients with spine pain, risk factor for Spinal Epidural Abscess and no neurologic deficits
- Emergent MRI
Treatment of Spinal Epidural Abscess
- Broad spectrum antibiotics (Staph/Strep/gm neg)
- Emergent Neurosurgical consultation
4. Vertebral Fracture
Clinical Presentation of Vertebral Fracture
- Usually elderly with osteoporosis
- Trauma
- Point Vertebral Tenderness
- Steroid use
- A person with Lower Back Pain on long-term steroids is considered to have a compression fracture until proven otherwise (Spec 99%)
Work-up for Vertebral Fracture
• Xrays / CT Spine
Visceral Causes of Low Back Pain
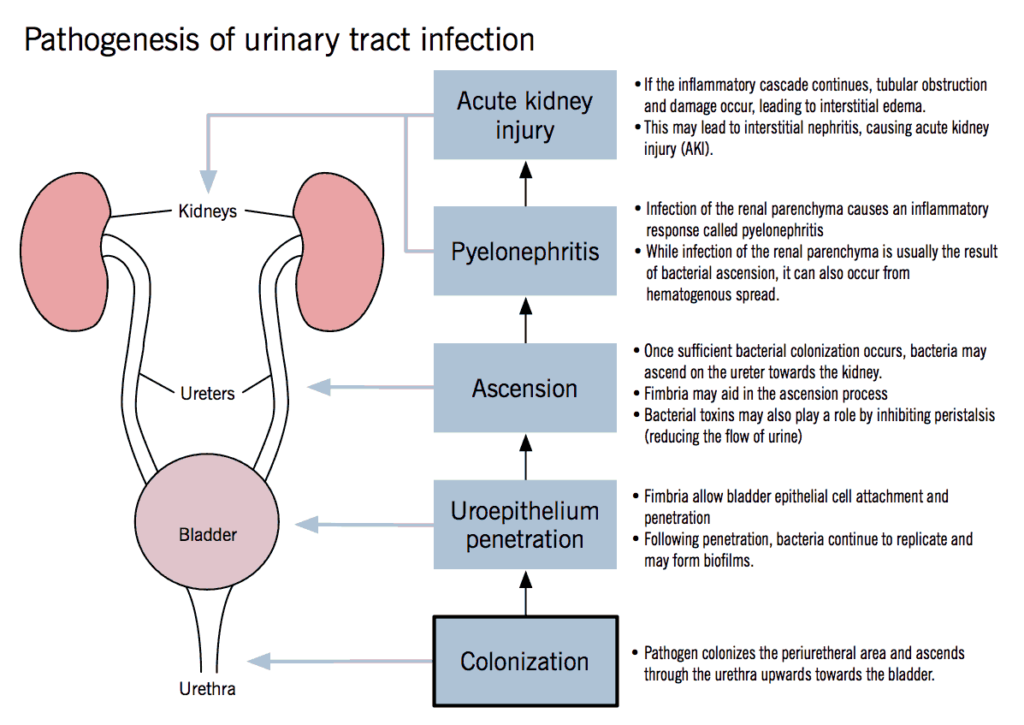
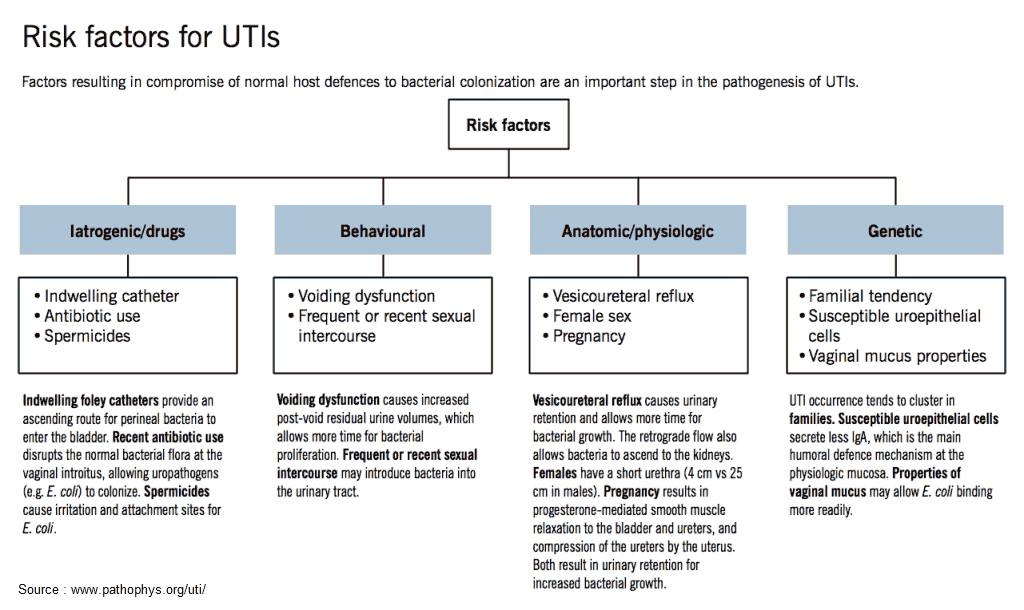
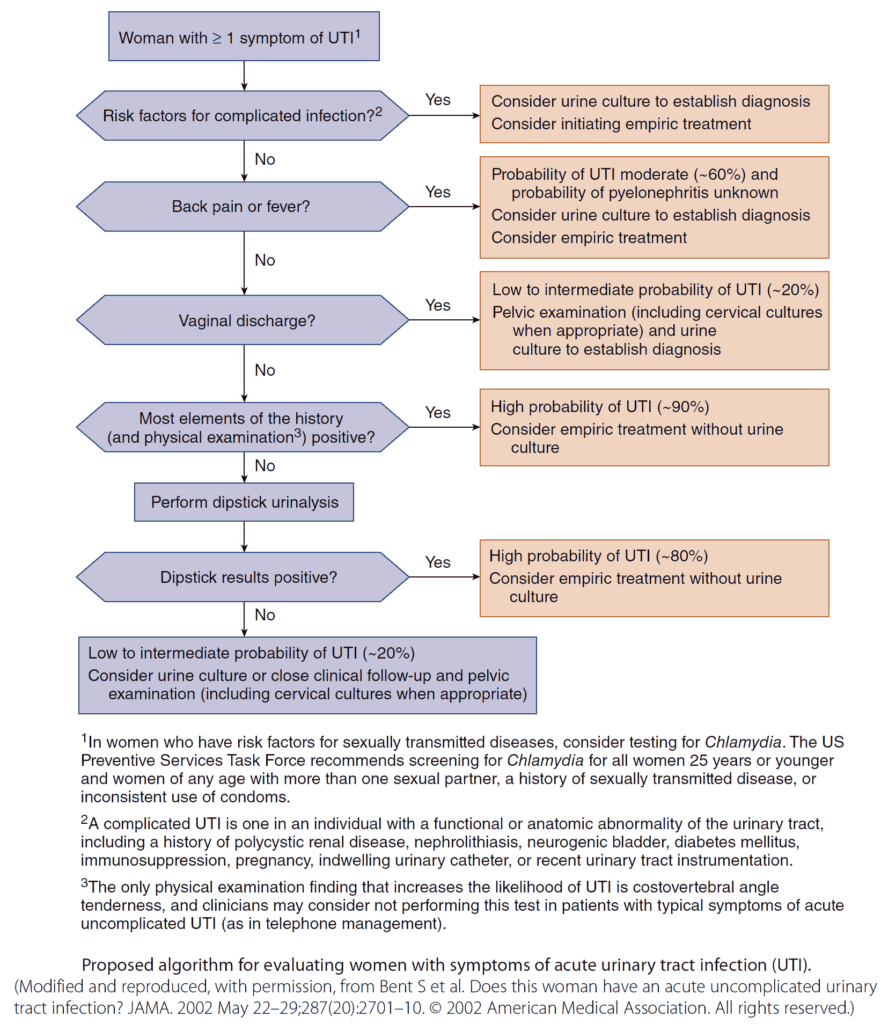
1. UTI / Pyelonephritis
Definitions
- Uncomplicated UTI: young, healthy, non-pregnant women with structurally and functionally normal urinary tracts
- Complicated UTI: UTI associated with an underlying condition that increases the risk of failing therapy
- Complicated pyelonephritis: progression of upper UTI to emphysematous pyelonephritis, renal corticomedullary abscess, perinephric abscess, or papillary necrosis
Risk Factors for Complicated UTI
□ Pregnancy
□ Diabetes
□ Male gender
□ Immunosuppression (AIDS, chemotherapy…)
□ Functional GentioUrinay abnormality (catheter, neurogenic bladder…)
□ Structural GU abnormality (stones, fistula, PCKD, transpant…)
Clinical Presentation
- Cystitis
- Urinary frequency and urgency, dysuria, and hematuria
- Suprapubic pain, low back pain
- New or increased incontinence in older patients or Altered Mental Status / Delirium
- Pyelonephritis
- Flank or abdominal pain, CVA (costovertebral angle) tenderness on exam
- Fever/chills, Nausesa / Vomitus
- Complicated Pyelonephritis (Sepsis, Renal failure)
Diagnosis
- Urine Dipstick / Urine Analysis (UA)
- Either nitrite OR leukocyte esterase (LE) positive: 75% sensitive, 82% specific
- Nitrite AND leukocyte esterase positive: 35-84% sensitive, 98-100% specific
- Nitrite alone (95-98%) more specific than leukocyte esterase alone (59-96%) but S. saprophyticus, pseudomonas, and enterococci do not reduce nitrate
- False positive LE (leukocyte esterase) with vaginitis or cervicitis
- Pyuria and bacteruria may be absent if obstruction of the collecting system or ureters is present
- Urine Microscopy
- White blood cell casts are diagnostic of upper urinary tract infection
- Urine culture
- Helpful in guiding antibiotic therapy in pyelonephritis or failed antibiotic treatment
- Positive: single organism isolated with ≥ 100,000 CFU
- Imaging
- Not routinely necessary
- CT abdomen/pelvis with/without IV contrast consider to/if :
- rule out infected/obstructed ureteral stone
- rule out pyelonephritis complication (abscess…):
- Consider if failure of response to therapy in 48-72 hours
- Recurrence of symptoms within a few weeks of therapy
- Suspicion for obstruction, gas, hemorrhage, masses
- Ultrasound:
- Rule out hydronephrosis / obstruction / stone
Treatment
- Antibiotics
- Base antibiotic selection on previous culture data, local resistance patterns, patients history and medical problems
- Adjunctive pain control option: Phenazopyridine PO TID (urinary analgesic).
- See Current Guidelines (Clinical Infectious Diseases 2011;52(5):e103)
Complications
- Pyonephrosis
- Infection + obstruction (pus under pressure)
- Pyelonephritis with an obstructing stone, mass, or other obstruction
- Therapy: emergent urology/interventional radiology consult for percutaneous nephrostomy tube or stenting
- Renal abscess
- Diagnosis: CT with IV contrast; can be visualized on Ultrasound
- Therapy: Resuscitation, antibiotics, percutaneous drainage (depending on size and response to antibiotics)
- Emphysematous UTI
- Definition: necrotizing infection with gas formation in bladder (cystitis), renal pelvis (pyelitis) or kidney parenchyma (pyelonephritis)
- High mortality (20% to 40%) even with treatment
- 95% of cases occur in patients with DM
- Major risk factor is infected obstructing stone
- Papillary necrosis
- Definition: coagulative necrosis of the renal medullary pyramids and papillae
Disposition
- Outpatient therapy appropriate if:
- Uncomplicated pyelonephritis
- Normal vitals, normal renal function, no urinary obstruction
- Pain control and hydration status adequate
- Able to tolerate Oral medications
2. Renal Colic
Clinical Presentation of Renal Colic
- Renal colic
- Mechanism of Action: obstruction of urinary tract → ↑ pressures → renal capsular distention (visceral pain/N/V) → ↑ peristalsis of ureter (colicky pain)
- Unilateral flank pain → radiating to groin
- Migration of pain (depending on location of stone):
- Back pain → flank pain → lower quadrant abdominal pain → penile / labial / testicular pain
- Colic pain: intermittent, waxes/wanes, patient writhing, unable to sit still
- Urinary symptoms: urgency, frequency, dysuria, gross hematuria
- Nausea/vomiting
- Physical Exam : CVA (costovertebral angle) tenderness or lower abdominal tenderness
Diagnosing Renal Colic
- Urinalysis
- Microscopic hematuria only 85% sensitive for urolithiasis
- Use to rule-out infection/UTI and infected stone
- UA negative?: Patient may still have urine infection proximal to obstructing stone
- KUB (kidney, ureter, and bladder X-ray)
- 85-90% of stones are radioopaque (calcium, struvite, cystine) but KUB only 40-62% sensitive and 60-67% specific
- Little diagnostic utility; consider in patient with known history of radiopaque stones and typical presentation
- Ultrasound
- Ureteral calculi
- Sensitivity 45% and specificity 94%
- More likely to see larger stones (>4mm), at the UVJ (ureterovesical junction), or proximal near the renal pelvis.
- Hydronephrosis
- Sensitivity 85-90% and specificity 90-100%
- Not visualize stone itself but can demonstrate obstructive sequelae
- Presence/absence of hydronephrosis is neither diagnostic nor prognostic
- Preferred initial test in pregnancy, children → no radiation
- Use to evaluate abdomen/pelvis for alternative diagnoses (gallstones, appy etc…)
- Ureteral calculi
- CT (Non-contrast):
- Study of choice to evaluate urolithiasis
- Indications:
- 1st time diagnosis of urolithiasis
- Atypical presentation
- Rule out infection
- Not improving with conservative treatment
- Sensitivity 96-98% and specificity ~100%
- Useful in prognosis (size/location of stone, obstruction/hydronephrosis, perinephric stranding)
- No imaging ?:
- Pt with known kidney stone, typical presentation, well appearing, no risks for complications and good follow/up
- May treat empirically (pain control, hydration)
Treatment of Renal Colic
- Conservative treatment
- Pain control, hydration, expectant stone passage.
- NSAIDs
- Inhibits prostaglandin-mediated process in urolithiasis
- As effective as opioids and fewer side effects of nausea and vomiting
- Ketorolac IV or Ketorolac + Opiate combination
- Opiates
- In addition to NSAID or if contraindications to NSAID
- Hydration & Diuresis
- No evidence that increased hydration or forced diuresis improves pain scores or rate of passage ⇒ Use: replete volume in dehydrated patients or those with elevated creatinine only
- Medical Expulsion Therapy:
- CCBs (e.g nifedipine) or α-antagonists (e.g. tamsulosin)
- Mechanism of Action: relax ureteral smooth muscle → allow passage of stone
- Conclusion: Trial of tamsulosin (0.4 mg qd x4 weeks) in stones <10mm is reasonable
- Emergent urology consult
- Urosepsis, obstruction with proximal infection, AKI, anuria, intractable pain/vomiting, stones >10mm
- Renal Stents
- Use:
- Facilitate drainage of upper urinary tract and relieve obstruction
- Temporizing while await stone passage or definitive urological procedure.
- Complications: pain, hematuria, urgency and frequency (more common), upward migration, infection, sepsis (rare)
- Use:
- Infected kidney stone
- Treatment: decompression, emergently by urology or IR
- Admission, hydration, IV antibiotics
- UTI + non-obstructing stone: if well appearing, outpatient antibiotics, urology follow-up
| Size of stone | Rate of passage |
| 1 mm | 87 % |
| 2-4 mm | 76 % |
| 5-7 mm | 60 % |
| 7-9 mm | 48 % |
| >9 mm | 25 % |
Disposition
- Admit
- Obstructing stone with a proximal infection, urosepsis, acute renal failure, anuria, or intractable pain, nausea, or vomiting
- Urology consult
- Discharge Home
- Stable, tolerating po, pain controlled, nausea/vomiting controlled, outpatient urology follow-up
- Outpatient Urology follow-up:
- Stone >10mm, failure to pass stone after conservative treatment, pain not controlled
Journal Club: Tamsulosin in ureteral stones
RCT (Arch Intern Med 2010;170:2021)
- Study: multicenter, placebo-controlled, randomized, double-blind study of tamsulosin vs placebo (good)
- No difference in expulsion delay within 42 days; (P = .30)
- No difference in surgical procedure or other secondary end points between groups
- Conclusion: “Tamsulosin did not accelerate the expulsion of distal ureteral stones in patients with ureteral colic”
Systematic review (Ann Emerg Med. 2007;50:552)
- Previous review suggested increase stone passage rate and decreased time to stone passage with tamsulosin
- Critique: Review had poor quality, unblinded studies, poor follow up
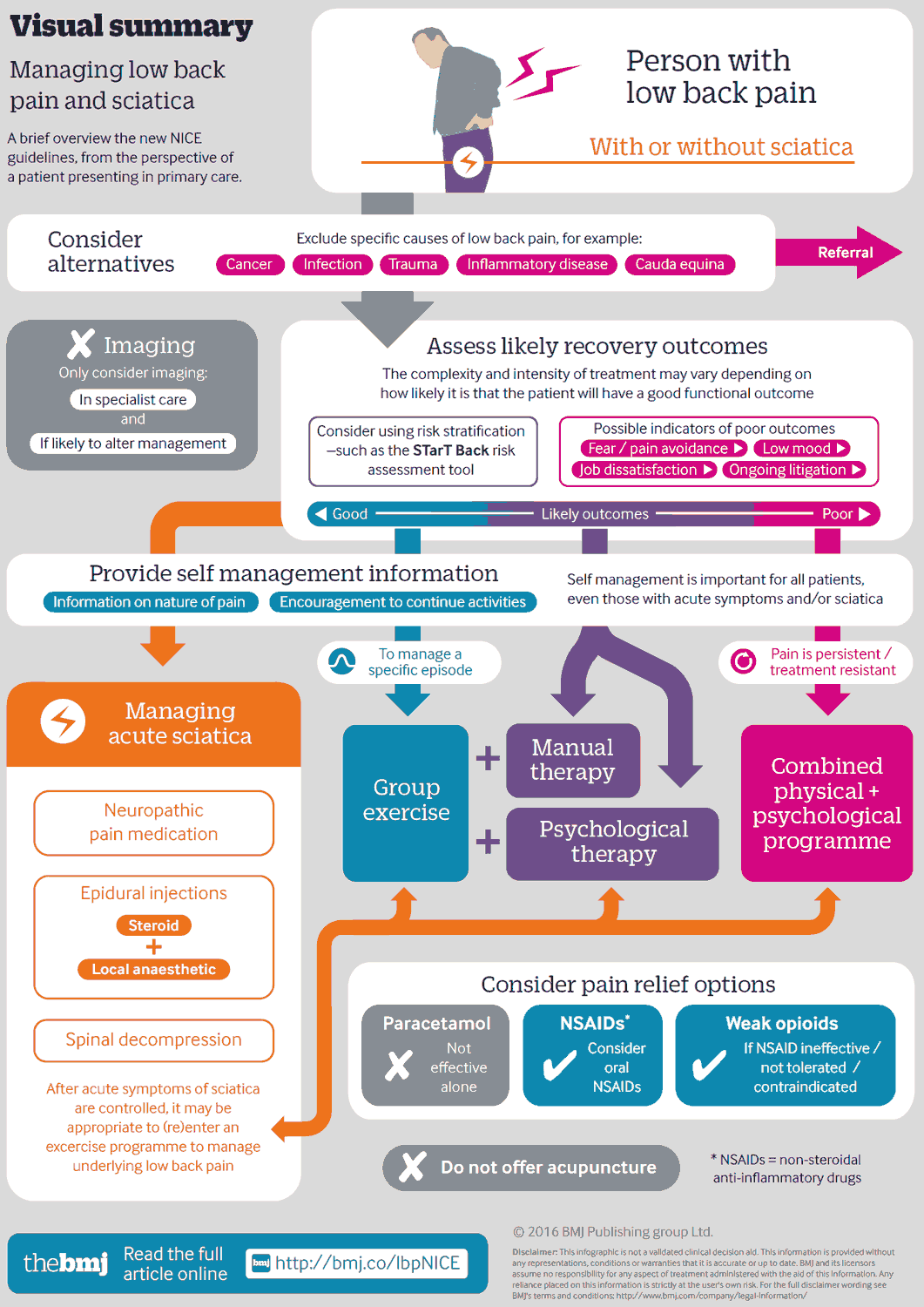
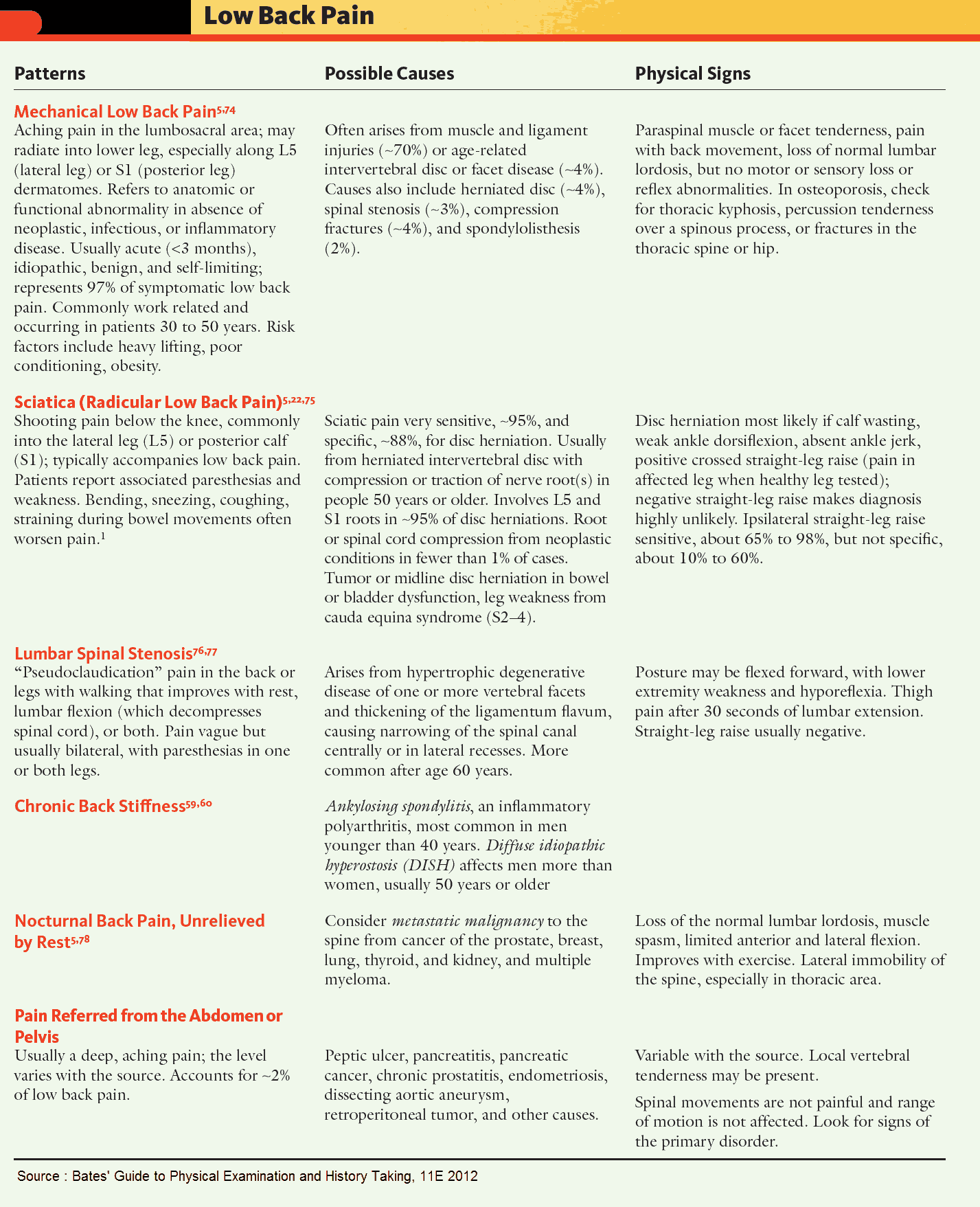
Mechanical Low Back Pain
1. Sciatica (ischialgia)
Definition
- Peripheral radiculopathy caused by compression of nerve root, usually caused by disc herniation or spinal stenosis
Clinical Presentation of Sciatica
- Back pain + neuropathy (paresthesia, sensory loss) down one leg
- Unilateral symptoms that extend distal to knee
- Sensory > Motor
- Single myo/dermatome involved
- SLR (Straight leg raise) called Lasègue test or Lazarević’s sign
- Pain when the straight leg is raised to an angle of between 30 and 70 degrees
- Pain must extend below knee
- Sensitivity 91%, Specificity 26% (Spine 25 (9): 1140–7)
- Crossed SLR: Raising the opposite leg causes pain on affected side (sensitivity 29%, specificity 88%)
Treatment of Sciatica
- 90% of acute sciatica responds to conservative treatment
- Conservative management: Tylenol / NSAIDS / continue daily activities
- Treat similar to lumbar strain except consider Xrays to rule out other causes of nerve compression (tumor, fracture, spondylolisthesis, infection…)
- Emergent/Urgent Surgery
- Significant motor deficit (foot drop, unable to ambulate)
- Intractable pain
- Indications for outpatient surgery
- Definite herniation on imaging study +
- Corresponding pain syndrome +
- Corresponding neurologic deficit +
- No response to 4-6 weeks conservative treatment
2. Lumbar Strain
General
- Diagnosis of exclusion
- No further work-up needed
Treatment
• Activity as tolerated
• Analgesics / Muscle relaxants
• Continuing normal daily activities as tolerated leads to more rapid recovery than either bed rest or back immobilizing exercises (NEJM 1995;332(6):351-5)
References:
- Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emerg Med Clin North Am. 2010 Nov;28(4):811-39. doi: 10.1016/j.emc.2010.06.001. Epub 2010 Aug 4. PMID: 20971393. https://pubmed.ncbi.nlm.nih.gov/20971393/
- Della-Giustina DA. Emergency department evaluation and treatment of back pain. Emerg Med Clin North Am. 1999 Nov;17(4):877-93, vi-vii. doi: 10.1016/s0733-8627(05)70102-4. PMID: 10584107. https://pubmed.ncbi.nlm.nih.gov/10584107/
- Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992 Aug 12;268(6):760-5. PMID: 1386391. https://pubmed.ncbi.nlm.nih.gov/1386391/
- Kostuik JP, Harrington I, Alexander D, Rand W, Evans D. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986 Mar;68(3):386-91. PMID: 2936744. https://pubmed.ncbi.nlm.nih.gov/2936744/
- Davis DP, Wold RM, Patel RJ, Tran AJ, Tokhi RN, Chan TC, Vilke GM. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004 Apr;26(3):285-91. doi: 10.1016/j.jemermed.2003.11.013. PMID: 15028325. https://pubmed.ncbi.nlm.nih.gov/15028325/
- Davis DP, Salazar A, Chan TC, Vilke GM. Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain. J Neurosurg Spine. 2011 Jun;14(6):765-70. doi: 10.3171/2011.1.SPINE1091. Epub 2011 Mar 18. PMID: 21417700. https://pubmed.ncbi.nlm.nih.gov/21417700/
- Lane DR, Takhar SS. Diagnosis and management of urinary tract infection and pyelonephritis. Emerg Med Clin North Am. 2011 Aug;29(3):539-52. doi: 10.1016/j.emc.2011.04.001. PMID: 21782073. https://pubmed.ncbi.nlm.nih.gov/21782073/
- Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE; Infectious Diseases Society of America; European Society for Microbiology and Infectious Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar 1;52(5):e103-20. doi: 10.1093/cid/ciq257. PMID: 21292654. https://pubmed.ncbi.nlm.nih.gov/21292654/
- Lu Z, Dong Z, Ding H, et al. Tamsulosin for ureteral stones: a systematic review and meta-analysis of a randomized controlled trial. 2012. In: Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK109618/
- Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007 Nov;50(5):552-63. doi: 10.1016/j.annemergmed.2007.05.015. Epub 2007 Aug 3. PMID: 17681643. https://pubmed.ncbi.nlm.nih.gov/17681643/
- Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007 Jun 23;334(7607):1313-7. doi: 10.1136/bmj.39223.428495.BE. PMID: 17585160; PMCID: PMC1895638. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1895638/