This article is an answer to the ECG Case 163
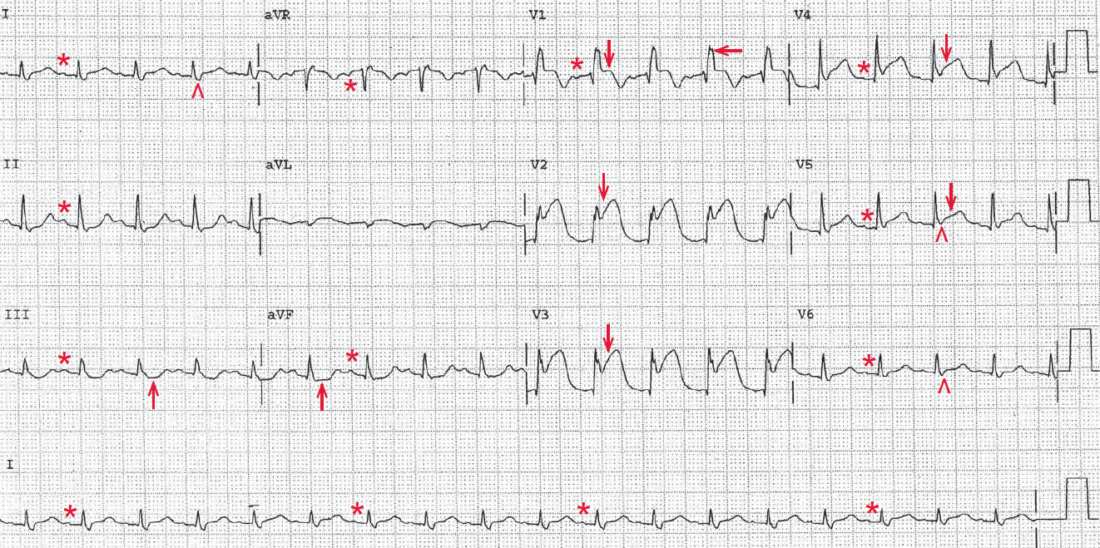
There is a regular rhythm at a rate of 110 bpm. There is a P wave (*) before each QRS complex, and the PR interval is stable (0.16 sec). The P wave is upright in leads I, II, aVF, and V4-V6 and negative in lead aVR. The P-wave morphology is normal. This is a sinus tachycardia.
The QRS complex duration is increased (0.12 sec), and there is a pattern of a right bundle branch block (RBBB) with an RSR′ complex (←) in lead V1 and broad S waves (^) in leads I and V5-V6.
There is significant ST-segment elevation (↓) in leads V1-V5, and also less significant ST elevation in leads I and aVL. The ST-segment morphology is no longer concave but is now convex and merges with the T wave. Also noted are minimal ST-segment depressions in leads III and aVF (↑); these are reciprocal changes. Hence this is an acute anterolateral wall ST-segment elevation myocardial infarction (STEMI) involving the septum and apex of the left ventricle.
This patient likely has a chronic RBBB on the basis of his known COPD. However, an RBBB can also develop acutely in the context of an MI that involves the intraventricular septum. A large anterior MI can disrupt the path of the right bundle, although this is uncommon.
More often, acute anteroseptal MI results in a left bundle branch block. When an RBBB occurs as a result of an MI, the degree of myonecrosis is usually extensive and the prognosis is poorer. Occasionally, an RBBB reflects acute right ventricular dilation and pressure overload in the context of heart failure with elevated left ventricular filling pressures and pulmonary hypertension.
An acute STEMI is treated with prompt revascularization, with either a thrombolytic agent or percutaneous coronary intervention (ie, stenting), which should optimally be performed within 90 minutes of symptom onset. This depends largely on the time it takes for the patient to present to the emergency room.