This article is an answer to the ECG Case 167
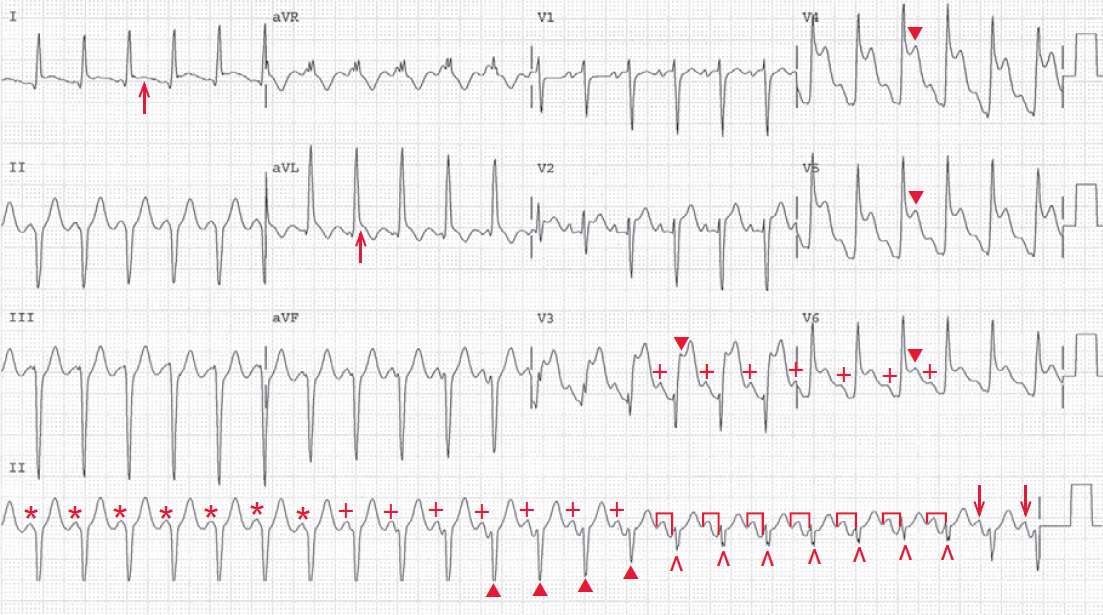
The shows a regular rhythm at a rate of 140 bpm. In the initial portion of the ECG (first 14 QRS complexes), there are regular QRS complexes, each with a duration of 0.12 second.
Although there are no P waves seen in the beginning of the ECG, P waves (+) become obvious by the eighth QRS complex in the rhythm strip. Indeed, there are P waves in the first 7 QRS complexes, which are superimposed at the beginning of the QRS complex (*).
It should be noted that the PR interval gradually increases as the QRS complex duration decreases and changes in morphology. By the fifteenth through the twenty-first QRS complex, there is a stable PR interval (┌┐) (0.16 sec) and a stable QRS morphology (^).
The last two QRS complexes have a P wave before them (↓), but the PR is slightly shorter, the QRS complex morphology is slightly different, and the QRS complex duration is increasing. Hence there is evidence of AV dissociation present with a wide QRS complex.
The changing morphology and duration of the QRS complex that occurs as the PR interval lengths suggests that these are fusion beats (especially complexes 11–14 [▲] where the QRS complex morphology is intermediate between the wide ones and the captured complexes), while the fifteenth through the twenty-first QRS complexes are captured. At the end, there is again fusion (last two QRS complexes). Hence this is a sinus tachycardia with AV dissociation and a ventricular tachycardia.
Since the ventricular rate and atrial rate are identical, this is termed isorhythmic dissociation. It is not clear if this is complete heart block with an escape ventricular rhythm or an accelerated idioventricular rhythm, ie, ventricular tachycardia.
The occurrence of intermittent fusion and capture means that this is an accelerated ventricular rhythm, ie, ventricular tachycardia. When there is a subtle increase in the sinus rate (or a subtle decrease in the ventricular rate), AV capture occurs.
In addition, there is pronounced ST-segment elevation in leads V3–V6 (▼). The ST segments still have a concave morphology. Given the clinical history, the ECG changes are consistent with an acute anterolateral myocardial infarction. Although the complexes in leads I through aVF are ventricular, there is also ST-segment elevation in leads I and aVL (↑), suggesting that there is also involvement of the lateral wall.
READ MORE: