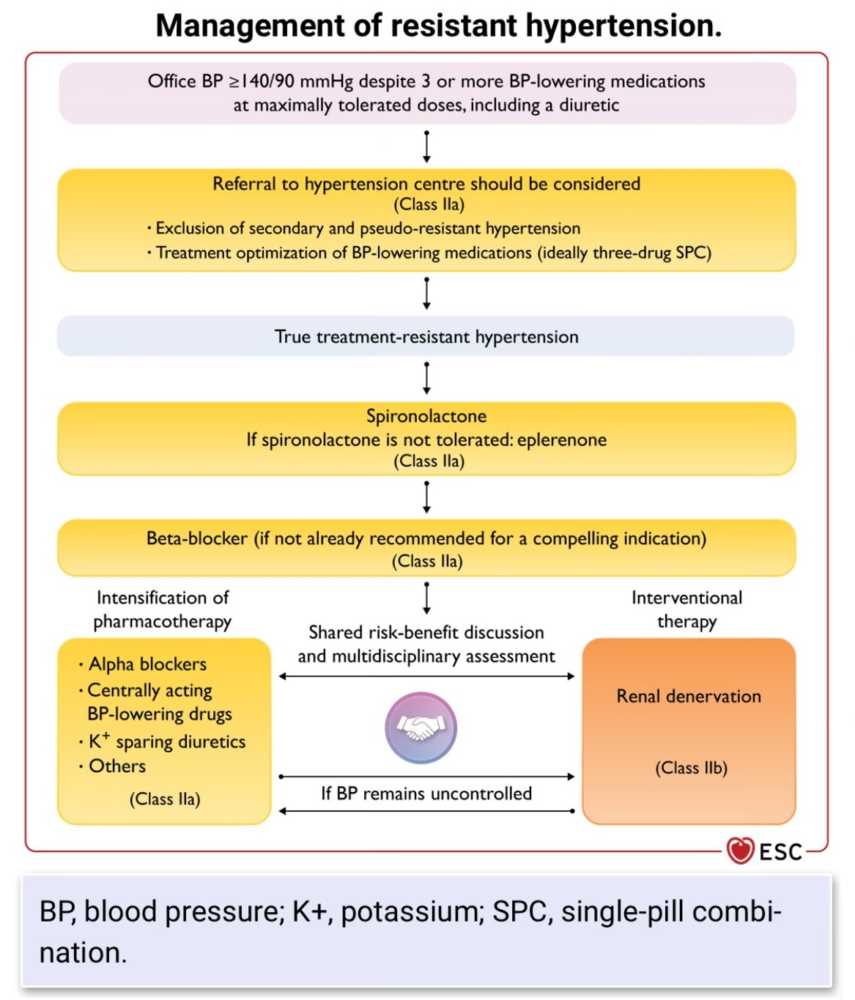
Driving Better Results in the Treatment of Resistant Hypertension
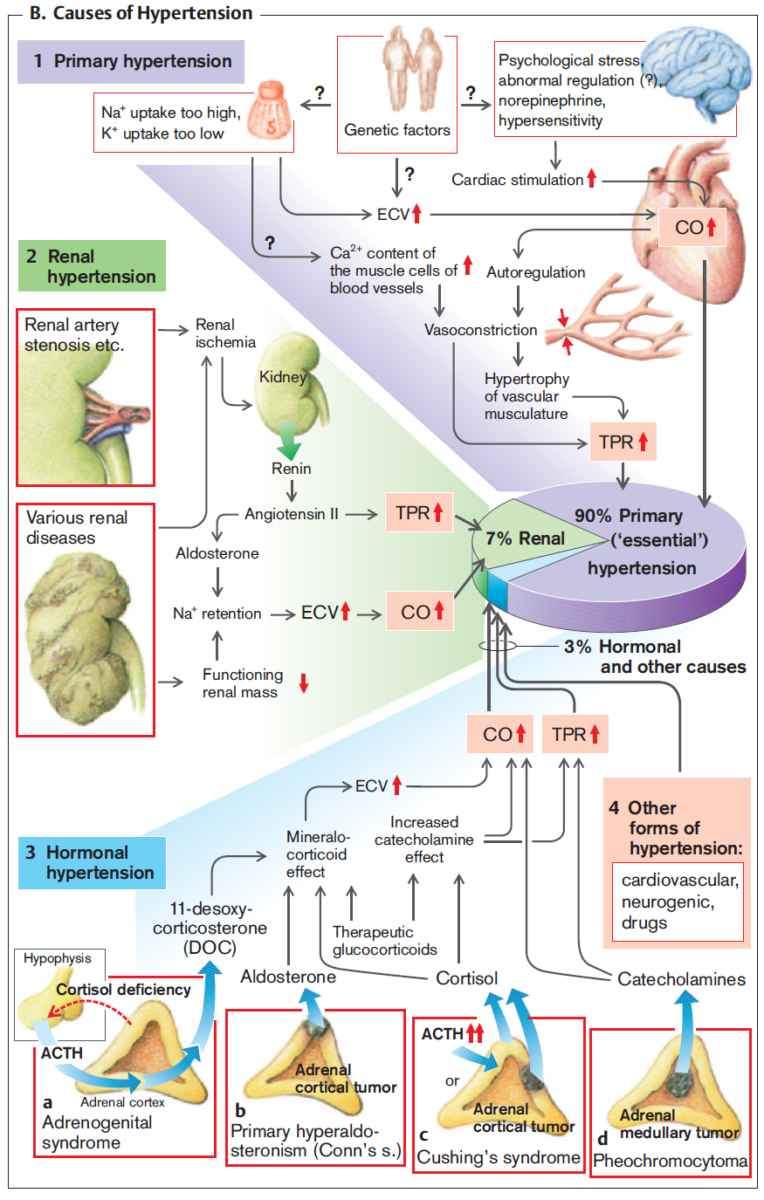
Resistant hypertension is a multifaceted condition that complicates standard hypertension management. Its complexity stems from various overlapping causes and population-level disparities...

![Read more about the article Left Ventricular Hypertrophy (LVH): How to Recognize it on ECG [With Examples]](https://manualofmedicine.com/wp-content/uploads/2025/12/Summary-of-the-various-diagnostic-ECG-criteria-for-left-ventricular-hypertrophy-LVH.png)
![Read more about the article Atrial Flutter: ECG Interpretation [With Examples]](https://manualofmedicine.com/wp-content/uploads/2022/01/Atrial-Flutter-with-4-1-AV-Block.png)