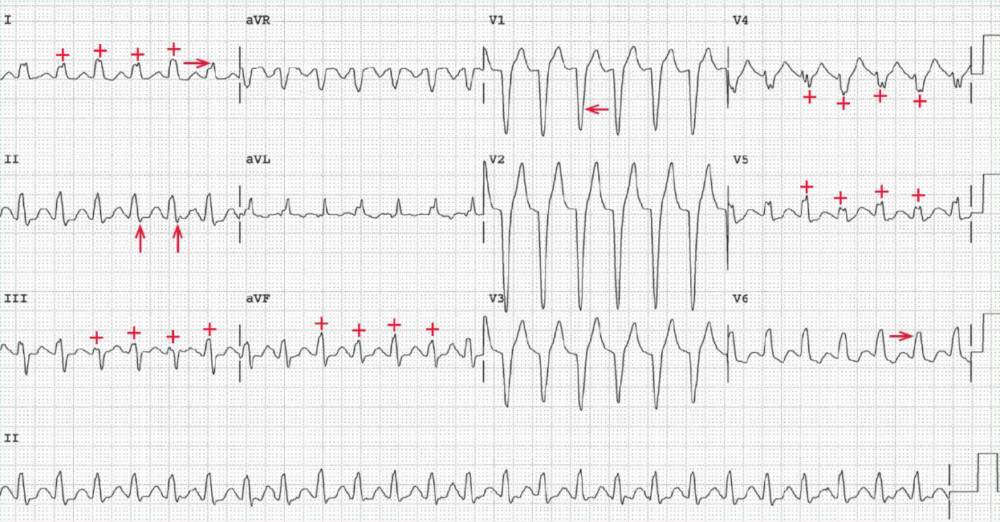
The ECG shows a regular rhythm at a rate of 154 bpm. The QRS complex duration is increased (0.14 sec). There is a broad R wave in leads I and V5-V6 (—>) and a deep QS complex in lead VI (<—), characteristic of typical left bundle branch block (LBBB).
No P waves are seen before or after any of the QRS complexes. Hence this is termed no RP tachycardia. The etiology may be either ventricular tachycardia or supraventricular (junctional) tachycardia with aberration.
READ ALSO: Never Mistake Ventricular Tachycardia for Supraventricular Tachycardia with Aberrant Conduction
The most common etiology for supraventricular or junctional tachycardia that is not associated with any obvious P waves is AV nodal reentrant tachycardia (AVNRT). In this case it is associated with an LBBB, which is either rate related or preexisting, being present during normal sinus rhythm.
The presence of a QRS complex with a typical LBBB morphology strongly suggests that the arrhythmia is supraventricular.
Although P waves are not seen, there is a small terminal S wave in lead II (↑) that is suggestive of a P wave. To establish this as a retrograde P wave, the morphology of the QRS complex during the tachycardia should be compared with the QRS complex morphology during sinus rhythm.
In addition, there is evidence of beat-to-beat changes in QRS complex amplitude (+), termed QRS (electrical) alternans, which is most prominent in leads I, III, aVF, V4, and V5.
Although most often considered a hallmark of cardiac tamponade, QRS alternans may be seen in any rapid supraventricular tachycardia. It is not generally seen with ventricular tachycardia.
Other causes of electrical or QRS alternans, also the result of alterations in calcium fluxes, include acute myocardial infarction, decompensated heart failure, and severe cardiomyopathy.

![Read more about the article Atrial Flutter: ECG Interpretation [With Examples]](https://manualofmedicine.com/wp-content/uploads/2022/01/Atrial-Flutter-with-4-1-AV-Block-300x135.png)