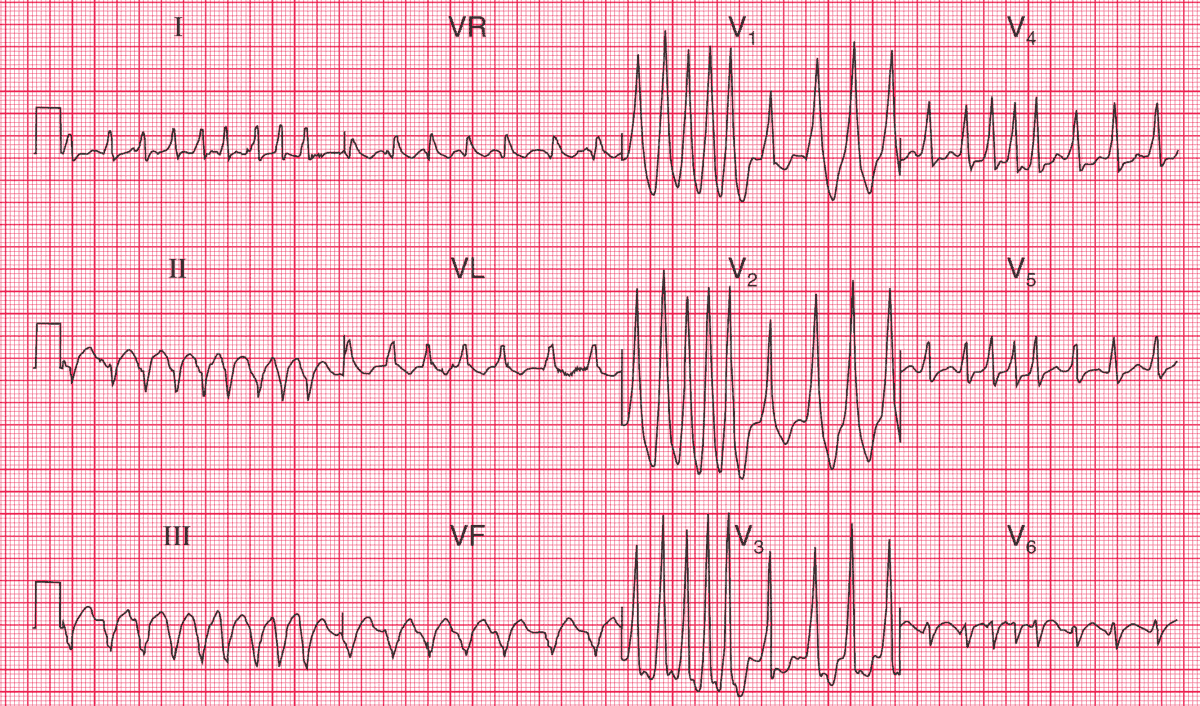
ECG Intepretation
- Irregularly irregular tachycardia
- No consistent P waves visible
- Left axis deviation
- QRS complex duration varies between about 120 and 160 ms
- QRS complexes show a dominant R wave in lead V1 and a prominent S wave in lead V6
- After the longer pauses, the upstroke of the QRS complexes appears slurred
Clinical Interpretation
The marked irregularity of this rhythm must be explained by atrial fibrillation with rapid ventricular response.
The broad QRS complexes might be due to right bundle branch block, but the dominant R wave in lead V1, together with the slurred upstroke of the QRS complex in at least some leads, indicate the Wolff–Parkinson–White (WPW).
What to do ?
A combination of the WPW syndrome and atrial fibrillation is very dangerous, because it can degenerate into ventricular fibrillation. The arrhythmia needs treating as an emergency, whatever the clinical state of the patient.
It is important not to use drugs that may block the atrioventricular node and increase conduction through the accessory pathway, because this will increase the risk of ventricular fibrillation. Therefore, adenosine, digoxin, verapamil and lidocaine are contraindicated.
The drugs that slow conduction in the accessory pathway, and are therefore safe, are the beta-blockers, flecainide and amiodarone. Thereafter, an electrophysiological study to identify and ablate the accessory pathway is essential.
- READ MORE:
- Similar Cases:
- ECG Case 80: Atrial Fibrillation and WPW Syndrome
- ECG Case 71: Atrial fibrillation with RVR, LAFB and Acute Anterolateral STEMI
- ECG Case 66: Atrial Fibrillation with an Uncontrolled Ventricular Rate
- ECG Case 59: Atrial Fibrillation with Rapid Ventricular Response (RVR) and Diffuse Subendocardial Ischemia