The rhythm is irregularly irregular at a rate of 54 bpm. There are no obvious organized P waves; rather, there are fine and rapid waveforms (+) that are irregular in amplitude, morphology, and interval. These are atrial fibrillatory waves and the underlying rhythm is atrial fibrillation with a slow ventricular response.
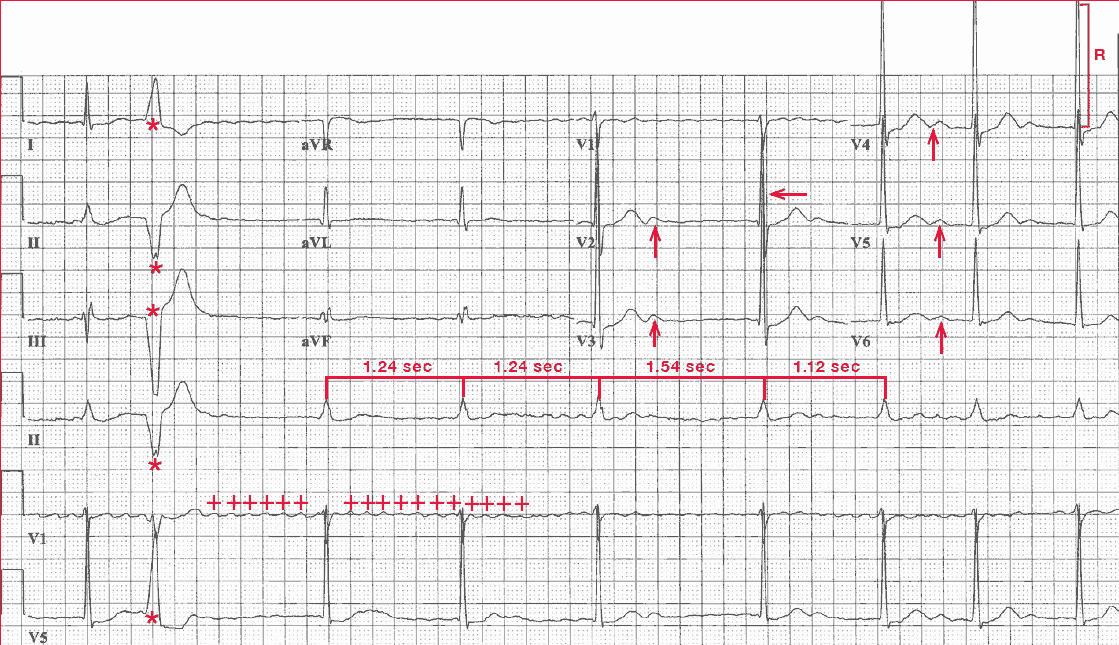
A single premature ventricular complex can be seen (second QRS complex [*]). The QRS complex axis, duration (0.10 sec), and morphology are normal. However, there is early transition (ie, a tall R wave in lead V2 [←]) as a result of counterclockwise rotation in the horizontal plane.
The amplitude of the QRS complex is tall (R-wave amplitude in leads V3-V4 = 33 mm [ ] ]), which is diagnostic for left ventricular hypertrophy (ie, S-wave or R-wave in any precordial lead ≥25 mm). The QT/QTc intervals are normal (460/440 msec).
In addition, prominent U waves are seen in leads V2-V6 (↑). It is often seen as a low-amplitude, positive waveform in the right precordial leads (V1-V3) and it often becomes more prominent with bradycardia.
However, an increase in the amplitude of the U wave or its presence in the lateral precordial leads (V4-V6) is suggestive of hypokalemia, which is likely the result of the addition of hydrochlorothiazide. This is a thiazide diuretic, and one of the most common side effects of this class of drugs is hypokalemia.
The presence of hypokalemia may result in an increase in digoxin effect and possible digoxin toxicity, even with stable and therapeutic digoxin levels. It is likely that her symptoms of fatigue and muscle aches are the result of hypokalemia
The slow ventricular response rate noted in this patient is the result of combined therapy with two AV nodal blocking agents. Digoxin slows AV nodal conduction as a result of increased vagal tone. Calcium channel blockers have a direct effect on AV nodal conduction properties because the AV nodal electrophysiologic properties are mediated by a slow calcium current.
It has been observed that in patients with a history of paroxysmal or intermittent atrial fibrillation, the use of digoxin is associated with increased episodes of atrial fibrillation and may even precipitate sustained atrial fibrillation. Therefore, digoxin is not appropriate therapy for prevention of paroxysmal atrial fibrillation.