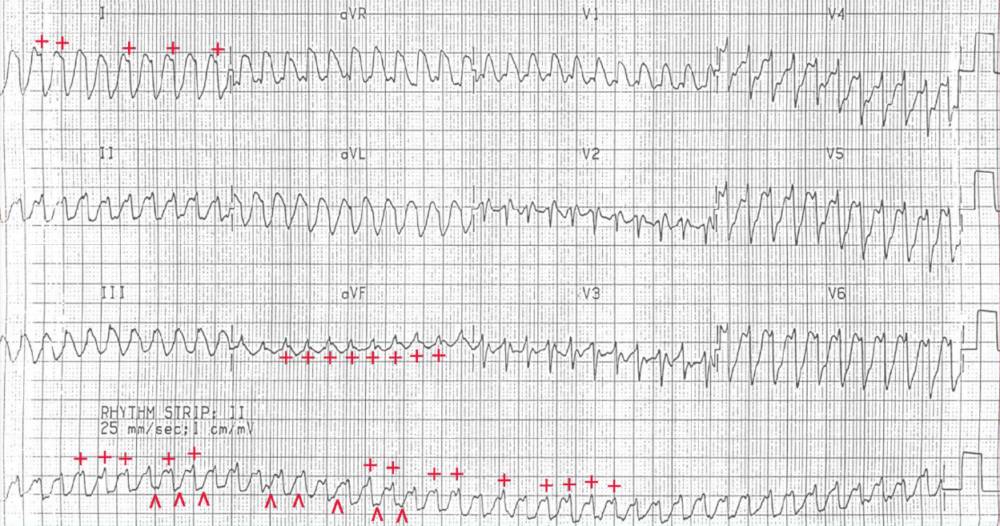
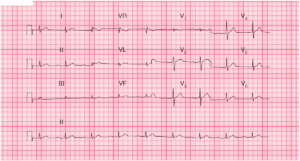
There is a regular rhythm at a rate of 270 bpm. The QRS complex duration is 0.16 second; the QRS morphology is abnormal and the axis is rightward, between +90° and +180° (negative QRS complex in lead I and positive QRS complex in lead aVF).
There are only two arrhythmias that present with a regular rate over 260 bpm (ie, atrial flutter with 1:1 conduction or ventricular tachycardia, which at this rate is often termed ventricular flutter). There is no obvious atrial activity.
There is subtle variability in the morphology of the QRS complex (+) and ST-T waves (^), most apparent in the lead II rhythm strip as well as leads I and aVF (+). These are features seen with sustained ventricular tachycardia. The morphology of the QRS complexes is similar; hence this is monomorphic ventricular tachycardia.
Immediate defibrillation is indicated when the arrhythmia is associated with hemodynamic compromise, as in this patient who became pulseless.
Importantly, cardioversion (which is the delivery of a low- energy shock synchronous with the QRS complex) should not be used as at this rate it is not possible to distinguish between the QRS complex and the T wave, and the shock could be delivered on top of the T wave.
In addition, CPR and advanced cardiovascular life support should be performed, including airway maintenance and oxygenation (ie, intubation), chest compressions, and administration of epinephrine (+/- vasopressin) and anti-arrhythmic therapy at the appropriate time intervals.