Radiologic Findings
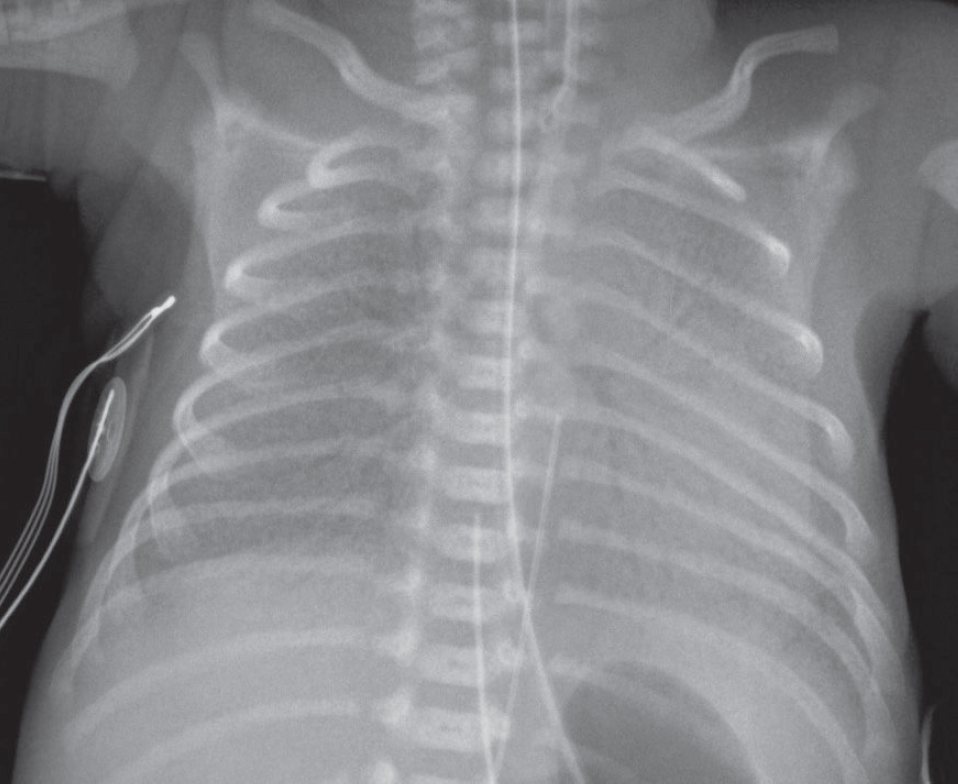
AP chest radiograph shows:
- Bilateral, symmetrical, perihilar opacities with a fine granular pattern and associated air bronchograms.
- The lung volumes are diminished bilaterally.
- Note the endotracheal tube, enteric tube, umbilical arterial and umbilical venous catheters.
Diagnosis
Adhesive Atelectasis: Respiratory Distress Syndrome (RDS) of the Newborn
Differential Diagnosis
- Pneumonia
- Volume overload or heart failure
- Massive aspiration
- Pulmonary hemorrhage
Adhesive Atelectasis: Respiratory Distress Syndrome (RDS) of the Newborn
Background
The pressure-volume relationships of the lung depend on forces acting at the air-tissue interface of the alveolar wall. These forces are further understood by applying Laplace’s law (p = 2T/r), where p represents pressure, T the surface tension at the air-tissue interface, and r the radius of a sphere, which in this case represents the alveoli.
As alveoli diminish in volume, the surface tension of the interface is diminished by surfactant (phos-pholipid dipalmitoyl phosphatidylcholine). The production of abnormal or insufficient surfactant results in increased surface tension within the alveoli and widespread alveolar collapse (e.g., microatelectasis) despite patent airways.
Once collapsed, alveolar walls tend to adhere (hence the term adhesive atelectasis), making re-expansion difficult. Adhesive atelectasis may produce significant arteriovenous shunting in spite of a relatively normal chest radiograph.
Clinical Findings
The best examples of adhesive atelectasis are RDS of the newborn and acute radiation pneumonitis. Adhesive atelectasis may also occur with acute respiratory distress syndrome (ARDS) of adults, smoke inhalation, bronchopneumonia, uremia, prolonged shallow breathing associated with surgery, cardiac bypass surgery, pulmonary contusions and other causes of pulmonary hemorrhage, and acute pulmonary thromboembolic disease.
Adhesive atelectasis tends to be more widespread with both newborn and adult forms of ARDS and smoke inhalation, whereas it is limited to the radiation port or its outer margins with acute radiation pneumonitis.
In pulmonary embolism, focal ischemia distal to the embolus can result in a marked reduction in surfactant levels, leading to subsegmental or even segmental atelectasis.
Imaging Findings
- Chest radiography may be relatively normal
- Ground-glass opacities and/or consolidation with associated volume loss
- Subsegmental or even segmental atelectasis
- Patent bronchi and bronchioles may manifest as air bronchograms (i.e., nonobstructive atelectasis)
Management
- Directed toward underlying cause
- Supportive; supplemental oxygen and mechanical ventilation (positive end-expiratory pressure) as needed
- Surfactant (Curosurf [Poractant Alpha] [Chiesi Farmaceutici, Parma, Italy]) administration
Prognosis
- Variable
- Curosurf improves oxygenation and lung compliance and reduces mortality and pneumothoraces associated with RDS
Pearls
Prototypical examples of adhesive atelectasis include respiratory distress syndrome of the newborn and acute radiation pneumonitis.
Suggested Readings
- Fraser RS, Müller NL, Colman N, Paré PD. Atelectasis. In: Fraser and Paré’s Diagnosis of Diseases of the Chest, 4th ed. Philadelphia: Saunders; 1999:522
- Plavka R, Kopecký P, Sebron V, et al. Early versus delayed surfactant administration in extremely premature neonates with respiratory distress syndrome ventilated by high-frequency oscillatory ventilation. Intensive Care Med 2002;28(10):1483–1490
- Schindler MB. Treatment of atelectasis: where is the evidence? Crit Care 2005;9(4):341–342
- Wilcox P, Baile EM, Hards J, et al. Phrenic nerve function and its relationship to atelectasis after coronary artery bypass surgery. Chest 1988;93(4):693–698
- Woodring JH, Reed JC. Types and mechanisms of pulmonary atelectasis. J Thorac Imaging 1996;11(2):92–108