This article is an answer to the Case – 38-year-old Female with Painful Patches and Plaques
Warfarin-induced skin necrosis is a rare complication that usually occurs within three to five days of starting therapy. Obese and postmenopausal women are most commonly affected. Fatty areas such as the breasts, thighs, buttocks and abdomen are the most likely areas to be involved.
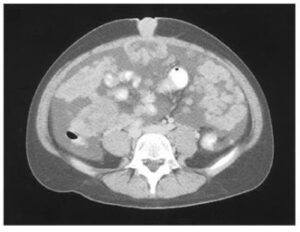
Initially the lesions are red, painful patches and plaques that subsequently develop into hemorrhagic bullae and then ultimately into necrotic eschars.
Pathoetiology of Warfarin-Induced Skin Necrosis
The pathoetiology is believed to be due the decrease in the anticoagulant functional protein C, which occurs more quickly than the decrease in functional procoagulant enzymes upon initiation of warfarin.
Although the overall effect of warfarin is supposed to be anticoagulant, if the protein C level drops more quickly than the procoagulant enzymes, then the initial net effect of the warfarin will actually be procoagulant. This leads to thrombosis and skin necrosis.
Notably, up to one-third of patients with warfarin-induced skin necrosis may have an inherited partial deficiency in protein C. On histology, thrombosis within blood vessels is seen without significant inflammation.
Treatment
Treating warfarin-induced skin necrosis consists of immediately ceasing warfarin and administering vitamin K and heparin. Infusion of purified protein C is also helpful.
Heparin is another agent that may cause anticoagulant-induced skin necrosis. Heparin-induced skin necrosis begins six to 12 days after treatment is initiated and may occur either locally at the site of injection or in a more widespread pattern.
Unfractionated heparin is more likely to cause necrosis than low molecular weight heparin. Most necrotic skin reactions caused by heparin are associated with the heparin-induced thrombocytopenia (HIT).
Heparin-dependent antibody directed against platelets causes HIT. The antibody causes platelet aggregation within blood vessels leading to thrombosis. This may lead to infarction of multiple organ systems including skin, heart, brain and lungs.
HIT treatment involves ceasing treatment with heparin and administering a direct thrombin inhibitor. Immediate treatment of HIT with warfarin is contraindicated, because it can actually worsen the prothrombotic state.