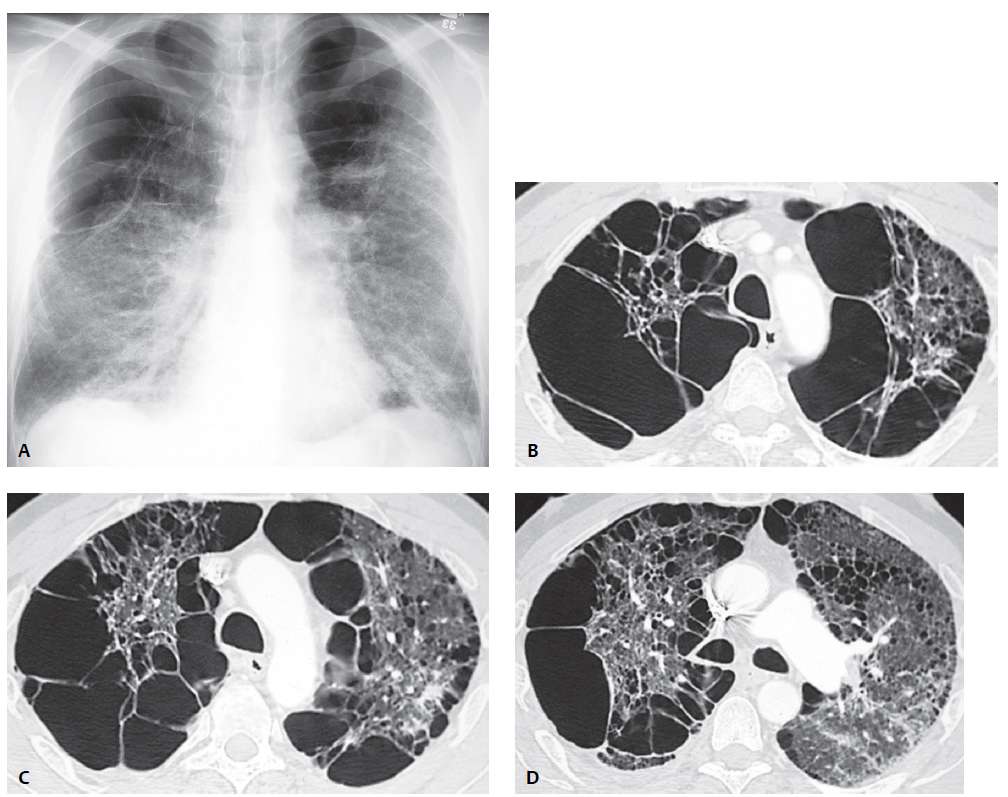
PA chest radiograph (A) demonstrates hyperinflation with bilateral upper lobe hyperlucency secondary to bilateral large apical bullae that compress adjacent lung. Bands of atelectasis are demonstrated at both lung bases.
High-resolution CT (lung window) (B, C, D) demonstrates bilateral large bullae that preferentially affect the right lung and produce mediastinal shift to the left. Scattered areas of proximal acinar emphysema and a single subpleural arcade of distal acinar emphysema are demonstrated in the left upper lobe (D).
Etiology
The pathogenesis of distal acinar emphysema is uncertain but is probably related to a relative paucity of vascular and elastic fibers in subpleural pulmonary lobules.
Clinical Findings
Bullous lung disease is most commonly detected in patients who have concomitant emphysema but also occurs in patients with connective-tissue diseases, such as Marfan syndrome and Ehlers-Danlos syndrome. Affected patients may be asymptomatic but commonly complain of dyspnea on exertion.
Distal acinar emphysema rarely causes functional abnormalities. Rupture of subleural bullae may result in primary spontaneous pneumothorax in tall, asthenic individuals.
Imaging Features
Chest Radiography
- Thin-walled, well-defined avascular areas in lung parenchyma (bullae)
- Mass effect on adjacent lung
- Air-fluid levels within secondarily infected bullae
- Associated pneumothorax
MDCT /HRCT
- Many of the same features seen on chest radiography
- Focal subpleural cystic areas near interlobular septa, large vessels, and bronchi
- Frequent associated proximal acinar emphysema
- Large bullae, usually between 2–8 cm in diameter (giant bullous emphysema)
Management
- Smoking cessation and preoperative pulmonary rehabilitation
- Surgical resection of affected lobe for patients with incapacitating dyspnea and large bullae that fill more than 30% of the affected hemithorax, and for patients with recurrent infection/pneumothorax
Prognosis
- Good
Pearls
- Bullae typically increase progressively in size, but may also become infected and subsequently disappear
- Patient selection remains one of the most important aspects of successful surgery for bullous lung disease. Compressed, atelectatic lung may re-expand following resection of bullae.
- Distal acinar emphysema may be an isolated finding or may be associated with chronic bronchitis and chronic airflow obstruction.
Imaging Features Chest R adiography •â•¢ Thin-walled, well-defined avascular areas in lung parenchyma (bullae) (Fig. 30.1A) •â•¢ Mass effect on adjacent lung (Fig. 30.1A) •â•¢ Air-fluid levels within secondarily infected bullae •â•¢ Associated pneumothorax MDCT /HRCT •â•¢ Many of the same features seen on chest radiography •â•¢ Focal subpleural cystic areas near interlobular septa, large vessels, and bronchi (Figs. 30.1B, 30.1C, 30.1D, 30.3, 30.4, 30.5) •â•¢ Frequent associated proximal acinar emphysema (Figs. 30.1D, 30.4) •â•¢ Large bullae, usually between 2–8 cm in diameter (giant bullous emphysema) (Figs. 30.4, 30.5) Management •â•¢ Smoking cessation and preoperative pulmonary rehabilitation •â•¢ Surgical resection of affected lobe for patients with incapacitating dyspnea and large bullae that fill more than 30% of the affected hemithorax, and for patients with recurrent infection/pneumothorax Prognosis •â•¢ Good