Table of Contents
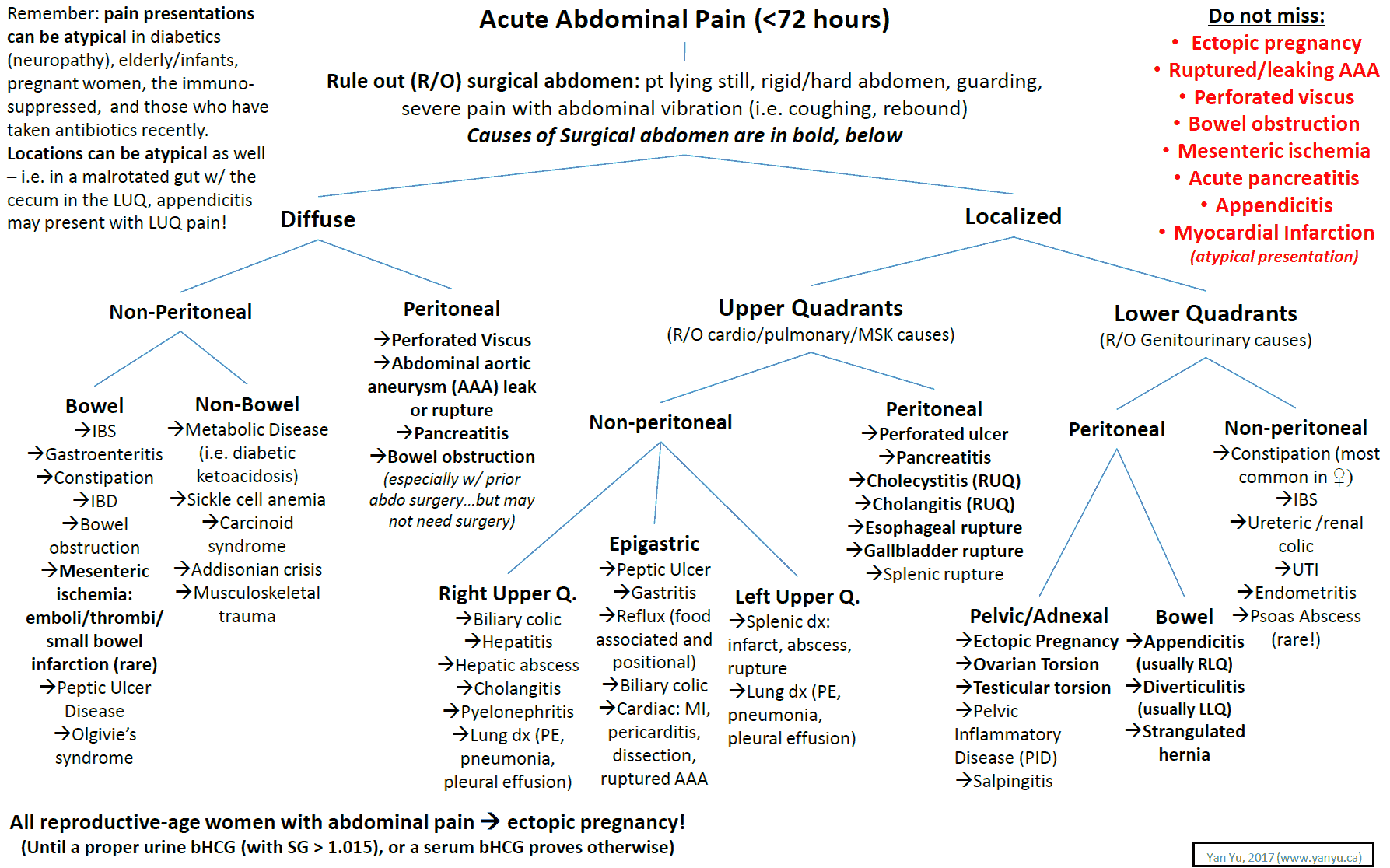
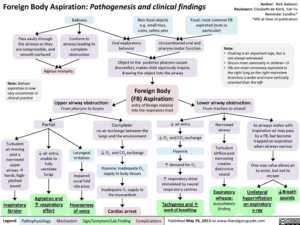
Resuscitation and Critical Diagnosis
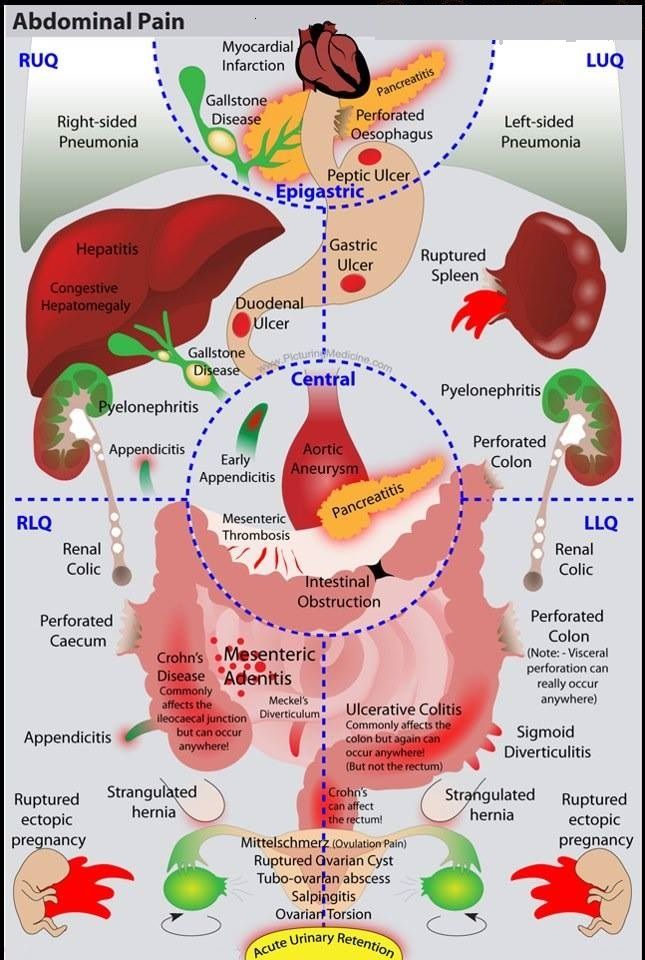
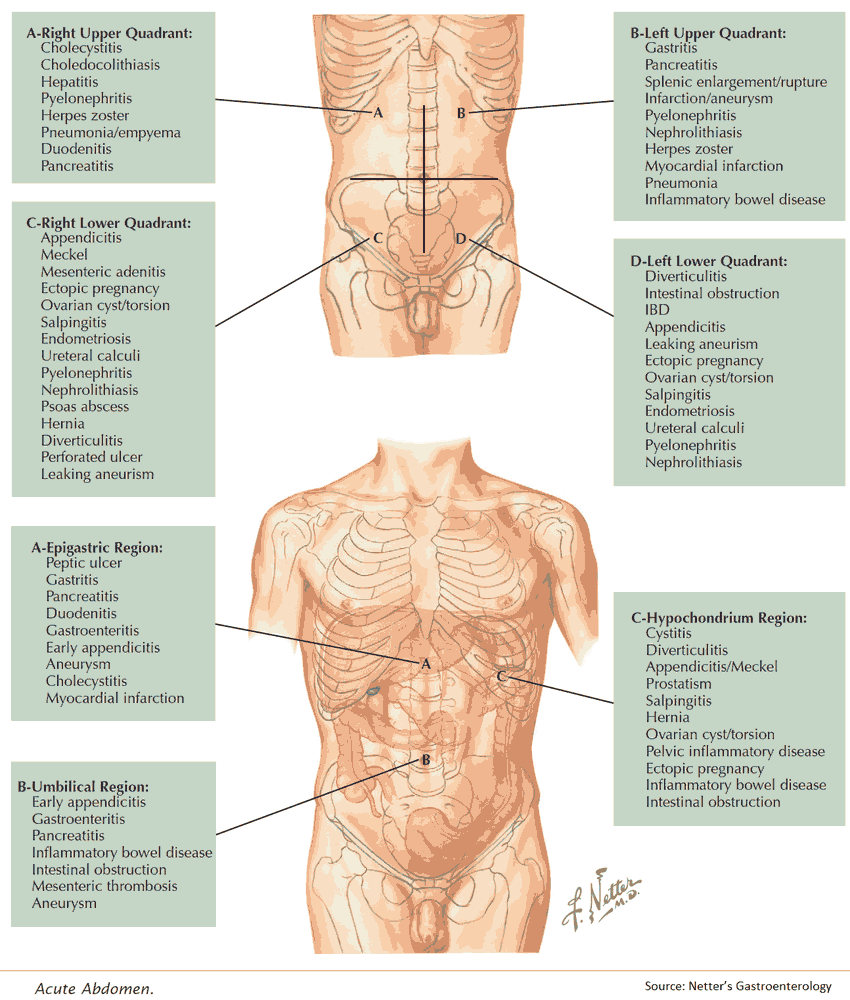
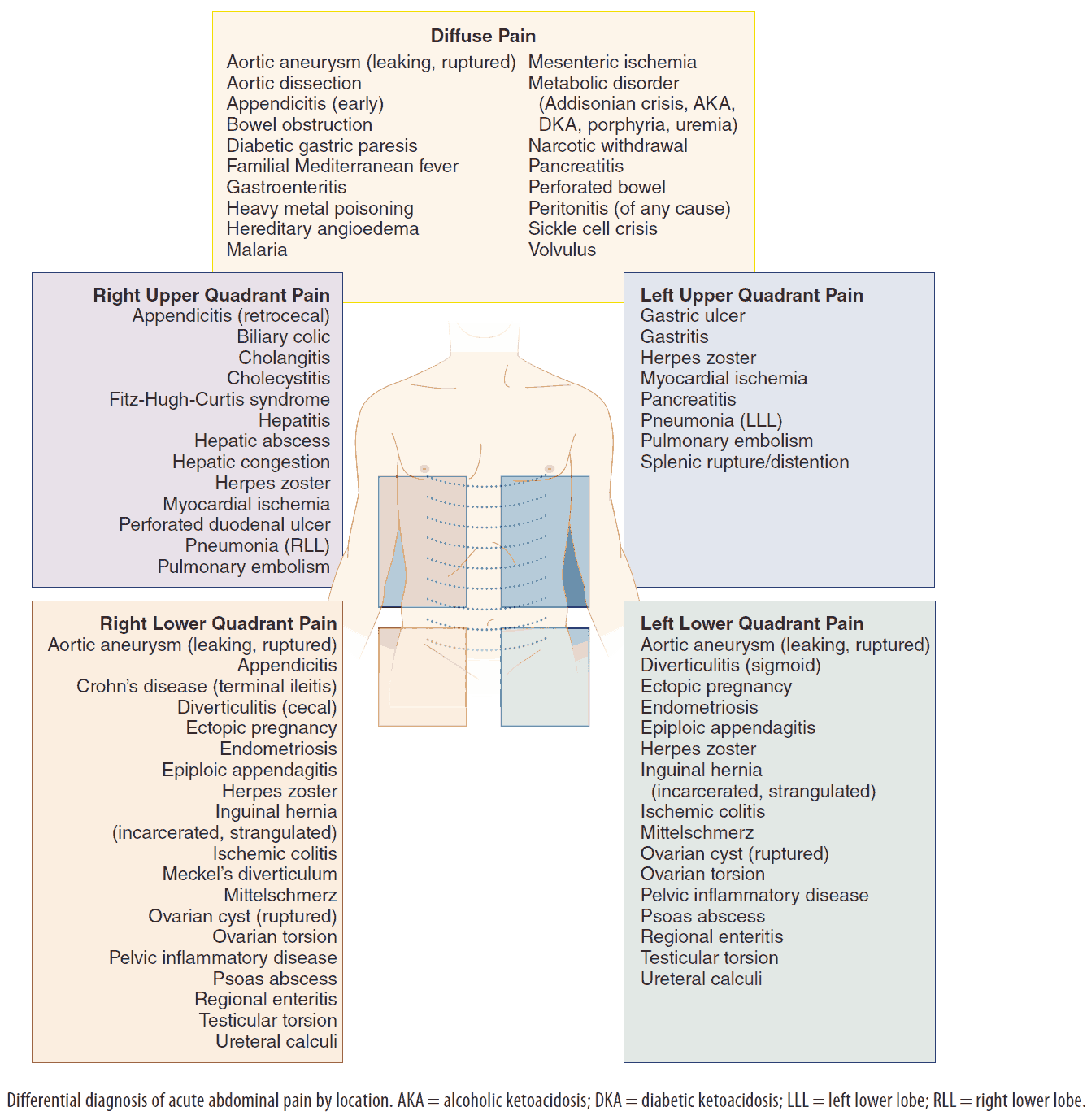
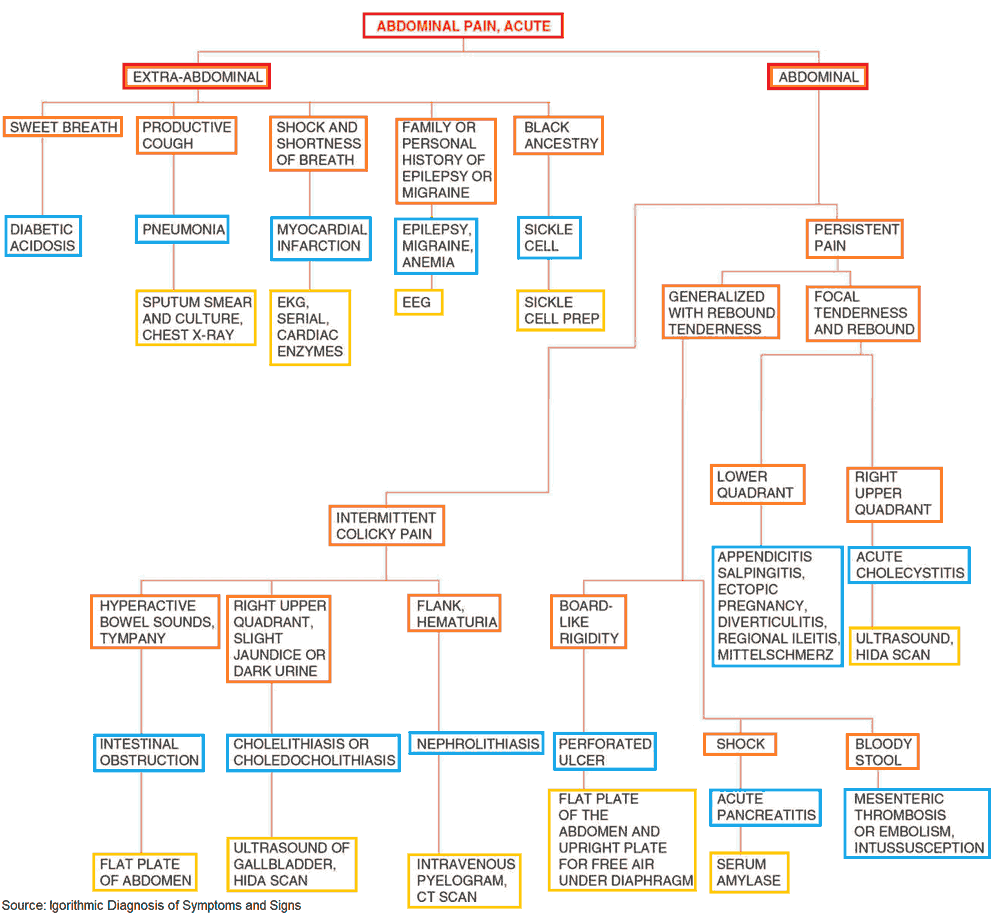
- Work-up for abdominal pain begins with resuscitation and exclusion of critical diagnoses:
- AAA (Abdominal Aortic Aneurysm)
- Mesenteric Ischemia
- Perforation
- SBO (small bowel obstruction)
- Ectopic pregnancy
- Then, through a detailed history and physical, consider all the causes of abdominal pain
- Rule out Genitourinary causes (pyelonephritis vs kidney stone) if possible with Urine Analysis
- The differential for upper abdominal pain may come down to Gallstone etiology vs Gastritis/PUD that will need further imaging based on suspicion (ultrasound of abdomen)
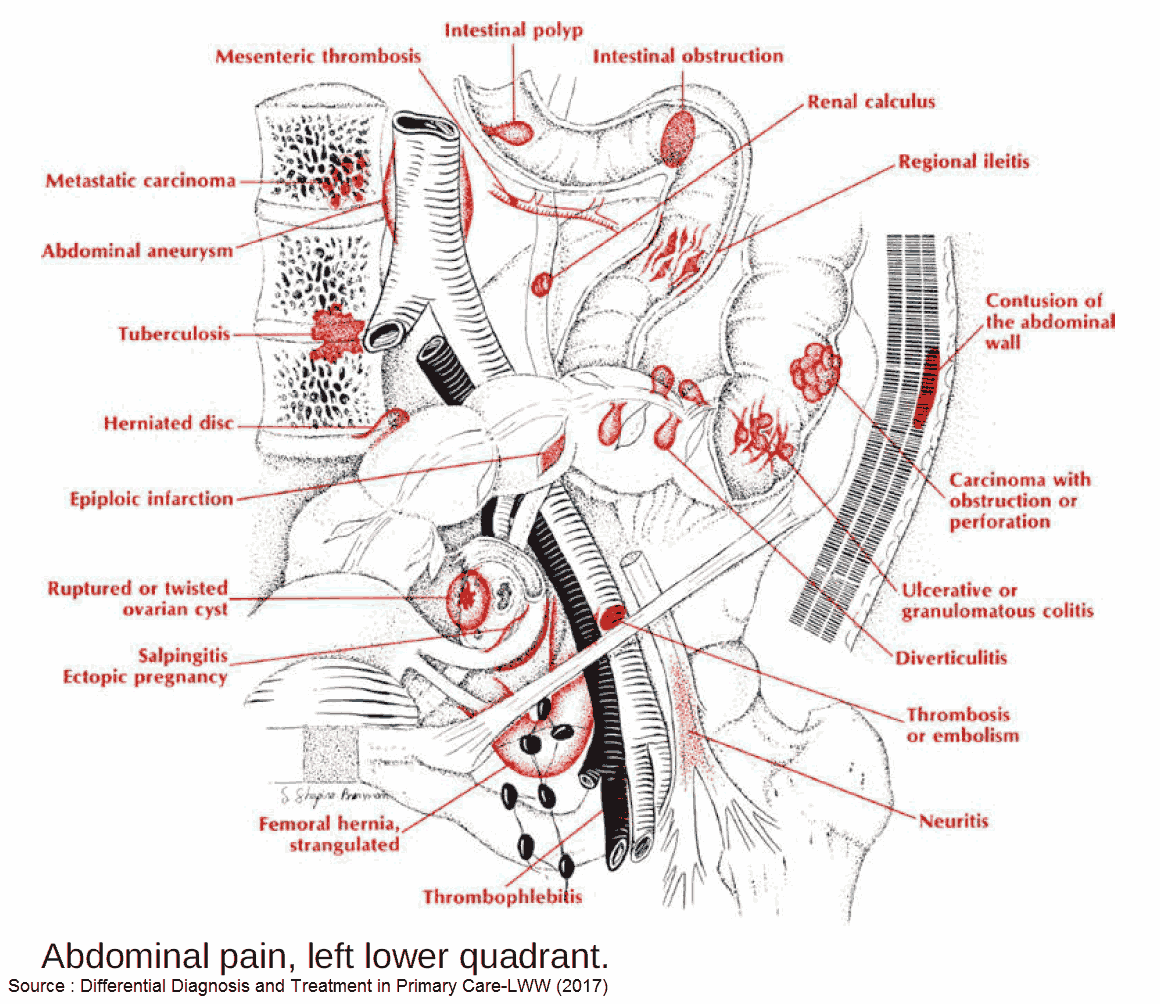
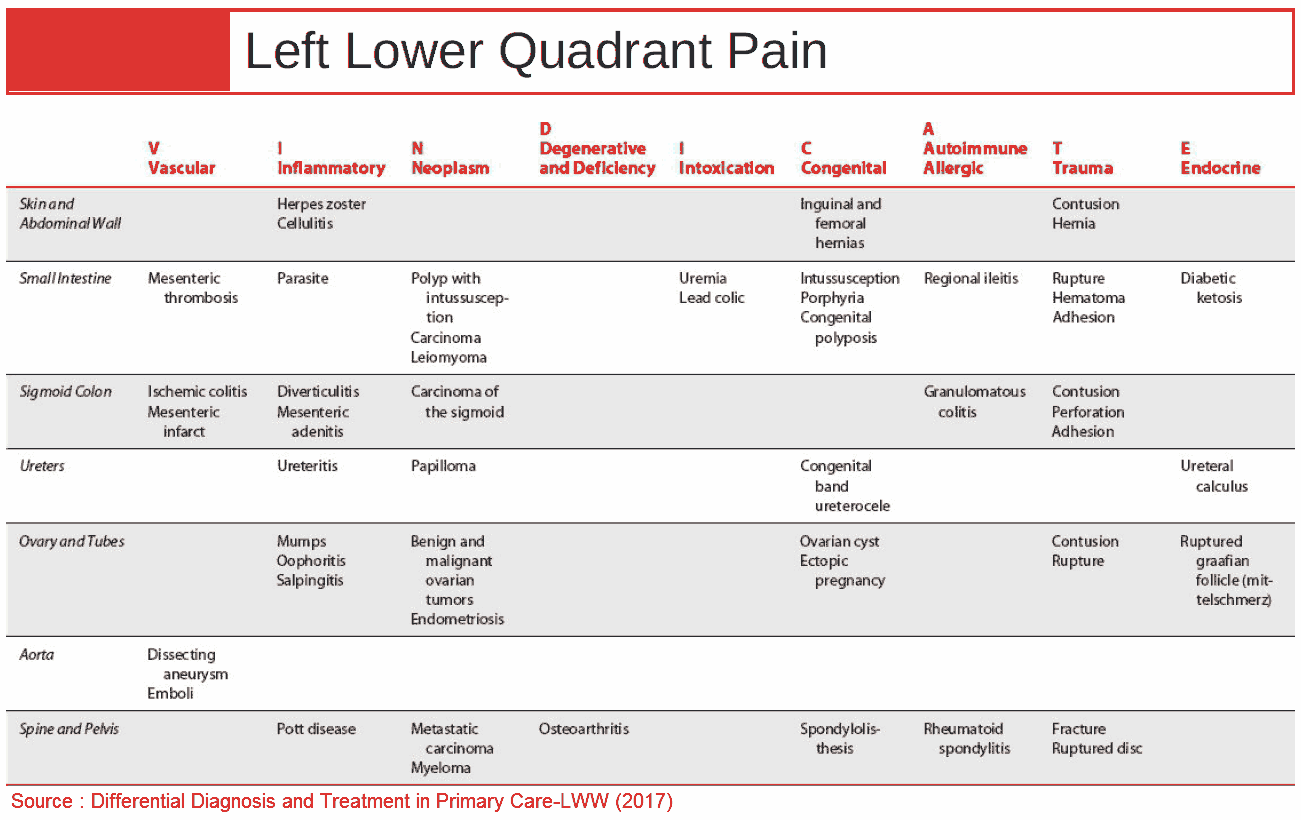
- The differential for lower abdominal pain may come down to GI (appendicitis, diverticulitis) vs pelvic etiology (in females) and will need further imaging based on suspicion (CT A/P vs pelvic ultrasound)
Resuscitate
- IV/O2/Monitor, IV Fluids, Labs as needed, pregnancy test
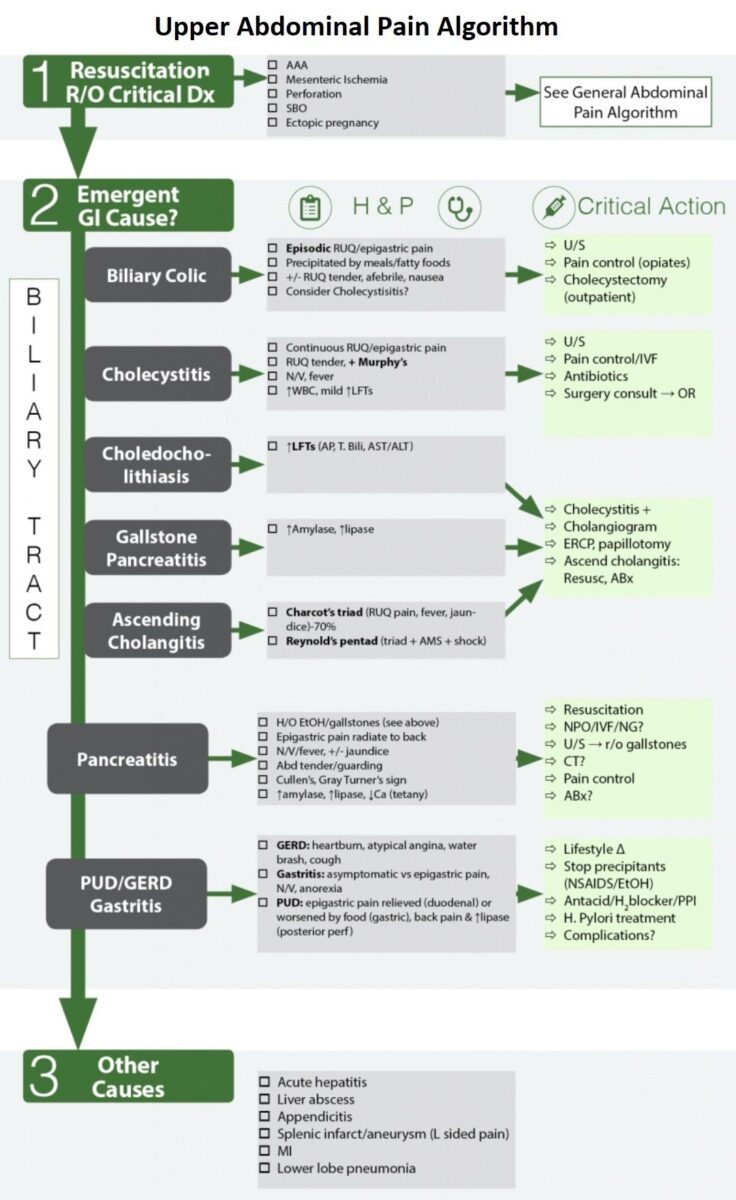
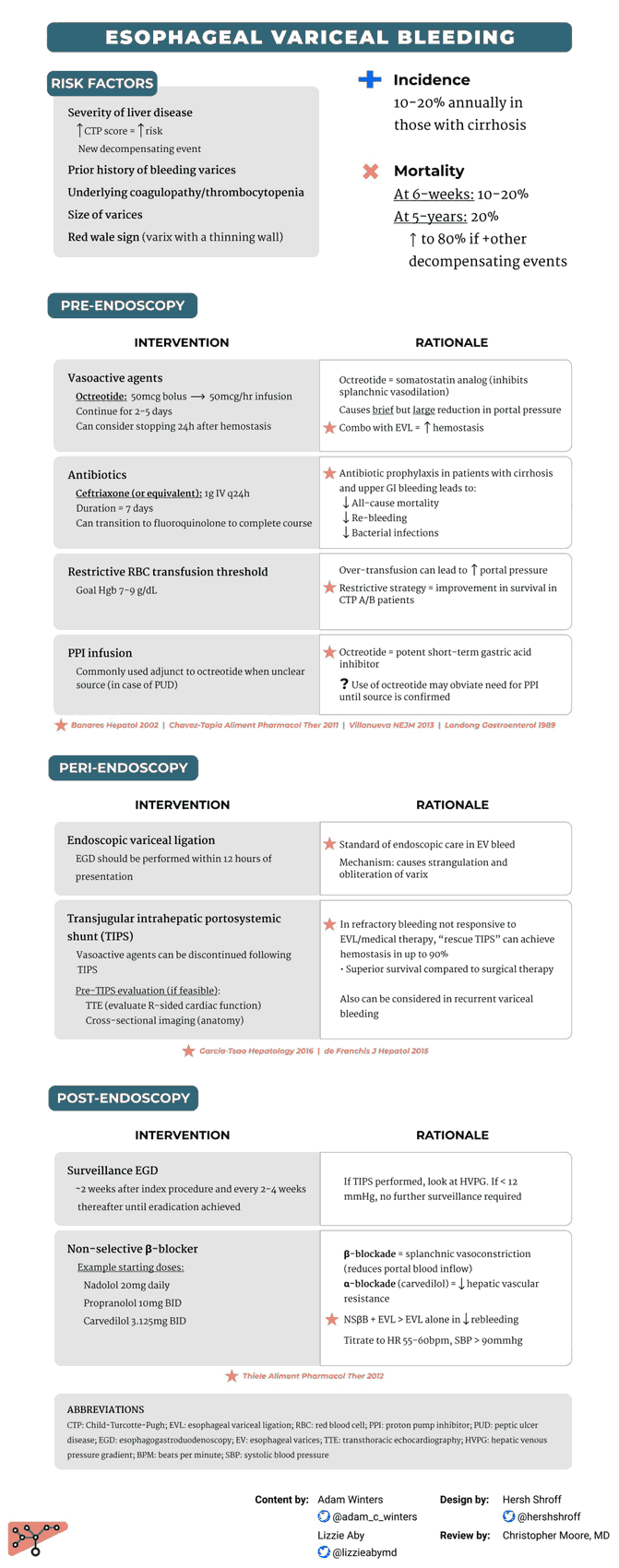
Emergent Gastrointestinal ( GI ) Causes of Upper Abdominal Pain
- Billiary Tract Disease
- Biliary Colic
- Cholecystitis
- Choledocholithiasis
- Gallstone pancreatitis
- Ascending cholangitis
- Acute Pancreatitis
- Gastritis , GERD , Peptic Ulcer Disease
1. Billiary Tract Disease
The goal is to find the location of the stone and its associated complications. Is it still in the gallbladder (symptomatic cholelithiasis), in the cystic duct (cholecystitis), or in the CBD (choledocholithiasis, gallstone pancreatitis, ascending cholangitis)
Cholelithiasis
- Prevalence of 10% in US, usually asymptomatic (symptoms develop in 2%/yr)
Biliary Colic
- Symptomatic cholelithiasis caused by obstruction of cystic duct by gallstones
- Clinical: Episodic pain in Right Upper Quadrant (RUQ), minutes to hours, resolves spontaneously
- Precipitated by meals/fatty foods
- Treatment: Recurrent biliary colic → pain control, elective outpatient cholecystectomy
Cholecystitis
- Clinical (vs biliary colic, may be difficult to distinguish)
- Pain longer in duration (>6 hours), localizes to RUQ, ↑ N/V/F (more nausea, vomitus)
- Murphy’s sign:
- Localized peritonitis over gallbladder, arrest of inspiration on gallbladder palpation with pain
- Highest LR+ of PE/lab values
- Diminished in elderly
- Course
- 1/3 will worsen→ complications (cholangitis, perforation)
- 1/2 will improve spontaneously (7-10days)
- Laboratory: increased WBC, mild increase of LFTs
- Radiology
- Right upper quadrant ultrasound (sensitivity 84-97%, specificity up to 100%)
- Findings: Gallstones, pericholecystic fluid, gallbladder wall thickening (>3mm), sonographic Murphy’s
- HIDA scan: non-visualization of contrast in gallbladder (cholecystitis) or intestine (choledocholithiasis)
- Treatmentof Cholecystitis
- NPO / IV Fluids / Broad spectrum antibiotics
- Semi-urgent Cholecystectomy, laparoscopic (at 24-48h) with CBD exploration or ERCP if CBD stone of concern
- Complications of Cholecystitis: gallbladder perforation, emphysematous cholecystitis, gangrenous cholecystitis, cholangitis, gallstone ileus
Choledocholithiasis
- Define: Gallstone lodged in common bile duct
- Clinical: similar presentation to cholecystitis except elevated LFTs (Alkaline Phosphatase (ALP), Total Bilirubin)
- Radiology: Right upper quadrant ultrasound
- Dilated CBD (>6mm)
- Common bile duct stone
- ERCP
- Diagnose and treat common duct stones (with sphincterectomy)
- Rule out other causes of obstruction (tumors…)
Gallstone Pancreatitis
- Elevated amylase and lipase
- ERCP to decompress biliary tree
Ascending Cholangitis
- Common Bile Duct obstruction causing infection proximal to obstruction, potentially causing sepsis (increased mortality)
- Charcot’s triad (RUQ pain, fever, jaundice)
- Reynold’s pentad (Charcot + hypotension + AMS)
- Treatment
- Conservative (NPO, IV Fluids, broad-spectrum Antibiotics, elective ERCP at resolution)
- If failure of conservative therapy (15%), emergent surgery is indicated (Percutaneous vs ERCP)
Read More: Ascending Cholangitis aka Biliary Sepsis
2. Acute Pancreatitis
Etiology of Acute Pancreatitis:
- Gallstones (35%), Alcohol (30%)
- Idiopathic (10%), ERCP complications (4%), Tumors, Drugs (furosemide, sulfa, thiazides, valproate, tetracyclines…), infection (viral, mycoplasma), blunt trauma (1.5%), scorpion, hypercalcemia, elevated triglycerides ( hypertriglyceridemia )
Symptoms and Signs of Acute Pancreatitis
- Epigastric pain radiating to back
- Nausea / Vomitus / fever, jaundice
- Abdominal tenderness / guarding, Cullen’s (peri-umbilical ecchymosis), Gray Turner’s (flank bruising)
Diagnosis of Acute Pancreatitis:
- Lipase
- Levels peak (12-36h), duration (2 weeks)Test of choice, better sensitivity and specificity over amylase, lipase level 3x normal, more specific
- If high suspicion for pancreatitis and lipase negative, do CT scan
- Level of lipase not predictive of severity of pancreatitis
- Amylase
- Less specific, duration (1 week)
- Not used: many false positives and false negatives
- Many sources: bowel, uterus, pancreas
- Amylase: level 3x normal, not specific
- CT A/P
- Unsure of diagnosis (high index of suspicion and lipase low)
- Will see acute and chronic changes on CT
- Rule out surgical issues
- Staging system (Balthazar) → help stage and predict which patients will develop severe complication: necrotizing pancreatitis
- Unsure of diagnosis (high index of suspicion and lipase low)
- RUQ Ultrasound to diagnose gallstone pancreatitis
Treatment of Acute Pancreatitis
- Resuscitation
- NPO / bowel rest / IV Fluids / Nasogastric suction
- Fluid resuscitation (up to 10L/day, maintain adequate urinary output)
- Antibiotics
- Meta-analysis showed prophylactic antibiotics for necrotizing pancreatitis decreased sepsis and mortality
- Imipenem/meropenem, for sickest patients
- Necrotizing Pancreatitis
- Antibiotics (Imipenem), CT A/P, Urgent surgical consultation, ICU
- Fluid collections, CT or U/S guided drainage
- Infected pancreatic collections benefit from early surgery
- Gallstone Pancreatitis
- RUQ Ultrasound to diagnose
- MRCP if not sure of obstructive etiology
- Treatment: ERCP (but may cause pancreatitis)
Complications of Acute Pancreatitis
- NECROTIZING PANCREATITIS
- Pancreatitis → necrosis/liquefaction of tissue → local/systemic complications
- Greatest life-threatening complication of pancreatitis (mortality up to 50%)
- Predisposes to sepsis, multi-organ failure and death
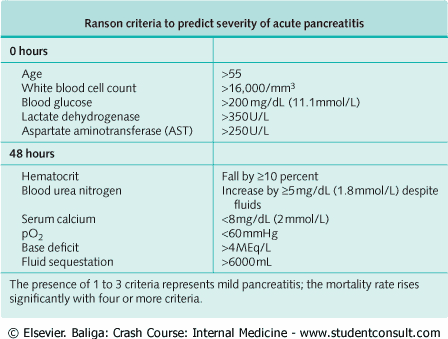
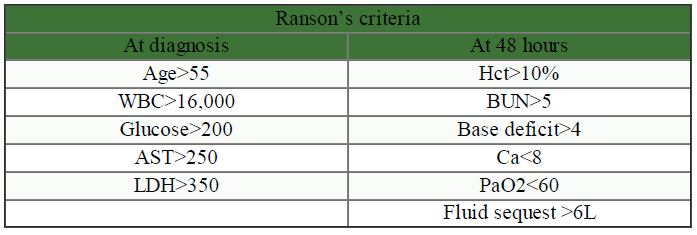
- Predictive factors:
- Hemorrhage (Gray-Turner, Cullen’s, delayed 48h),
- Pancreatic enzymes (low levels more consistent with necrosis),
- Severity of pancreatitis (Ranson’s criteria)
- Hemoconcentration: Hct >47% at 48h has high sensitivity and may need CT early in course (Am J Gastroenterol 1998;93:2130-4)
- Treatment
- Antibiotics (Imipenem), CT A/P, Urgent surgical consultation, ICU
- CT or U/S guided drainage for fluid collections
- Infected pancreatic collections benefit from early surgery
- SEPSIS
- Responsible for most mortality associated with Acute Pancreatitis
- See Sepsis algorithm
- PSEUDOCYST
- Drainage, >6cm after 6 weeks observation, or causing symptoms (abdominal pain, gastric outlet obstruction, biliary obstruction)
- Other
- ↓ Ca, ↑ glucose, ↑ TG, GI hemorrhage, ascites, pleural effusion, ARDS, renal failure
Read More: Acute Pancreatitis – Approach, Evaluation and Management
3. Gastritis , GERD , Peptic Ulcer Disease
General
- If patient stable, often considered default diagnosis when work-up negative and excluded lifethreats (MI, perforation…)
- Empiric therapy given with abdomen re-check
Clinical
- Gastroesophageal reflux disease (GERD): Heartburn, atypical angina, water brash, cough
- Gastritis: Asymptomatic vs epigastric pain, N/V, anorexia
- Peptic Ulcer Disease: Epigastric pain relieved (duodenal) or worsened (gastric) by food; back pain & elevated lipase (post perforation)
Treatment
- Lifestyle change (elevation of head when sleeping), stop precipitants (NSAIDS / alcohol)
- H. Pylori treatment, antacid / H2 blocker / PPI
Complications
- Peptic Ulcer Disease:
- Hemorrhage, Perforation, Intractable pain, Obstruction
- Posterior perforation may present like pancreatitis (back pain, elevated enzymes, vomiting…)
Read More: From Heartburn to Ulcers – Understanding Peptic Ulcer Disease
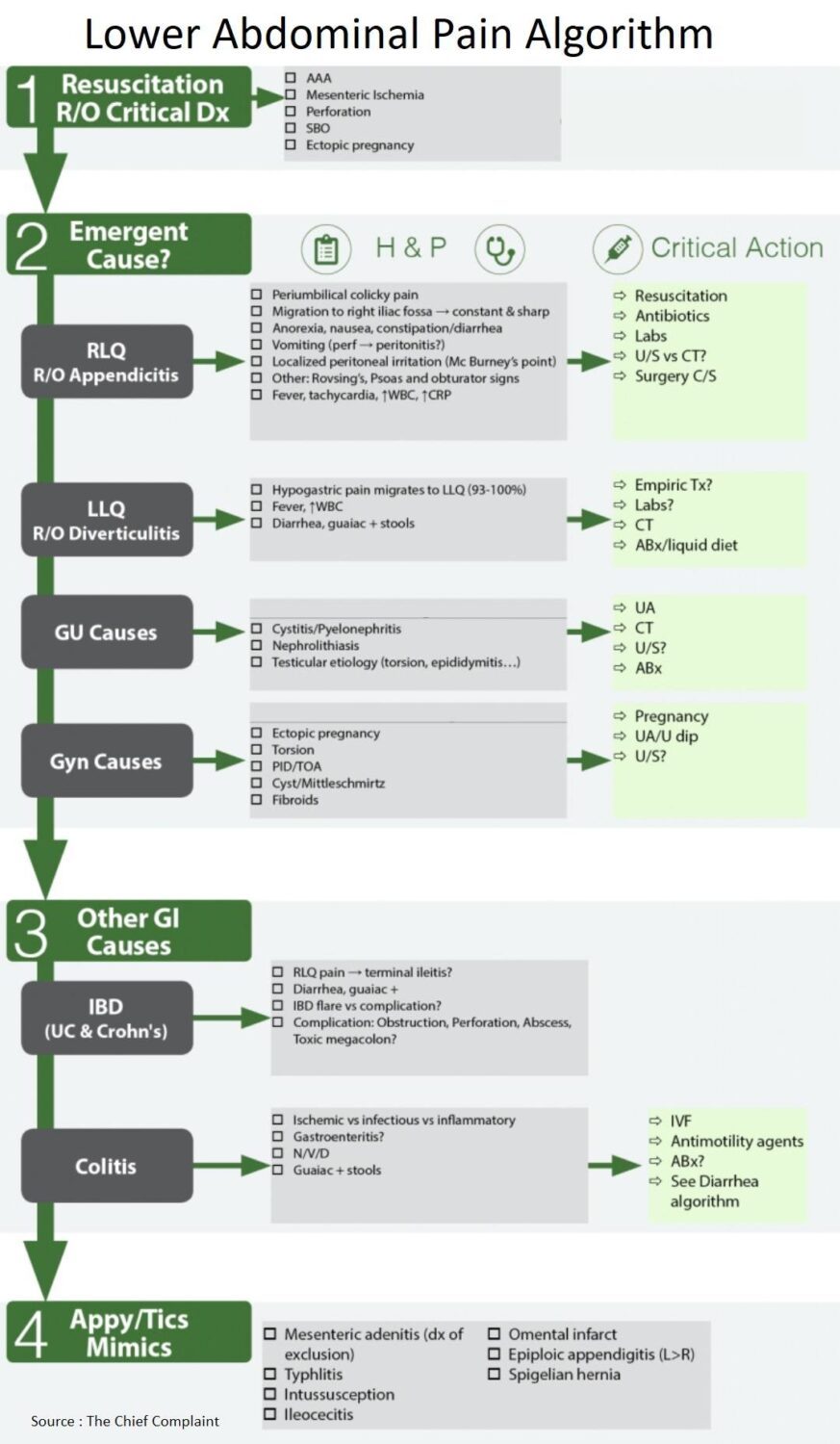
Emergent Causes of Lower Abdominal Pain
- Appendicitis
- Diverticulitis
- Pyelonephritis
- Nephrolithiasis
- Torsion / Pelvic inflammatory disease (PID) / TOA
- Acute Scrotum
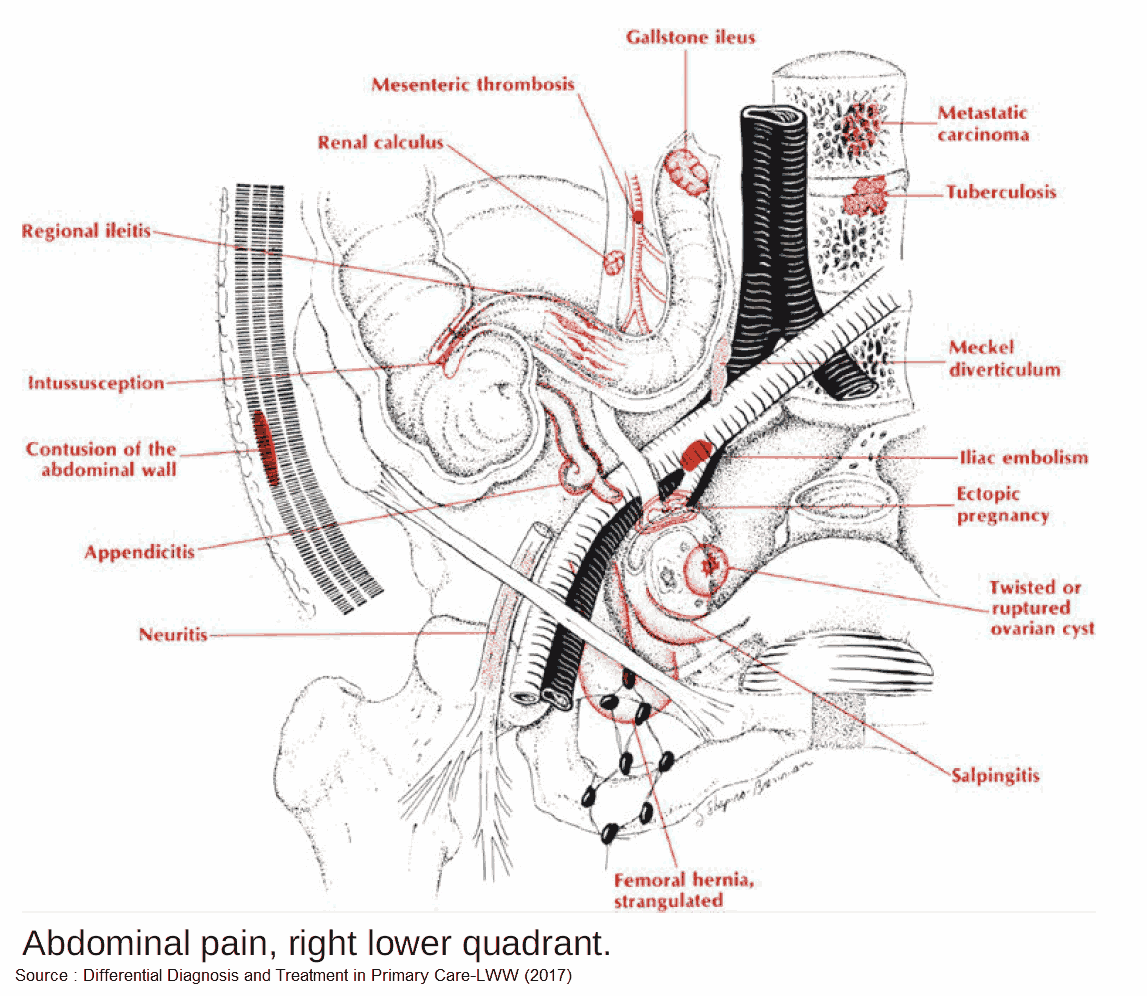
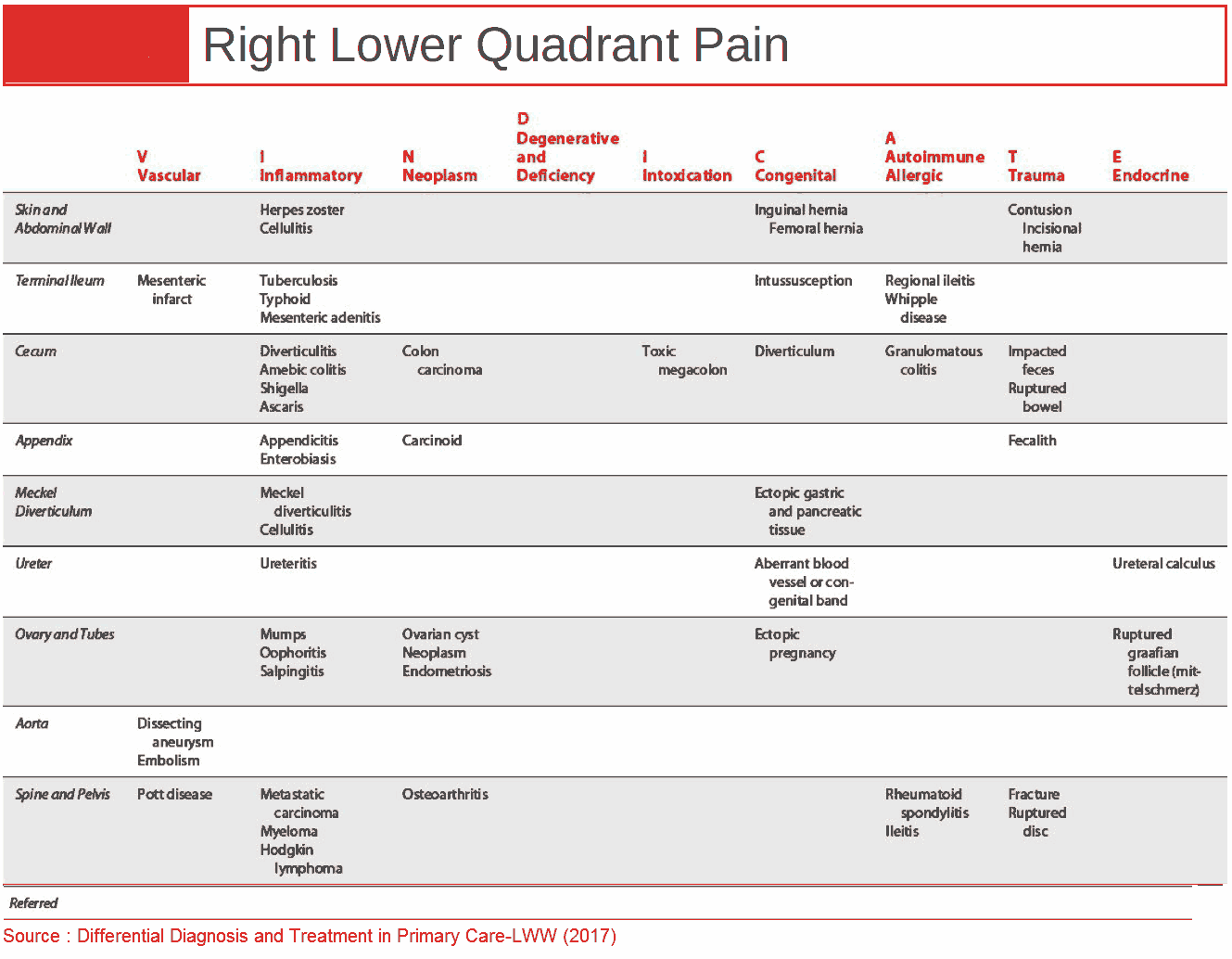
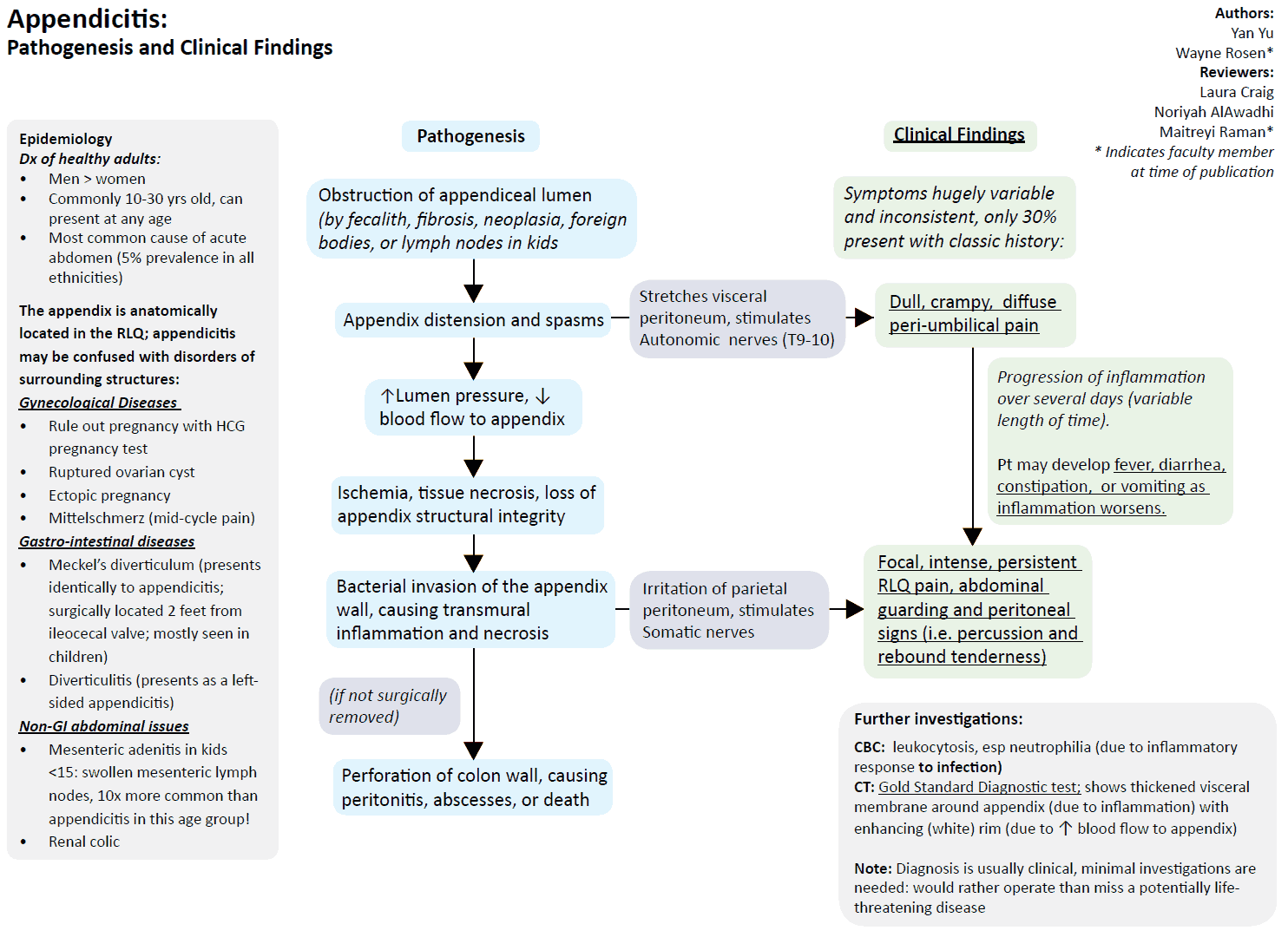
1. Appendicitis
Symptoms
- Abdominal pain
- Periumbilical colicky pain
- Migration to right iliac fossa, constant and sharp
- Localized peritoneal irritation (McBurney’s point)
- Rovsing’s (palpation in LLQ elicits pain in RLQ)
- Psoas (pain on passive extension of thigh or active flexion of hip, seen in retrocecal appendicitis)
- Obturator signs (pain on flexion and internal rotation of hip)
- Anorexia, nausea / vomiting, constipation / diarrhea
- Fever, tachycardia, High WBC, High CRP
- Strongest predictors of appendicitis: (Meta-analysis Brit J Surg 2004;91:28-37)
- Inflammatory response variables (PMN, WBC, CRP)
- Peritoneal irritation (rebound, percussion tenderness, guarding, rigidity)
- Migration of pain (epigastric/periumbilical then RLQ (right lower quadrant))
- Patients at extremes of age may have non-specific symptoms, may cause diagnostic difficulty
Work-up for Appendicitis (Ann Intern Med 2004;141:537-46)
- Ultrasound
- Aperistaltic and non-compressible structure > 6mm
- Sensitivity 86%; Specificity 81%
- CT
- Abnormal appendix, calcified appendicolith + periappendiceal inflammation or diameter > 6mm
- Sensitivity 94%; Specificity 95%
READ MORE: Imaging of Acute Pancreatitis: to Image or Not to Image
Treatment of Appendicitis
- Resuscitation
- Large bore IV, IV Fluids
- Pain control
- Opiate administration has no significant association with management errors (JAMA 2006;296:1764-1774)
- Antibiotics
- Broad spectrum, empiric
- Lower Incidence of postoperative wound infection and intra-abdominal abscess formation (Cochrane Database Syst Rev 2005;(3):CD001439)
- Antibiotics alone for treatment? (Lancet. 2011:377(9777):1573)
- Spontaneous resolution can also occur
- 1 year recurrence rate with antibiotics as sole therapy, 15% most within 10 days
- Surgery
- Risk of rupture in 0-36h is < 2%
- Each ensuing 12h period after 36h is 5%
- Timing (Arch Surg 2006;141:504-7)
- No significant difference between early (<12h after presentation) and later (12- 24h) appendectomy
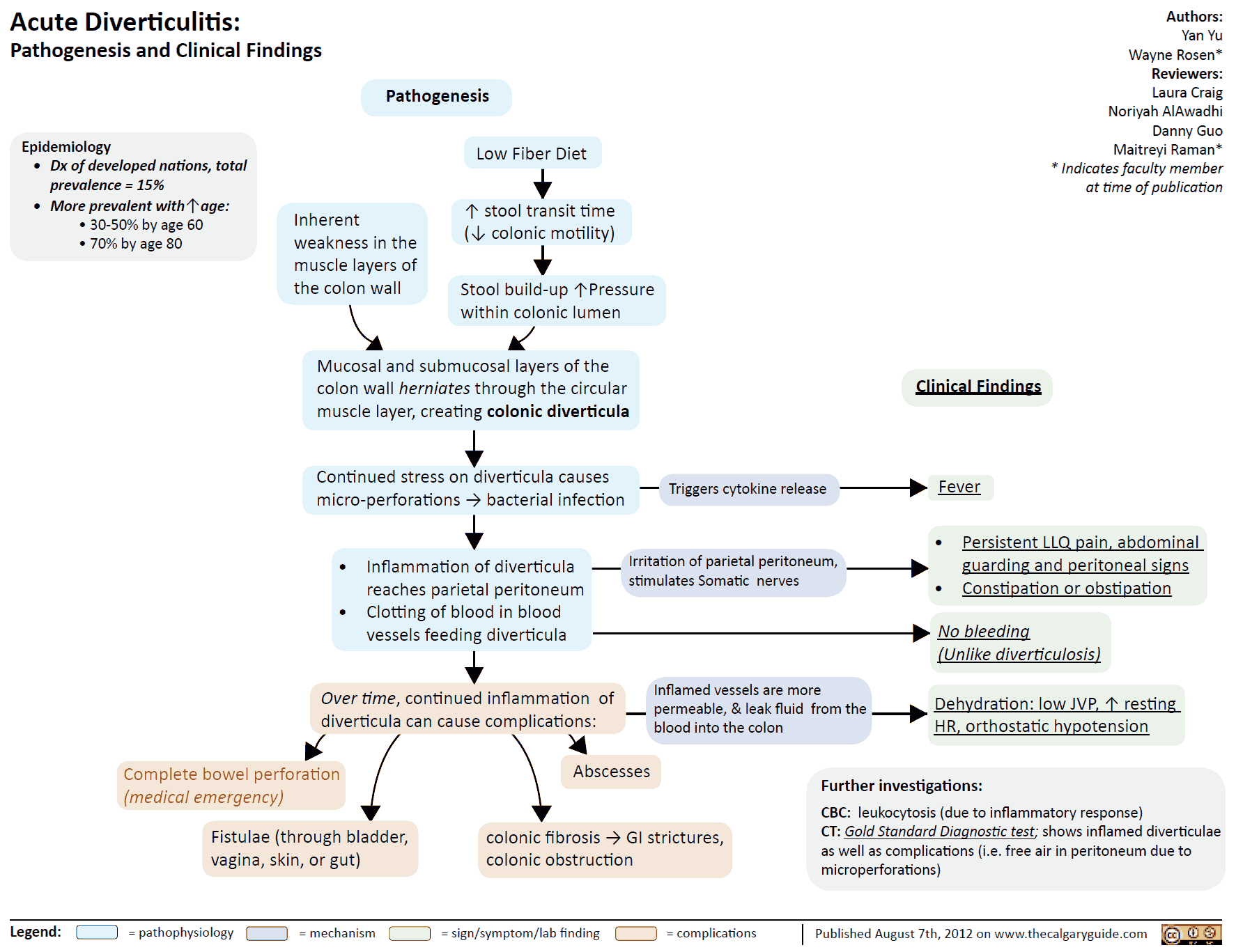
2. Diverticulitis
Clinical Presentation
- Presents like appendicitis, but of the LLQ (lower left quadrant)
- Hypogastric pain migrates to LLQ (93-100%)
- Fever, High WBC
- Diarrhea, guaiac + stools
Work-up for Diverticulitis (Am J Roentgenol 2002;178:1313-8)
- Empiric treatment
- No imaging studies needed if diagnosis is clear-cut, can begin empiric treatment
- CT
- Sensitivity 69-95%, Specificity 75-100%
- Use for uncertain diagnosis, exclude other causes of abdominal pain, rule out diverticular complications, or clinical deterioration
- Findings: bowel wall thickening (96%), fat stranding (95%), detects complications (free air, abscess, phlegmons, cancer)
- Ultrasound
- Sensitivity 84%, Specificity 93%
- Rule out AAA, hypoechoic bowel wall thickening, diverticula, abscess, hypoechoic around bowel wall
Complications of Diverticulitis (Emerg Med Clin N Am 2003;21:937-969)
- Abscess
- Can lead to fistula formation and sepsis
- Free perforation, peritonitis
- Rupture of diverticular abscess leading to acute surgical abdomen
- More common In elderly and immunosuppressed, high mortality (6-25%)
- Fistula
- Fistula between colon and surrounding structures: colovesicular, colovaginal, colocutaneous, coloenteric
- Colovesicular fistula most common (dysuria, pyuria, pneumaturia, fecaluria)
- Obstruction
- Uncommon, 2% of cases
- May cause Small-Bowel Obstruction when loops of bowel entangled in peridiverticular adhesions
Treatment of Diverticulitis
- Outpatient
- Indication: Mild symptoms, tolerating oral fluids, well appearing (Am Fam Physician 2005;72(7):1229)
- Antibiotics, 7-10days (Amoxicillin / Clavulanic acid, TMP/SMX (Trimethoprim / Sulfamethoxazole), ciprofloxacin/metronidazole)
- Liquid diet, may consider no antibiotics in extremely well appearing patients (Br J Surg 2012;99(4):532)
- If no improvement in 2-3 days consider peridiverticular disease (reassessment and admission?)
- Inpatient
- Indication: Severe symptoms requiring narcotics, unable to tolerate oral fluids, elderly, comorbid illnesses, ill/septic, no home support or follow-up
- IV antibiotics (gram negative/anaerobes), bowel rest
- Laparotomy in: generalized peritonitis, sepsis, visceral perforation, clinical deterioration
3. Pyelonephritis
4. Nephrolithiasis
Other Causes of Lower Abdominal Pain
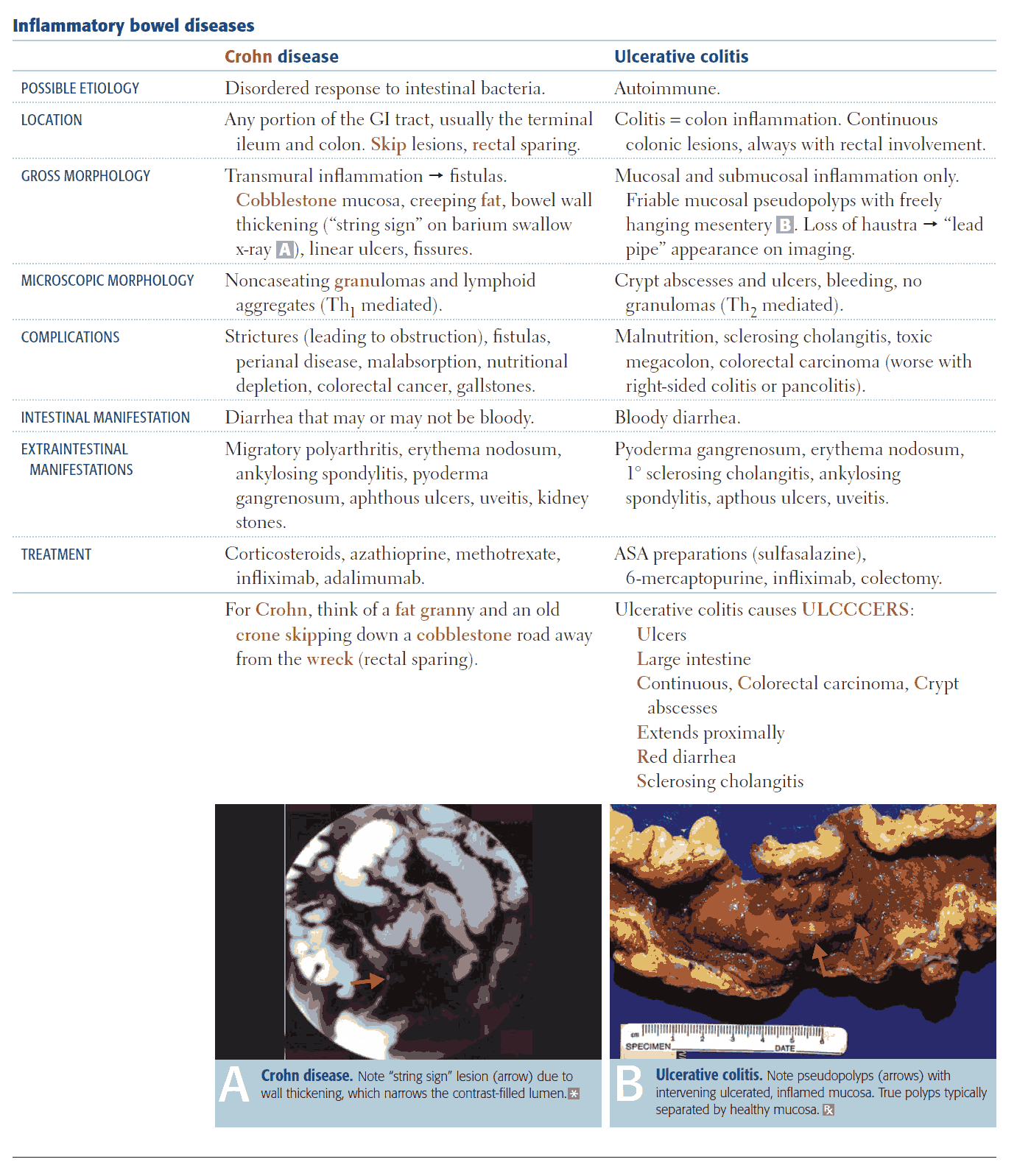
1. IBD (Inflammatory bowel disease)
Clinical Presentation
- RLQ pain often indicates terminal ileitis
- Diffuse abdominal pain, diarrhea, guaiac +
Complications
- May be difficult to distinguish “flare” from an acute complication, consider further diagnostic imaging
- TOXIC MEGACOLON
- Define: Lethal complication of IBD or infectious colitis, total or segmental nonobstructive colonic dilatation plus systemic toxicity
- Clinical: abrupt onset bloody diarrhea, fever, high WBC, tachycardia, third space losses, ill appearing, abdominal distension, perforation (peritoneal signs may be masked by steroids)
- Therapy: Resuscitation, blood transfusion, broad spectrum antibiotics, corticosteroids, +/- immunosuppressants, bowel rest and bowel decompression
- Surgery: indicated if no improvement on medical therapy (subtotal colectomy with endileostomy)
- Hemorrhage: (CD > UC), Resuscitation, blood transfusion, surgery consult (bowel resection?)
- Other: Obstruction, Perforation, Abscess
2. Colitis
- Etiology
- Ischemic vs infectious vs inflammatory
- Mesenteric Ischemia
- Clinical Presentation
- Gastroenteritis ?
- N/V/D
- Guaiac + stools
3. Other Appendicitis Mimics
- Mesenteric adenitis (diagnosis of exclusion)
- Typhlitis
- Intussusception
- Ileocecitis
- Omental infarct
- Epiploic appendigitis (L>R)
- Spigelian hernia
References
- Ranji SR, Goldman LE, Simel DL, Shojania KG. Do Opiates Affect the Clinical Evaluation of Patients With Acute Abdominal Pain? JAMA. 2006;296(14):1764–1774. doi:10.1001/jama.296.14.1764
- Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004 Oct 5;141(7):537-46. doi: 10.7326/0003-4819-141-7-200410050-00011. PMID: 15466771.
- Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg. 2004 Jan;91(1):28-37. doi: 10.1002/bjs.4464. PMID: 14716790.
- Abou-Nukta F, Bakhos C, Arroyo K, et al. Effects of Delaying Appendectomy for Acute Appendicitis for 12 to 24 Hours. Arch Surg. 2006;141(5):504–507. doi:10.1001/archsurg.141.5.504
- Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, Karoui M, Alves A, Dousset B, Valleur P, Falissard B, Franco D. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011 May 7;377(9777):1573-9. doi: 10.1016/S0140-6736(11)60410-8. PMID: 21550483.
- Andersen BR, Kallehave FL, Andersen HK. Antibiotics versus placebo for prevention of postoperative infection after appendicectomy. Cochrane Database Syst Rev. 2005 Jul 20;2005(3):CD001439. doi: 10.1002/14651858.CD001439.pub2. PMID: 16034862; PMCID: PMC8407323.
- Eglinton TW. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis (Br J Surg 2012; 99: 532-539). Br J Surg. 2012 Apr;99(4):540. doi: 10.1002/bjs.8687. PMID: 22396052.
- Salzman H, Lillie D. Diverticular disease: diagnosis and treatment. Am Fam Physician. 2005 Oct 1;72(7):1229-34. PMID: 16225025.
- Hendrickson M, Naparst TR. Abdominal surgical emergencies in the elderly. Emerg Med Clin North Am. 2003 Nov;21(4):937-69. doi: 10.1016/s0733-8627(03)00072-5. PMID: 14708814.
- Kircher MF, Rhea JT, Kihiczak D, Novelline RA. Frequency, sensitivity, and specificity of individual signs of diverticulitis on thin-section helical CT with colonic contrast material: experience with 312 cases. AJR Am J Roentgenol. 2002 Jun;178(6):1313-8. doi: 10.2214/ajr.178.6.1781313. PMID: 12034590.