This post is an answer to the Case – Skin Lesion in a Patient on Haemodialysis
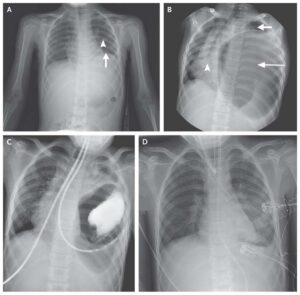
Radiography of the soft tissue revealed diffuse calcified arterioles in a mesh-like pattern (image). Histological examination of skin biopsy showed sclerosis and thrombosis of blood vessels (image) and von Kossa stains were positive for calcium deposits (image), confirming the diagnosis of calciphylaxis.
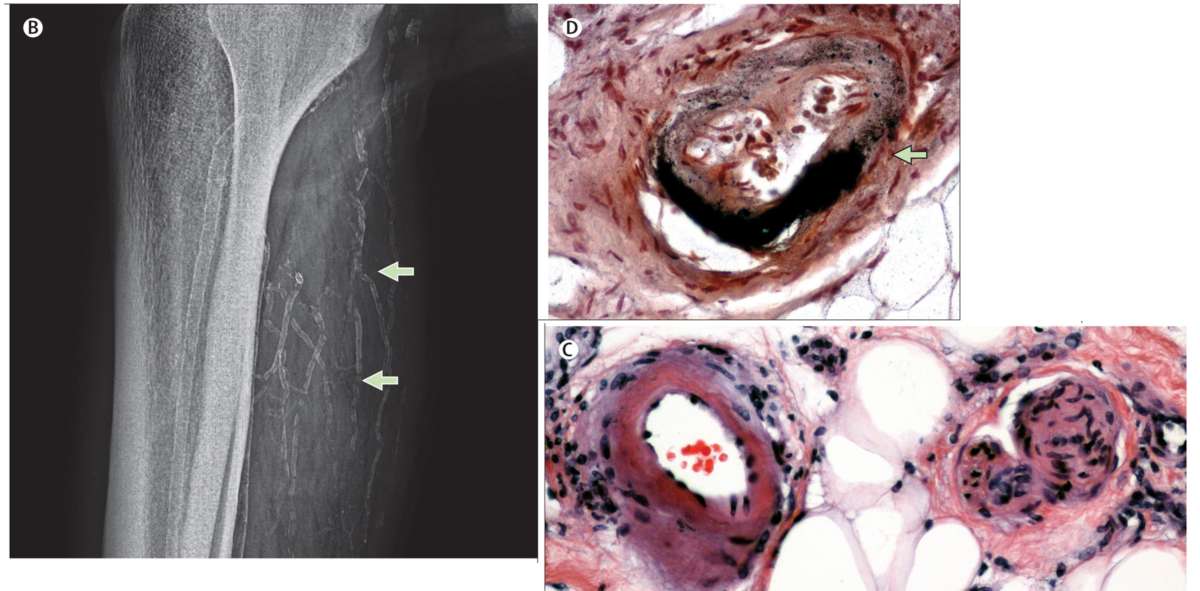
(C) Histological examination of skin biopsy from the ulceration: calcific sclerosis and microthrombi within a small artery (haematoxylin and eosin stain, magnification ×200).
(D) Calcium deposition of an artery (von Kossa stain, magnification ×200); calcium deposits are highlighted as dark granules (arrow).
Discussion
Calciphylaxis is a syndrome of systemic medial calcification of the arteries leading to tissue necrosis. Skin biopsy and radiographic features are helpful in the diagnosis; but negative results do not necessarily exclude the diagnosis.
Although the pathogenesis remains unclear, several comorbid conditions are known to increase its development. Associated risk factors in our patient were: end-stage renal disease, secondary hyperparathyroidism, and oral anticoagulation with phenprocoumon.
Recent reports indicate that low parathyroid hormone levels in association with adynamic bone diseases can also be associated with calciphylaxis.
Unfortunately, there is still no standardised treatment for calciphylaxis. Based on previous reports, phenprocoumon was withdrawn in our patient and he was treated with cinacalcet, daily haemodialysis, sodium thiosulfate, and bisphosphonate. After 4 weeks, skin condition improved and the patient was discharged home.