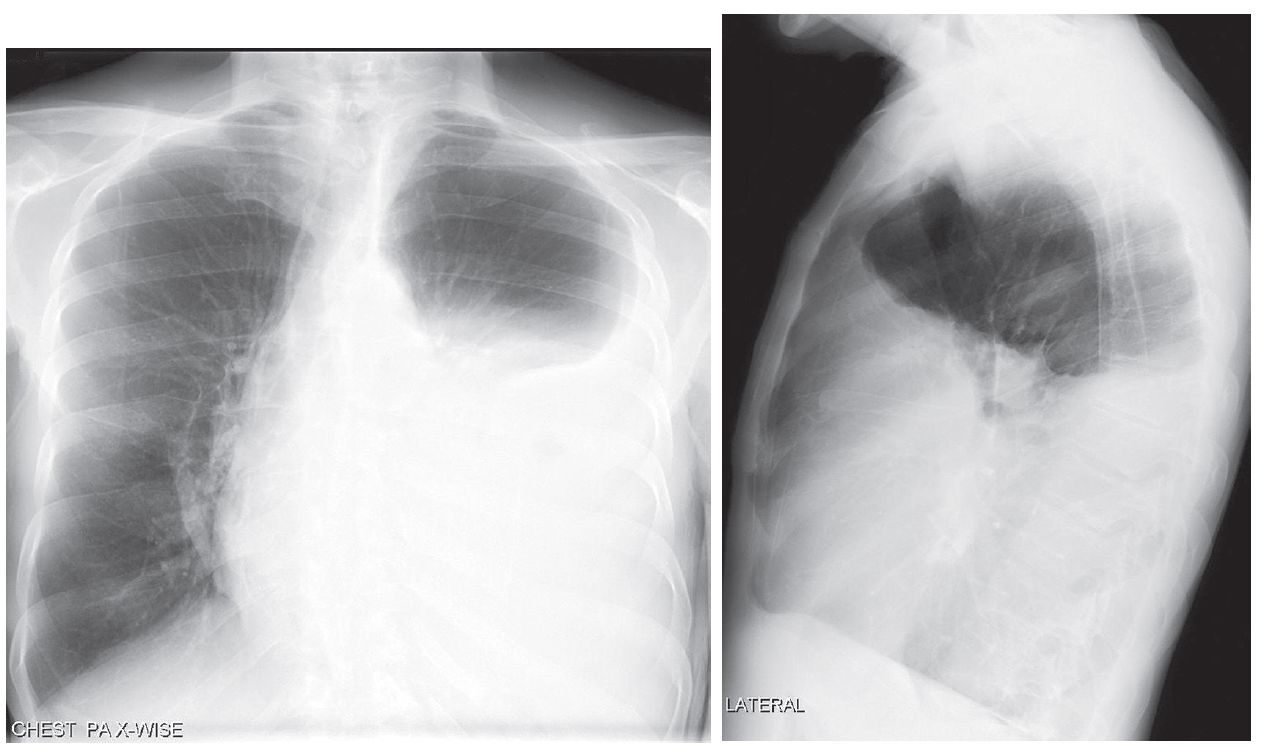
PA and lateral chest X-rays show opacification of nearly two-thirds of the left hemithorax. Note the airless left mid- and lower thorax and contralateral mediastinal shift from this pleural space-occupying process.
The lateral exam also demonstrates a positive spine sign characterized by increased opacity over the lower thoracic spine and obscuration of the left diaphragm.
Differential Diagnosis
- Atelectasis
- Parenchymal Consolidation
Relaxation (passive) atelectasis
Relaxation (passive) atelectasis occurs when there is loss of contact between the visceral and parietal pleurae by a space-occupying process (e.g., pleural effusion, pneumothorax) exerting extrinsic pressure on the parenchyma.
The elastic recoil properties of the lung preserve its shape as it loses volume. In the absence of pleural adhesions, the degree of atelectasis is proportional to the volume of fluid or air in the pleural space.
Mantle or compressive atelectasis is a subtype of relaxation atelectasis resulting from a space-occupying lesion exerting intrinsic pressure on the lung, forcing air out of the alveoli.
Mantle atelectasis may occur in response to large bullous lesions as well as from dominant intraparenchymal lung masses, loculated pleural fluid collections, chest wall–based lesions, and subdiaphragmatic disease (e.g., massive ascites)
Clinical Findings
If atelectasis is secondary to massive pleural effusion, as in this case, the affected hemithorax is dull to percussion with diminished breath sounds on auscultation.
The severity of dyspnea depends on the patient’s underlying respiratory reserve and the rate at which the fluid accumulated. The gradual accumulation of fluid over time allows the patient to accommodate for the volume loss. Such patients may be less symptomatic.
Imaging Findings
- Upper lobes demonstrate greater degree of relaxation atelectasis with pneumothorax
- Lower lobes exhibit greater degree of relaxation atelectasis with pleural effusion
- Cartilaginous support of lobar and segmental bronchi allows them to resist collapse, remain air-filled, and manifest as air bronchograms
Management
Directed toward underlying disease process and evacuation of pleural fluid or air when necessary
Prognosis
In the absence of pleural adhesions, once the pleural air or fluid collection is evacuated, the elastic recoil properties of the chest wall and affected lung allow it to re-expand and function normally