Table of Contents
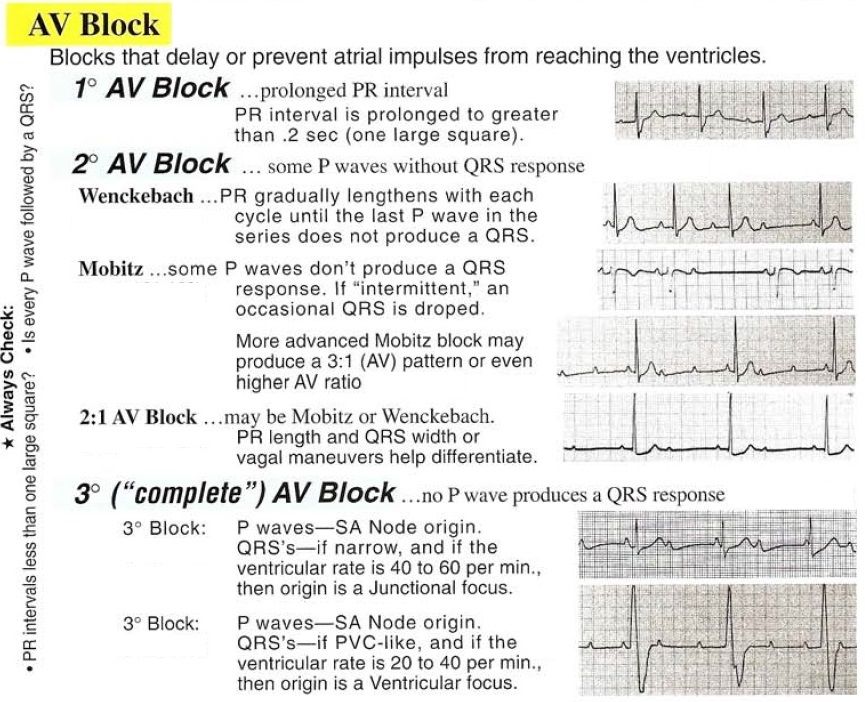
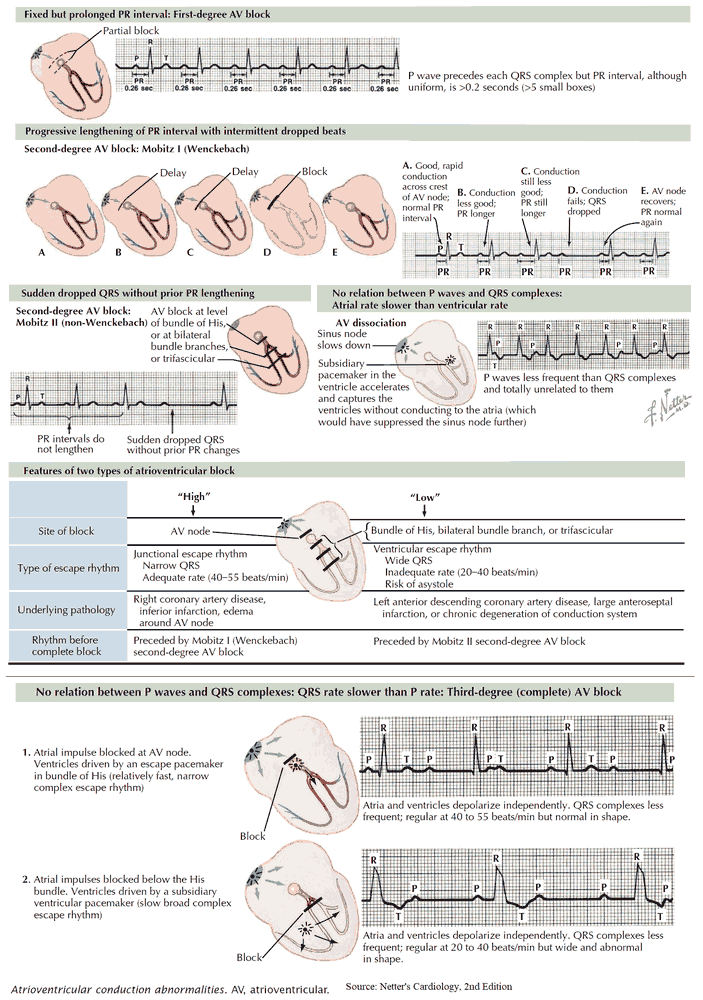
When there are conduction problems at the AV node or bundle of His, conduction of impulses between the atria and ventricles is affected. This can take several forms or ‘degrees’.
- First-degree AV block
- Second-degree AV block
- Mobitz type I AV block (Wenckebach phenomenon)
- Mobitz type II AV block
- 2:1 AV Block
- Third-degree AV Block
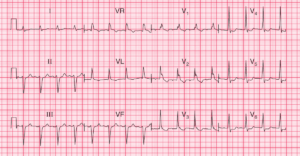
First-degree AV block
In first-degree AV block, conduction through the AV node is slower than usual and the PR interval is therefore prolonged. Nonetheless, every P wave is followed by a QRS complex and therefore there are no ‘dropped’ beats.
The normal PR interval is 0.12–0.20 s, and so first-degree AV block is diagnosed when the PR interval measures >0.20 s.
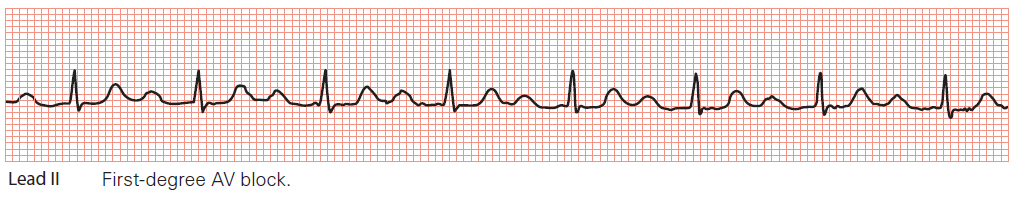
Key point: • The PR interval is prolonged at 0.28 s.
Causes of First-degree AV block
First-degree AV block is a common feature of vagally induced bradycardia, as an increase in vagal tone decreases AV nodal conduction. It may also be a feature of:
- ischaemic heart disease
- hyperkalaemia or hypokalaemia
- acute rheumatic myocarditis
- Lyme disease
- drugs:
- beta blockers
- rate-modifying calcium channel blockers
- digoxin.
Treatment of First-degree AV block
First-degree AV block in itself is asymptomatic and, in general, does not progress to other sorts of heart block (these are described later).
No specific treatment is necessary for first-degree AV block in its own right, but it should alert you to one of the above diagnoses (which may require treatment). First-degree AV block is not an indication for a pacemaker.
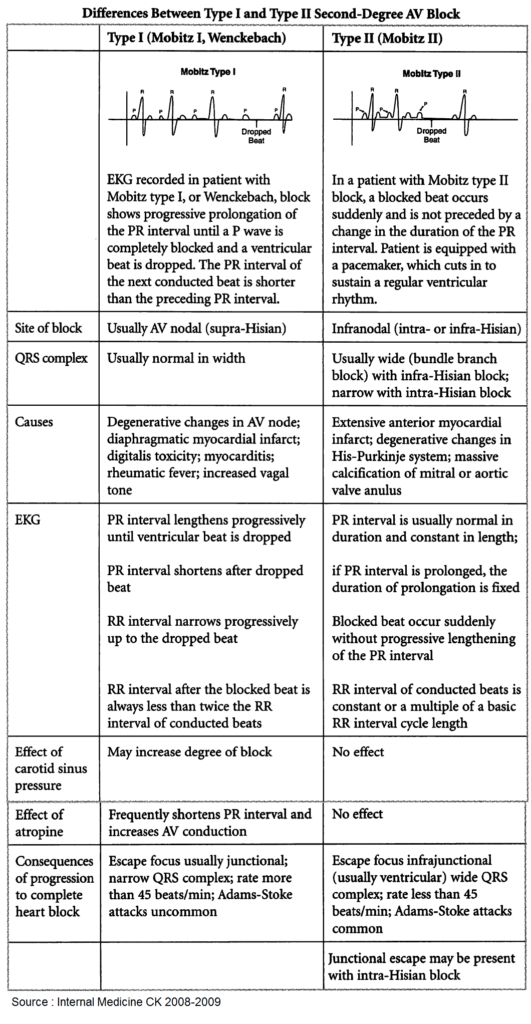
Second-degree AV block
In second-degree AV block, there starts to be an intermittent failure of AV conduction and as a result some P waves are not followed by QRS complexes. There are three types of second-degree AV block:
- if the PR interval gradually lengthens with each beat, until one P wave fails to produce a QRS complex, the patient has Mobitz type I AV block
- if the PR interval is fixed and normal, but occasionally a P wave fails to produce a QRS complex, the patient has Mobitz type II AV block
- if alternate P waves are not followed by QRS complexes, the patient has 2:1 AV block.
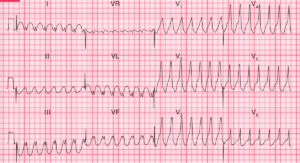
1. Mobitz type I AV block (Wenckebach phenomenon)
Mobitz type I AV block, also known as Wenckebach phenomenon, is usually a consequence of conduction problems within the AV node itself, sometimes simply as a result of high vagal tone – for instance, it is more commonly seen during sleep, and has a higher prevalence in athletes.
Its characteristic features are:
- the PR interval shows progressive lengthening until one P wave fails to be conducted and fails to produce a QRS complex
- the PR interval resets to normal and the cycle repeats.
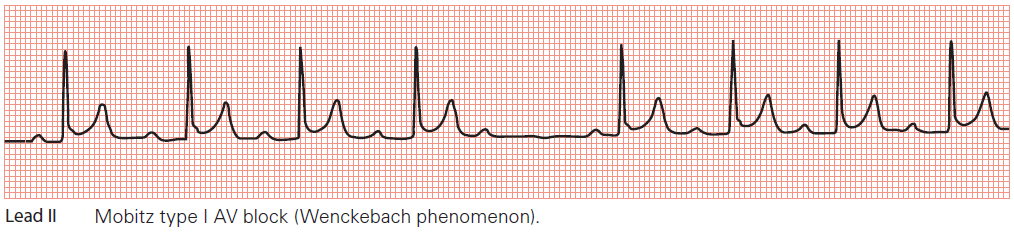
Key points: • The PR interval gradually lengthens until a P wave fails to be conducted.
• The PR interval resets, and the cycle repeats.
One can imagine Mobitz type I AV block as the AV node becoming increasingly ‘tired’ as it conducts each P wave – as a result, the node takes longer and longer to conduct each subsequent P wave until it totally ‘gives up’ and fails to conduct a P wave at all. This, however, gives the AV node a chance to ‘rest’, and by the time the next P wave arrives it is ready to conduct normally, before the cycle repeats itself.
When Mobitz type I AV block occurs at the level of the AV node it is generally regarded as ‘benign’, and a permanent pacemaker is not required unless the frequency of ‘dropped’ ventricular beats causes a symptomatic bradycardia.
When the block is distal to the AV node – infranodal (as identified by electrophysiological testing), in which case the QRS complexes may be wide, there is a stronger indication for pacing, even if patients are asymptomatic.
Treatment of Mobitz type I AV block
- In Mobitz type I AV block in the setting of acute myocardial infarction, pacing may be required depending on the type of infarction.
- In anterior myocardial infarction, a prophylactic temporary pacemaker is recommended in case third- degree ( complete) heart block develops.
- In inferior myocardial infarction, a pacemaker is only needed if symptoms or haemodynamic compromise result.
- Patients found to have Mobitz type I AV block prior to surgery will usually require temporary pacing perioperatively – discuss this with the anaesthetist and a cardiologist.
2. Mobitz type II AV block
Mobitz type II AV block is usually a consequence of conduction problems distal to the AV node (infranodal). As a result, there is a higher risk of progression to third-degree AV block and the prognosis is therefore worse than for Mobitz type I AV block.
Its characteristic features are:
- most P waves are followed by a QRS complex
- the PR interval is normal and constant
- occasionally, a P wave is not followed by a QRS complex.
Mobitz type II AV block is thought to result from abnormal conduction below the AV node (infranodal) and is considered more serious than Mobitz type I as it can progress without warning to third-degree (complete) heart block. Referral to a cardiologist is therefore recommended, as a pacemaker may be required.
The indications for pacing Mobitz type II AV block in the setting of an acute myocardial infarction, or perioperatively, are the same as for Mobitz type I AV block.
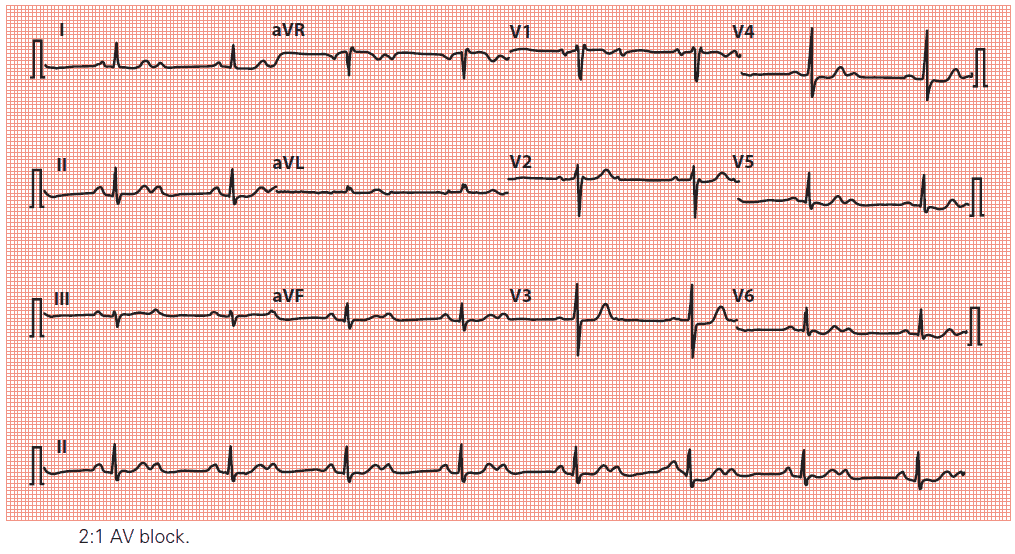
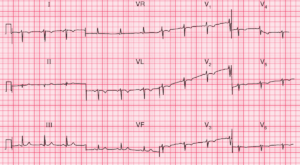
3. 2:1 AV block
2:1 AV block is a form of second-degree AV block that cannot be categorized as Mobitz type I or type II. Because every alternate P wave is missing, it’s impossible to say whether the PR interval would have lengthened or not. It’s therefore traditional to consider 2:1 AV block as a category of second-degree heart block in its own right.
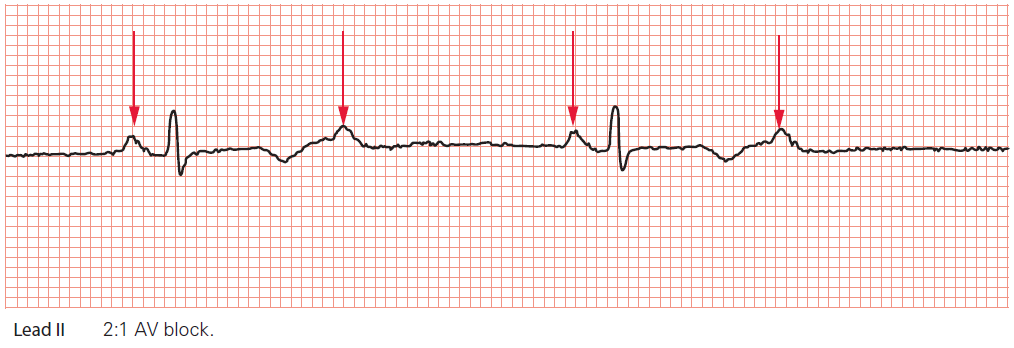
Key point: • The P waves are marked by arrows. Only every alternate P wave is followed by a QRS complex.
Third-degree AV block
In third-degree AV block (‘complete heart block’), there is complete interruption of conduction between atria and ventricles, so that the two are working independently.
The characteristic features of complete heart block are:
- P wave rate is faster than ventricular QRS complexes
- P waves bear no relationship to the ventricular QRS complexes
- if block occurs in the AV node, QRS complexes are usually narrow due to a subsidiary pacemaker arising in the bundle of His
- if block occurs below the AV node, QRS complexes are usually broad due to a subsidiary pacemaker arising in the left or right bundle branches.
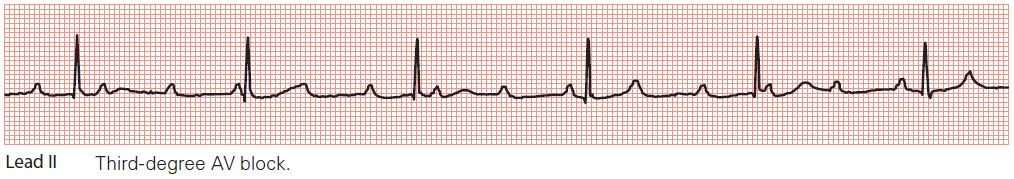
Key point: • There is a complete block of AV conduction, with sinus rhythm in the atria and a narrow complex
(‘junctional’) escape rhythm in the ventricles.
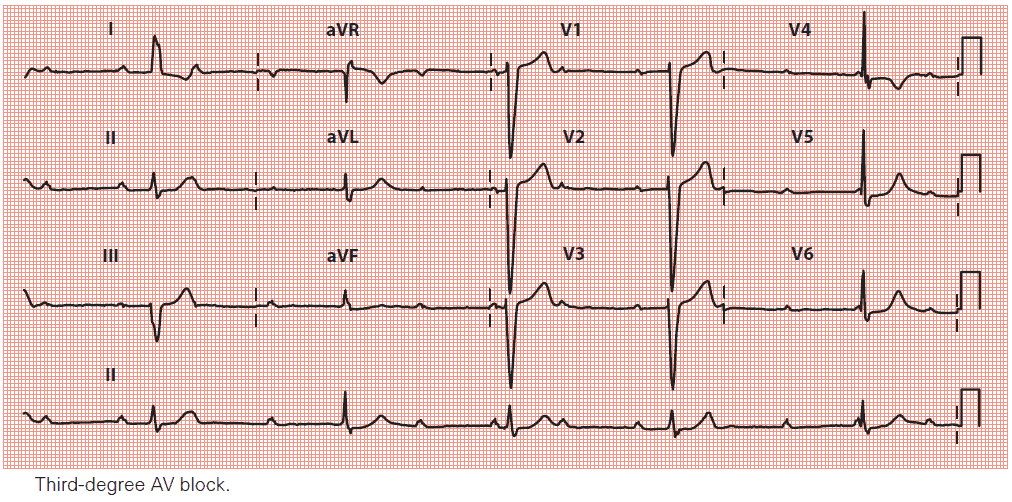
Key points: • The P wave (atrial) rate is approximately 75/min, with a QRS complex (ventricular) rate of approximately 30/min.
• There is no relationship between P waves and QRS complexes.
QRS complexes usually arise as the result of a ventricular escape rhythm, in which the QRS complexes are usually broad. However, if the level of AV block is located in or just below the AV node, a junctional escape rhythm may arise with narrow QRS complexes.
It is important to remember that any atrial rhythm can coexist with third-degree AV block, and so the P waves may be abnormal or even absent. A combination of bradycardia (ventricular rate usually 15–40/min) and broad QRS complexes should alert you to suspect third-degree AV block.
Third-degree AV block can be congenital or acquired. In congenital cases, which are uncommon, the block is usually at the level of the AV node and is often associated with maternal anti-Ro or anti-La antibodies.
Acquired cases can result from disease processes affecting the AV node and/or the infranodal conduction system.
Causes of third-degree AV block:
- Congenital
- Acquired
- drug toxicity (e.g. anti-arrhythmics)
- fibrosis/calcification of the conduction system
- myocardial ischaemia/infarction
- infection (e.g. Lyme disease)
- myocardial infiltration (e.g. amyloid, sarcoid)
- neuromuscular diseases (e.g. myotonic muscular dystrophy)
- metabolic disorders (e.g. hypothyroidism)
- cardiac procedures (e.g. ablation procedures, aortic valve surgery).
LYME DISEASE
In a patient with a recent onset of third-degree AV block, always consider the possibility of Lyme
disease. This is transmitted by the spirochaete Borrelia burgdorferi and, in the second stage
of the illness, can lead to first-degree, second-degree or third-degree AV block. The AV block
can resolve entirely in response to antibiotics, although the patient may require support with a
temporary pacemaker during treatment.
Treatment of third-degree AV block
In most cases, acquired third-degree AV block requires a permanent pacemaker. An exception to this is if there is a reversible cause (such as drug toxicity, e.g. betablockers, or infection, such as Lyme disease), in which case the patient may only require supportive treatment (which may include temporary pacing) until the cause has been treated and the AV block has resolved.
- In acute inferior wall myocardial infarction, third-degree AV block requires temporary pacing if the patient has symptoms or is haemodynamically compromised. However, pacing may not be required if the patient is asymptomatic and has a ventricular rate >35/min.
- In acute anterior wall myocardial infarction, the development of third-degree AV block usually indicates an extensive infarct (and thus a poor prognosis) and temporary pacing is indicated regardless of the patient’s symptoms or haemodynamic state.
- Temporary pacing is also usually necessary perioperatively in patients about to undergo surgery who are found to have third-degree AV block.
ATRIOVENTRICULAR DISSOCIATION
Atrioventricular dissociation is a term that is commonly used interchangeably with third-degree
AV block; however, it does not mean the same thing. Atrioventricular dissociation occurs when
the ventricular (QRS) rate is higher than the atrial (P wave) rate. The opposite is found in thirddegree
AV block. Atrioventricular dissociation usually occurs in the context of an escape rhythm
(from the AV junction or ventricles) during sinus bradycardia, or an acceleration in a subsidiary
focus in the AV junction or ventricles which then overtakes the sinoatrial node, which continues
firing independently
Read Also About : ECG Interpretation