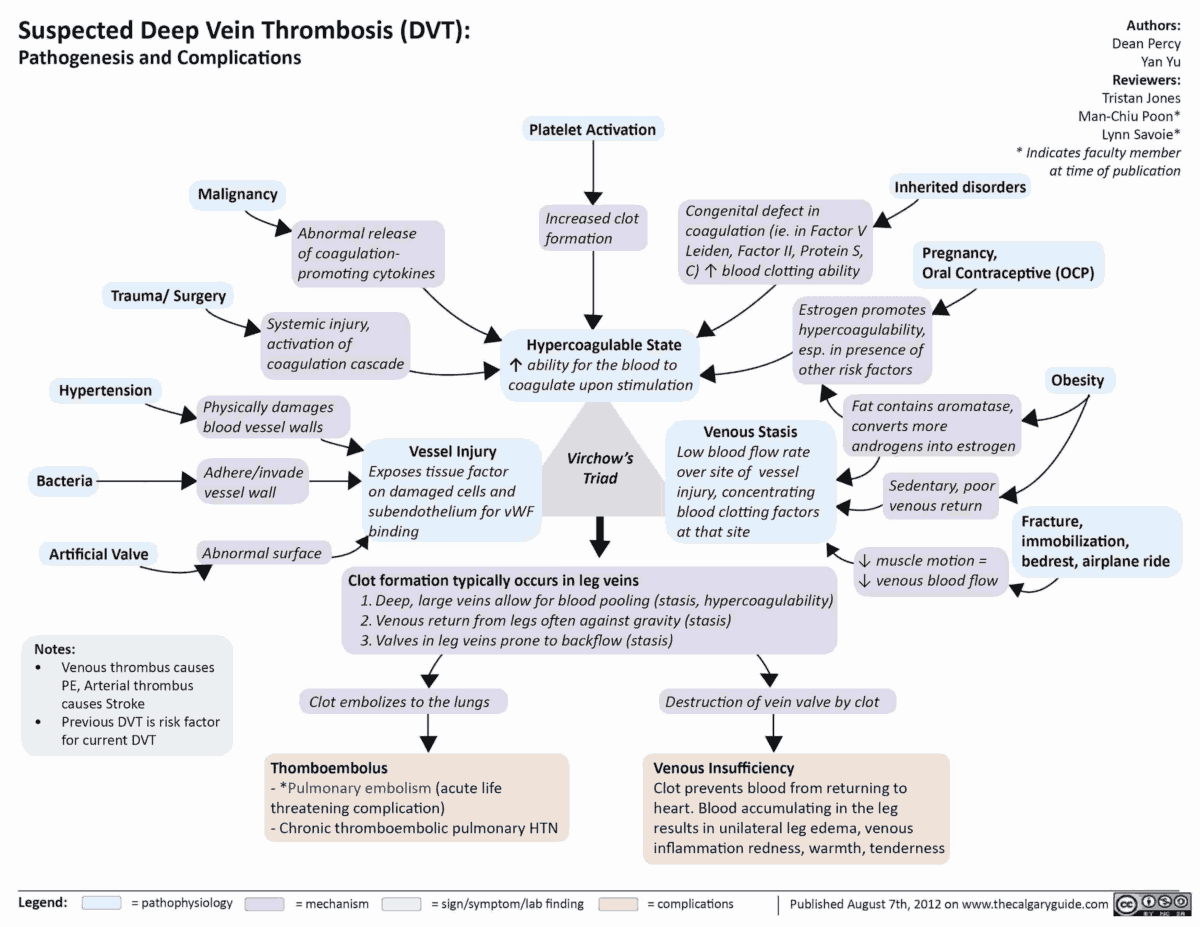
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is responsible for more than 250,000 annual hospitalizations in the United States, with significant risk for morbidity and mortality. The most serious clinical presentation of VTE is acute PE.
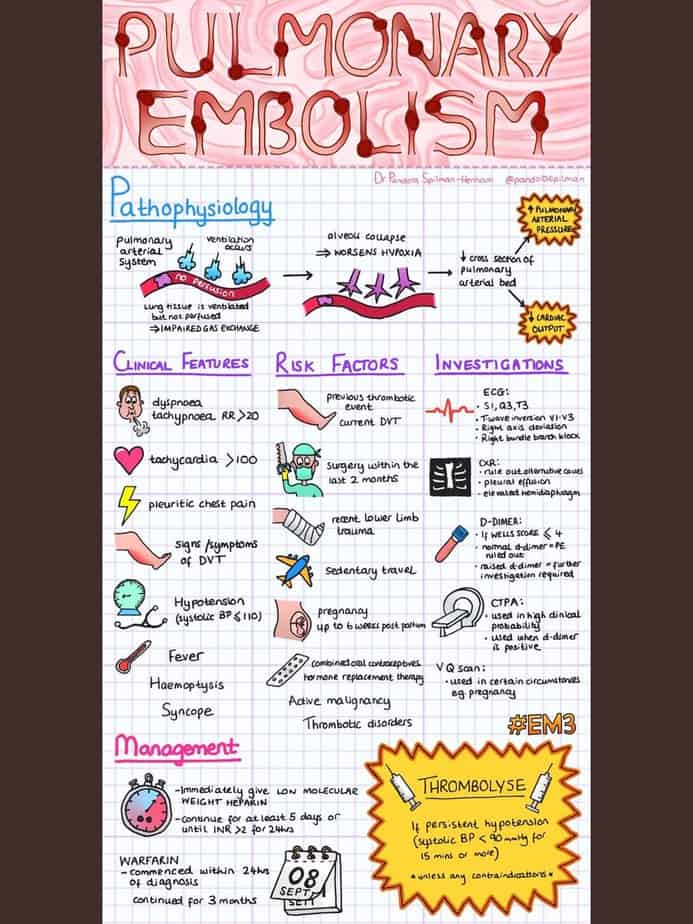
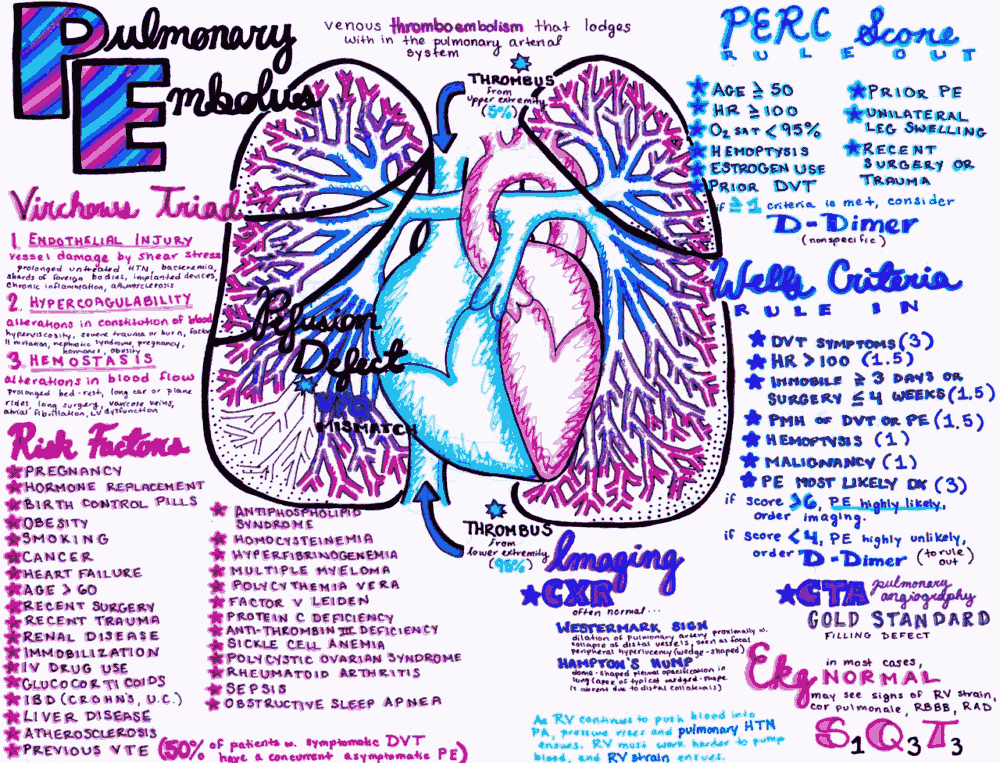
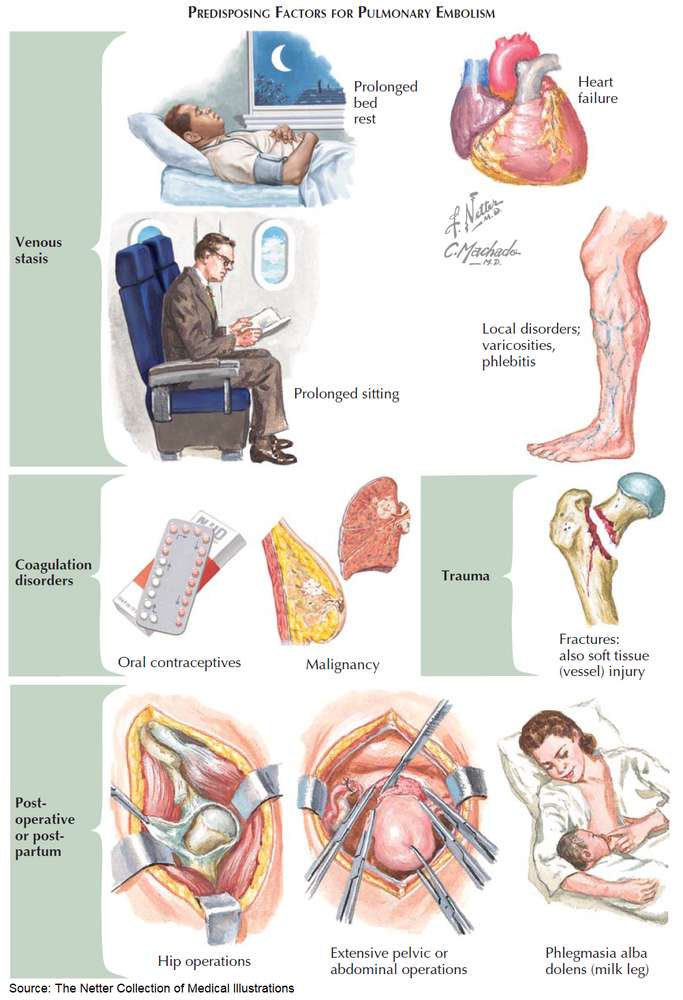
Risk factors for Pulmonary Thromboembolism
Risk factors for VTE must be considered as they may help the provider zero in on the diagnosis of PE.
- Extrinsic risk factors
- Surgery
- Trauma
- Immobilization
- Oral contraceptive or hormonal replacement therapy use
- Intrinsic risk factors
- Hypercoagulable states
- pregnancy, malignancy, and various coagulation disorders
- Hypercoagulable states
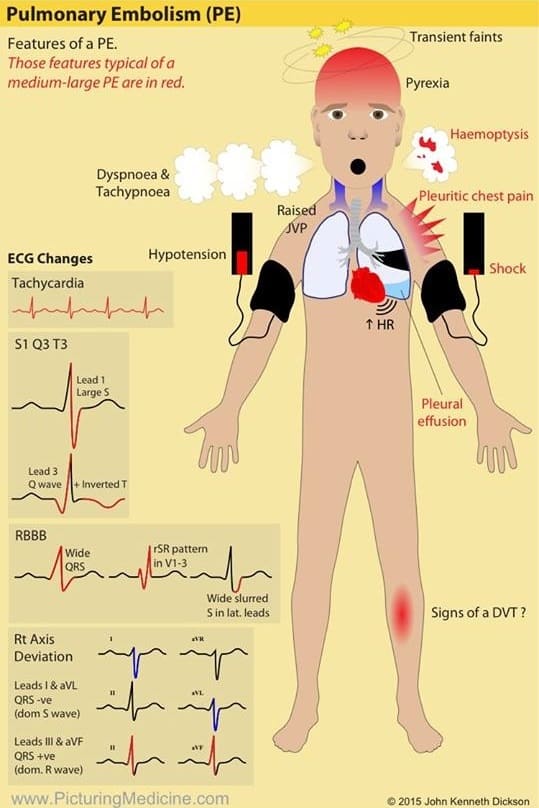
Symptoms and Signs of Pulmonary Thromboembolism
Symptoms
- Chest pain
- Dyspnea
- Syncope
- Symptoms of DVT
Signs
- tachycardia
- hypotension
- hypoxia
- tachypnea
- fever
- altered mental status
- signs of DVT (e.g., asymmetric extremity edema, or positive Homans sign)
One of the most life-threatening presentations of PE is massive PE. The American Heart Association (AHA), in its 2011 scientific statement, defined massive PE as:
- Acute PE with sustained hypotension (systolic blood pressure 90 mm Hg for at least 15 minutes or requiring inotropic support, not due to a cause other than PE, such as arrhythmia, hypovolemia, sepsis, or left ventricular [LV] dysfunction)
- Pulselessness, or
- Persistent profound bradycardia (heart rate < 40 beats per minute with signs or symptoms of shock).
Differential Diagnosis
The differential diagnosis for a patient presenting with symptoms of massive Pulmonary Thromboembolism includes:
- Acute coronary syndrome
- Cardiac tamponade
- Valvular dysfunction
- Acute pulmonary edema
- Pneumothorax
- Aortic dissection
Ultrasonographic Findings in Pulmonary Thromboembolism
When presented with a patient in whom these diagnoses are being considered, bedside transthoracic echocardiography is extremely useful. In this scenario, it may not be feasible to transport an unstable patient to have radiographic studies.
Ultrasonographic findings associated with massive PE include:
- Dilation of the right ventricular (RV) or inferior vena cava (IVC)
- RV dysfunction
- Septal flattening
- Pulmonary hypertension.
The clinician may also look for signs of DVT using lower extremity Doppler. Other findings such as cardiac tamponade, pneumothorax, and large pleural effusion may also be confirmed via bedside ultrasound, helping the provider key in on a diagnosis.
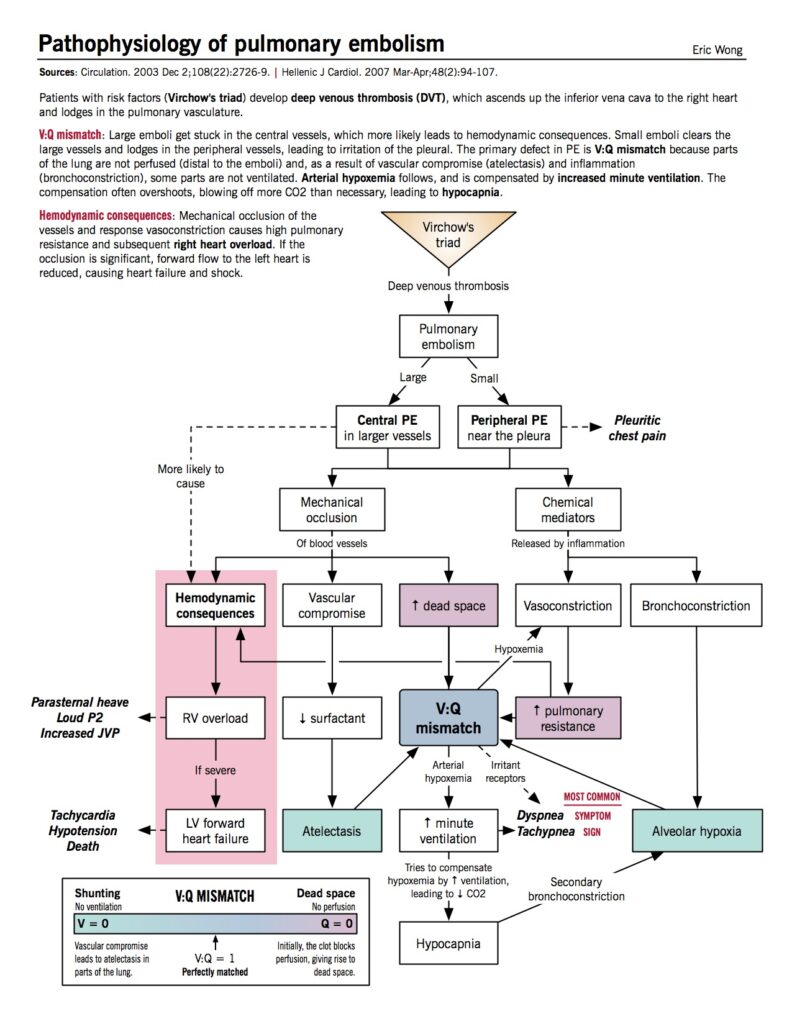
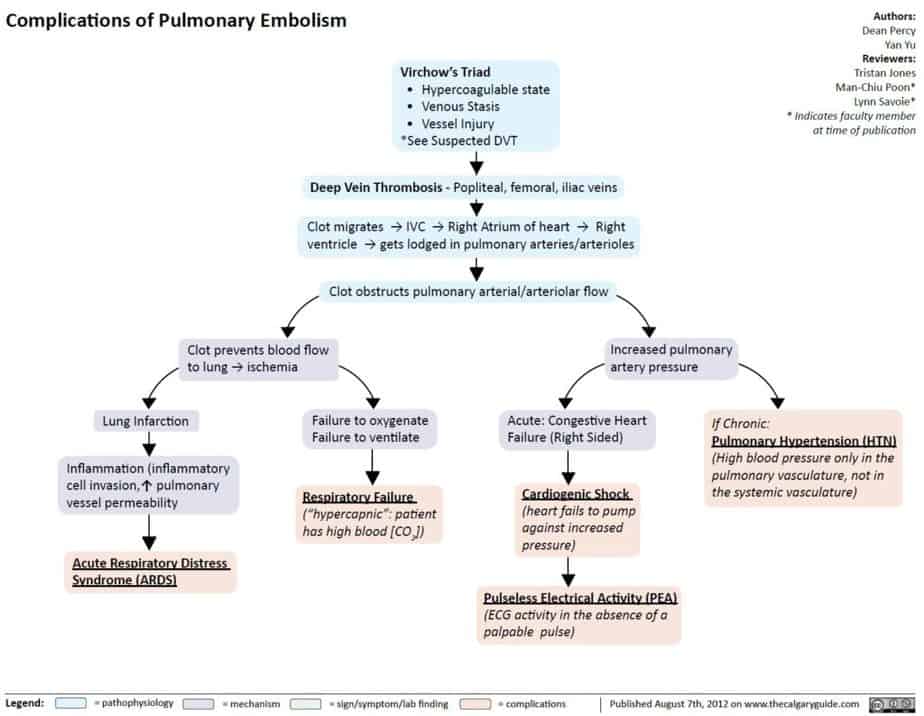
How does Pulmonary Thromboembolism compromise circulation and eventually lead to shock?
Acute PE interferes with the circulation in the pulmonary bed. If more than 30% to 50% of the total cross-sectional area of the pulmonary arterial bed is occluded by thromboemboli, the pulmonary artery pressure (PAP) increases.
Additionally, local hypoxia induces vasoconstriction in the vascular bed, leading to a further increase in the pulmonary vascular resistance. As such, the abrupt increase in pulmonary vascular resistance results in RV dilation, with resultant increase in RV pressure and volume.
The sudden increase in wall tension prevents the RV from overcoming the PAP, leading to leftward bowing of the interventricular septum. This impedes LV filling in early diastole, eventually reducing the cardiac output and contributing to hemodynamic instability and obstructive shock.
Treatment
Patients presenting with symptoms of massive PE must have their airway, breathing, and circulation immediately addressed. As massive PE causes obstructive shock, treatment is required to restore adequate circulation.
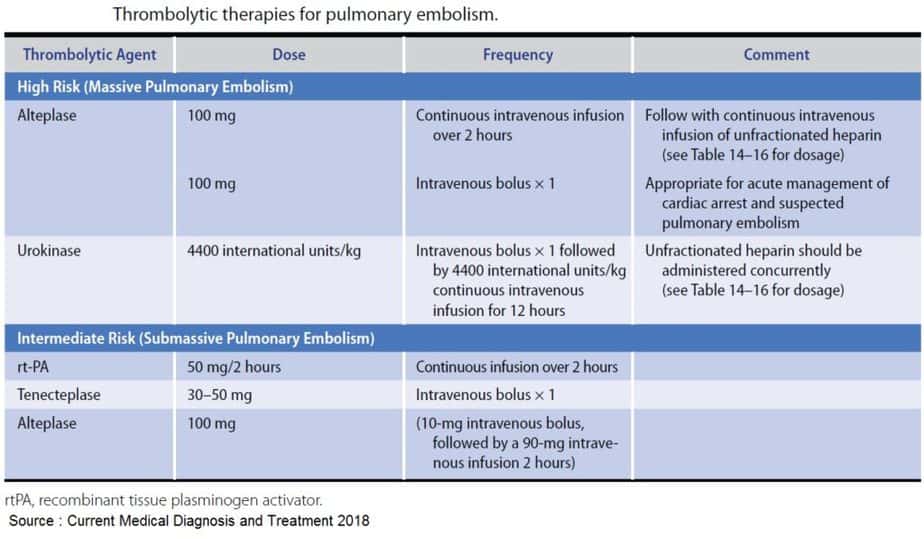
Per the AHA 2011 scientific statement, fibrinolysis is reasonable for patients with massive acute PE who have acceptable risks of bleeding complications (Class IIa; Level of Evidence B).
The data are derived from 13 main randomized controlled trials studying thrombolytics compared to placebo. Only a small subset included an investigation of massive PE, with primary outcomes being variable and conflicting in terms of trends toward improved survival and decrease in recurrent PEs.
The main positive outcomes observed with thrombolytics were stabilization of respiratory and cardiovascular function without vasopressor support, reduction of RV damage, and prevention of PE recurrence, with an increased probability of survival.
The main harms inflicted were major hemorrhage, including intracerebral hemorrhage, and increased risks of minor hemorrhages, resulting in prolonged length of stay and potential blood product administration.
The decision to administer a fibrinolytic agent depends on an individualized assessment of the risks and benefits. The optimal medical decision must incorporate patient wishes, life expectancy, and his/her risk of bleeding complications.
Once the decision to administer thrombolytic therapy has been made, the thrombolytic agent is typically administered via a peripheral intravenous catheter as an infusion.
The FDA-recommended infusion dose is for alteplase at 100 mg as a continuous infusion over 2 hours while withholding anticoagulation during the 2-hour infusion period. For this reason, when massive PE is suspected, anticoagulants with prolonged half-lives (such as low molecular weight heparin) should be avoided.
Anticoagulation is typically started after clot lysis with heparin and warfarin. The optimal duration of anticoagulation is based upon extrapolated evidence from patients with acute DVT in whom thrombolysis was not performed, which is a minimum of 3 months. Patients should be sent to an intensive care unit for further monitoring and treatment.
If patients survive this acute event, the main emphasis then turns to rehabilitation, anticoagulation compliance, and ultimate prevention of any predisposing factors for future VTE.
Although further clinical trials of the advanced therapies for VTE are needed, your decision must be based on the best available evidence. The administration of thrombolytics may lead improved morbidity and mortality and should be considered in the appropriate clinical scenario.
Key Points
- Clinical decision rules such as Wells’ criteria, Geneva score, and PERC (PE rule out criteria) are available to help determine pretest probability of VTE.
- Unexplained shock may be obstructive shock secondary to PE.
- Bedside ultrasound is a valuable tool when considering massive PE in a patient.
- Weigh risks and benefits when considering thrombolytic administration, paying special attention to bleeding risks.
- Emphasize compliance with anticoagulation after disposition.