Coagulopathy of liver disease leads to troubles as dramatic as large-volume hematemesis in a resuscitation bay or as indolent and irritating as a slowly oozing bleed around a central line on a boarded patient waiting for transfer out of the emergency department (ED).
By evaluating, anticipating, and correcting bleeding diatheses when appropriate, the emergency physician (EP) can help the patient achieve hemostasis and avoid these untoward outcomes.
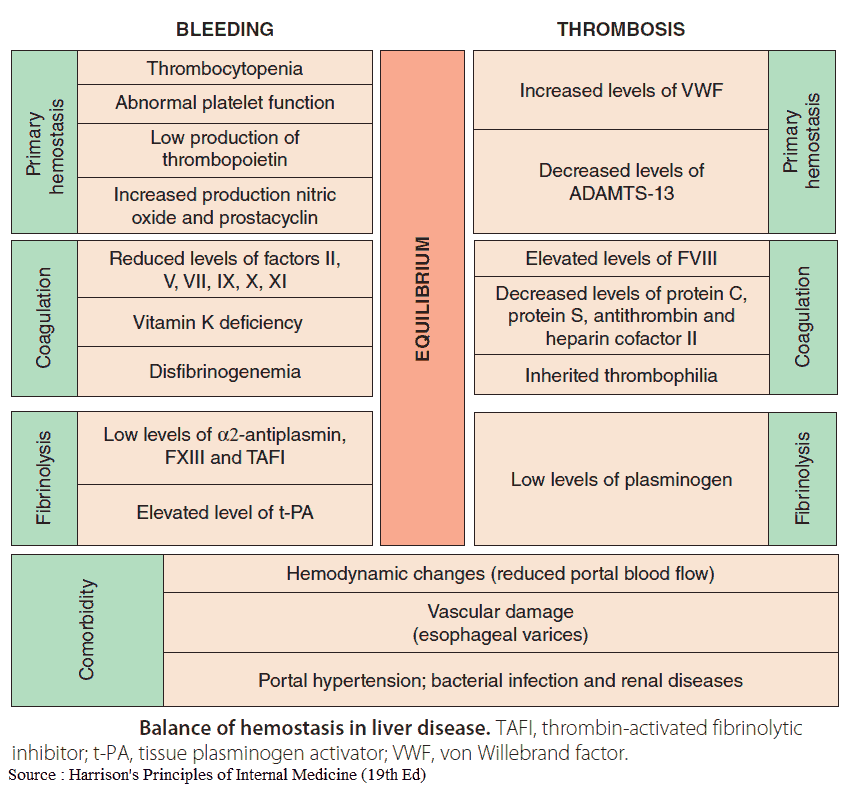
Blood clotting in the setting of chronic liver disease is complex and may result in a net prothrombotic or antithrombotic state.
Favoring bleeding (antithrombotic state) are:
- reductions in hepatically produced procoagulant factors (II, VII, IX, and X) and fibrinogen
- thrombocytopenia due to reduced thrombopoietin production, splenic sequestration, and production of antiplatelet antibodies
Favoring thromboses (prothrombotic state) are:
- reductions in a strong anticoagulant factor (protein C)
- increased platelet activation due to elevated von Willebrand factor levels
Complicating this situation is the lack of accurate lab assays to measure the net thrombotic state in liver disease patients. The international normalized ratio (INR) was validated as a standardized measure of anticoagulation for patients treated with Coumadin, but it is not calibrated to assess coagulopathy in liver disease patients.
Indeed, the risk of venous thromboembolism in hospitalized chronic liver disease patients is higher than for hospitalized patients without liver disease, indicating that a prothrombotic state is also frequently present.
Despite these issues, transfusion of blood products to correct these coagulation abnormalities is recommended when active bleeding is present.
Evaluation of Coagulopathy in Liver Failure
Fortunately for the goal-oriented provider, a small number of crucial laboratory tests are needed for rapid coagulopathy assessment in the ED.
Any patient with liver failure either actively bleeding or at risk of bleeding should have the following tests sent:
- prothrombin time/INR
- fibrinogen level
- platelet count.
A full battery of testing may help guide further evaluation and management down the road, but acute interventions will focus on these three tests.
Anticipating Need for Correction of Coagulopathy in Liver Failure
Patients with liver failure generally compensate for coagulopathy, and corrective medications or blood products should not be administered to patients without an active or anticipated source of bleeding, such as planned invasive procedures.
Acute correction is indicated for patients bleeding from gastrointestinal, traumatic, or iatrogenic sources.
Procedures with a high risk of harmful bleeding include:
- central lines
- lumbar punctures
- intracranial monitor placement
The urgency of these procedures must be weighed against the risk of waiting for correction of coagulopathy. Lower-risk procedures such as paracentesis and peripheral vascular access do not necessitate correction.
Appropriate Selection of Treatment of Coagulopathy in Liver Failure
Treating coagulopathy based on Fibrinogen level
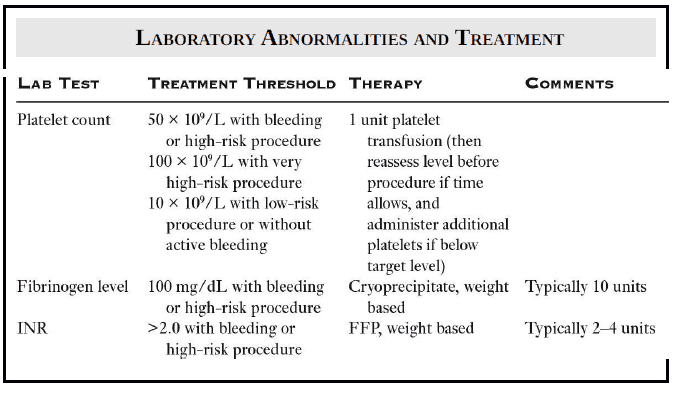
If the fibrinogen level is under 100 mg/dL and the patient warrants correction, cryoprecipitate should be given with weight-based dosing. This is typically around ten units.
Treating coagulopathy based on Platelet Count
- If the platelet count is <50 × 109/L during active or anticipated bleeding, 1 unit of platelets should be administered.
- Certain very high-risk procedures, such as ICP monitor placement, may warrant a higher platelet goal of >100 × 109/L.
- For patients without active or anticipated bleeding, platelet transfusion should be considered only for a platelet count of <10 × 109/L
Treating coagulopathy based on INR
Treating coagulopathy based on INR is more complicated, due to the multifactorial nature of delayed hemostasis and lack of consensus recommendations.
Fresh frozen plasma (FFP) is the frontline therapy for active or anticipated bleeding with INR over 2.0. Of note, the large volume of FFP required to treat coagulopathy may cause volume overload, which can worsen portal hypertension and bleeding due to gastroesophageal varices.
Recombinant factor 7 may be considered in the case of life-threatening bleeding, but outcome-based research remains limited and this agent is extremely expensive. The role for other agents, including prothrombin complex concentrates, is currently under investigation.
Although total vitamin K deficiency is not directly caused by chronic liver disease, it frequently accompanies the malnourishment that occurs with chronic alcohol abuse. Administration of parenteral (intravenous, intramuscular, or subcutaneous) vitamin K should therefore be considered in alcoholic patients with active bleeding when the INR is elevated, regardless of whether liver disease is present.
Summary
Coagulopathy in patients with liver failure is complex due to imbalances in both procoagulant and anticoagulant pathways. In the setting of active or anticipated bleeding, the EP should evaluate the PT/INR, fibrinogen, and platelet counts in these patients and prudently correct abnormalities based on the clinical scenario and the severity of bleeding or anticipated procedural risk.
Key Points
- If your patient has liver disease, anticipate both bleeding and clotting.
- Check PT/INR, fibrinogen levels, and platelet count in all patients at risk of bleeding.
- Correct coagulopathies judiciously and with appropriate therapy.
References / Suggested Readings
- Dasher K, Trotter JF. Intensive care unit management of liver-related coagulation disorders. Crit Care Clin. 2012;28:389–398.
- De Gasperi A, Corti A, Mazza E, et al. Acute liver failure: managing coagulopathy and the bleeding diathesis. Transplantation Proceedings. 2009;41:1256–1259.
- Munoz SJ, Stravitz RT, Gabriel DA. Coagulopathy of acute liver failure. Clin Liver Dis. 2009;13:95–107.
- Northup PG, Caldwell SH. Coagulation in liver disease: guide for the clinician. Clin Gastroenterol Hepatol. 2013;11:1064–1074.