Table of Contents
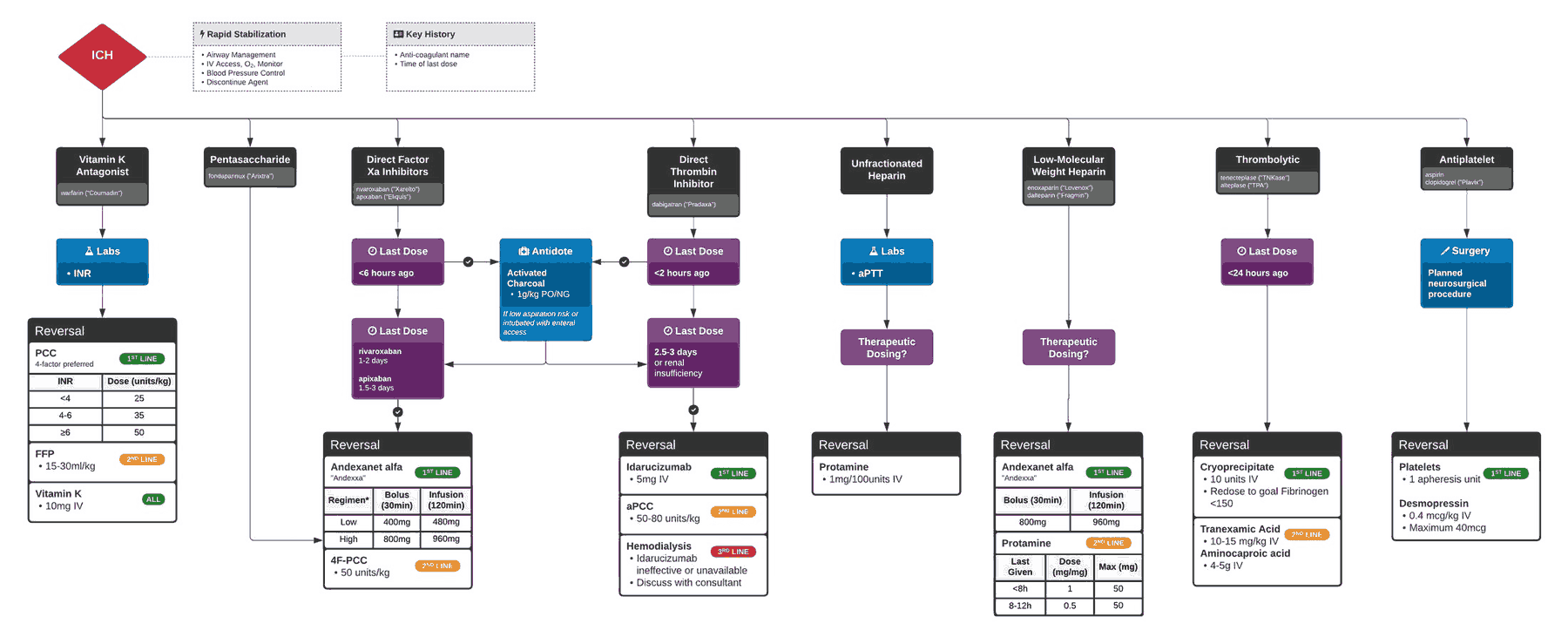
In the setting of life-threatening hemorrhage, the standard ABCs may be reconsidered as A2BC, with the additional “A” representing concomitant anticoagulant reversal. The anticoagulated patient with life-threatening hemorrhage does not allow time for nuanced discussions and thorough vetting of the evidence, as reversal is a time-sensitive action.
A classic scenario of life-threatening hemorrhage requiring emergent anticoagulant reversal is that of intracranial hemorrhage (ICH). We extrapolate recommendations for other hemorrhages from this often-studied patient group. The objectives of this article are to:
- Explore the rationale for rapid anticoagulant reversal in life threatening hemorrhage;
- Discuss the reversal of the most common anticoagulant: warfarin;
- Identify the newer Target Specific Oral Anticoagulants (TSOACs), proposed reversal strategies, and future reversal agents in development
- Provide a practical reference guide that can be utilized on one’s next shift.
Anticoagulants and Hemorrhage
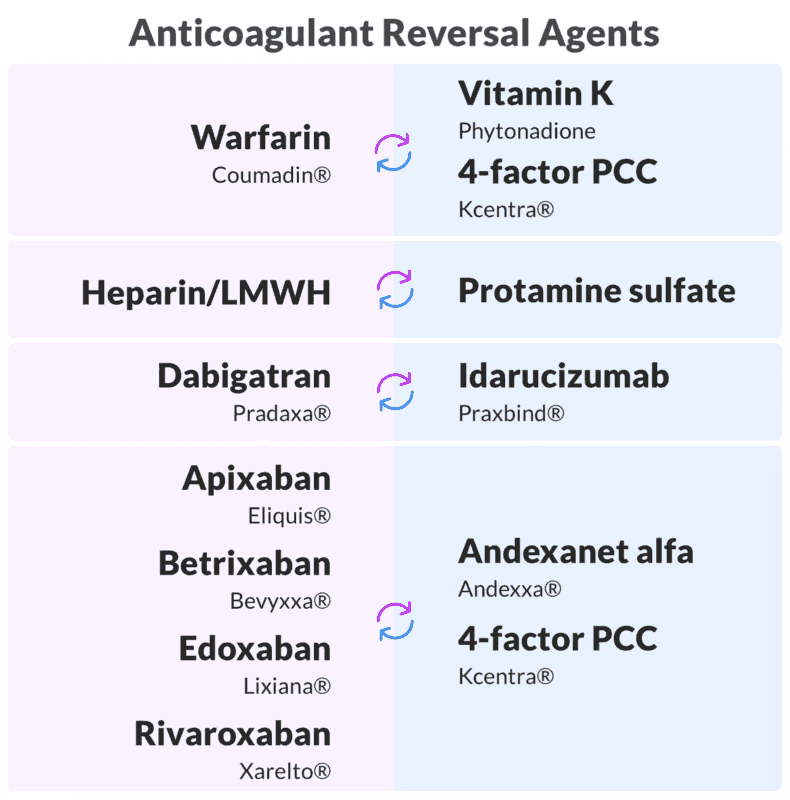
The most common oral anticoagulant is the vitamin K antagonist (VKA), warfarin. Increasing in popularity due to lack of required monitoring and greater anticoagulation reliability are the TSOACs, which include factor Xa inhibitors, and direct thrombin inhibitors (DTIs). Other common antithrombotic agents include antiplatelet agents.
While relative safety of all these agents has been demonstrated, a life-threatening emergency arises when these patients are bleeding, particularly in the setting of ICH. Typical ICH mortality is estimated at ~40%, increasing to ~60% when complicated by anticoagulation. Further neurologic morbidity increases with hematoma expansion, which worsens in the setting anticoagulation.
Warfarin Reversal
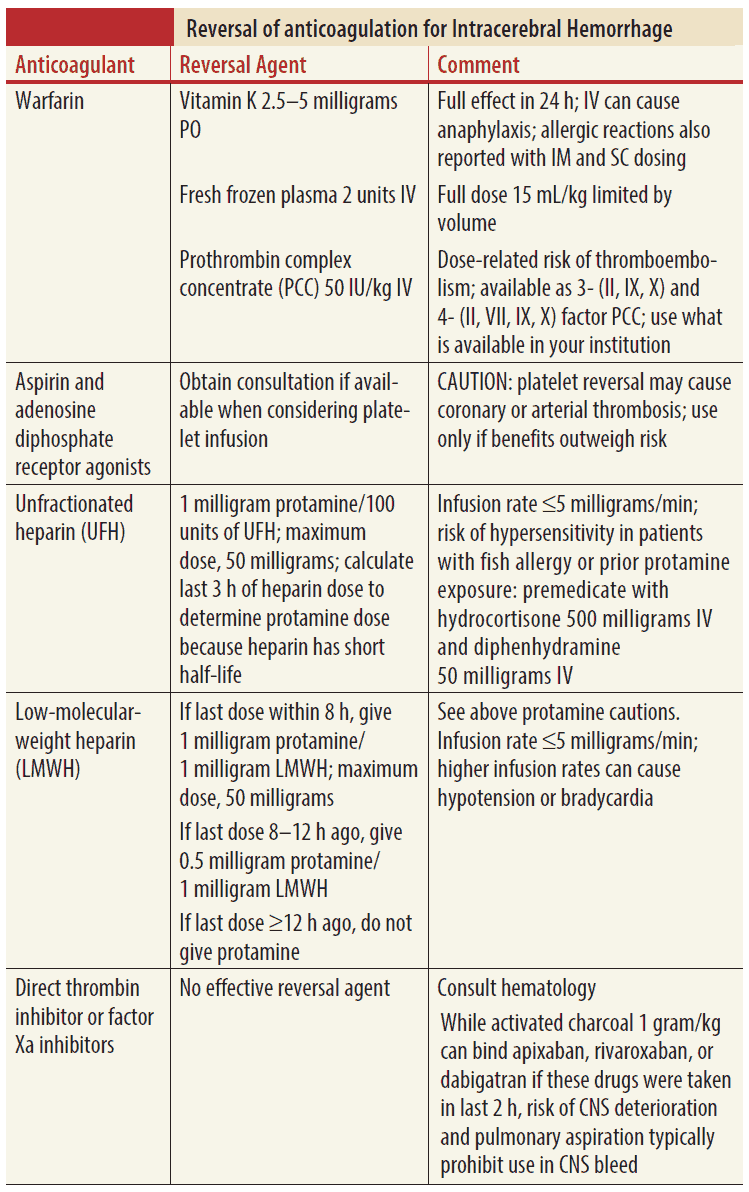
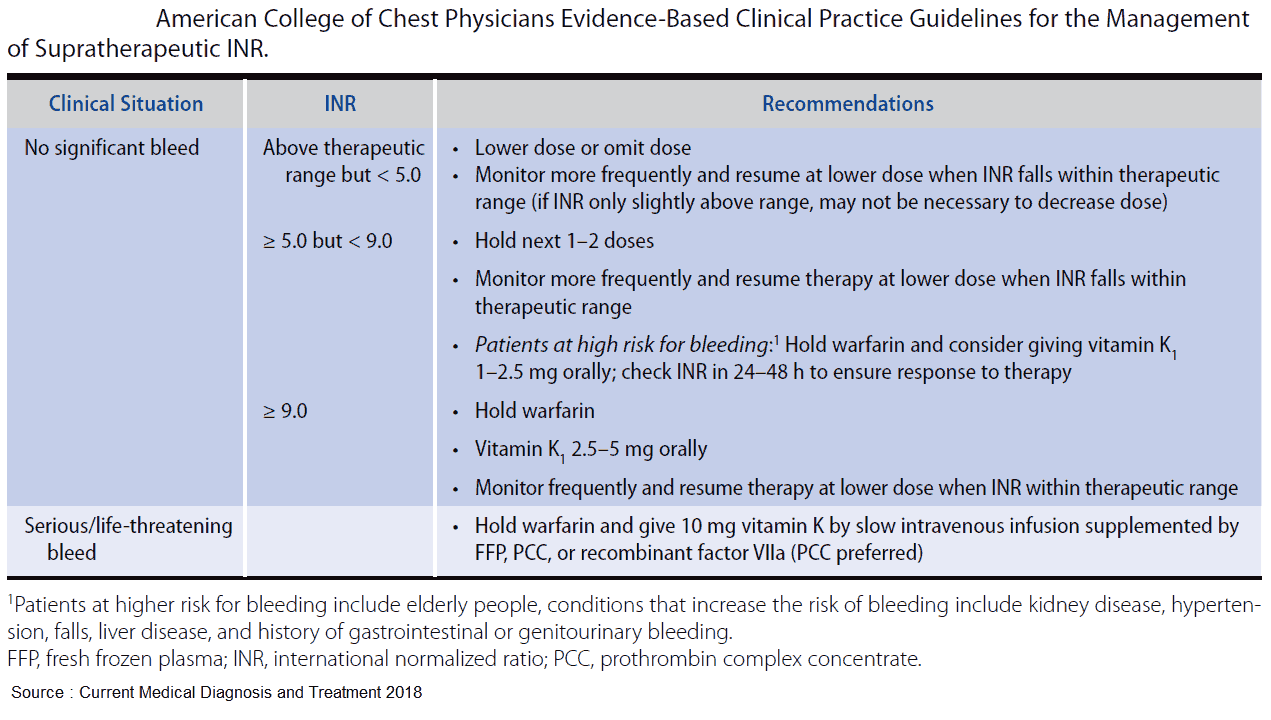
Reversing anticoagulants is informed by varying levels of evidence, with warfarin reversal being the most researched. Warfarin reversal can be achieved through various agents, each differing in time of onset and duration of action:
- Vitamin K
- Prothrombin complex concentrate (PCC)
- Fresh frozen plasma (FFP)
Intravenous vitamin K has an onset of action of 2 to 6 hours and requires up to 24 hours to achieve reversal on its own.
PCC is a concentrate of vitamin K–dependent factors II, VII, IX, and X, plus protein C and S as well as a small amount of heparin. Originally developed for hemophilia B treatment, PCC has been used in much of the developed world for emergent warfarin reversal due to rapid onset and reliable international normalized ratio (INR) correction.
A recent randomized trial of vitamin K + PCC versus vitamin K + FFP for VKA-associated hemorrhage, compared hemostatic efficacy, and INR correction. In this industry-sponsored noninferiority study, PCC reversal was more rapid and with fewer adverse effects, which were primarily plasma-related volume overload. Thrombotic complications did not differ between groups. This study led to FDA approval of PCC for urgent VKA reversal in the setting of major bleeding.
While there is a lack of mortality data, there are several reasons why PCC is the preferred agent over FFP. The major downside of a FFP reversal strategy is the delay to INR correction owing to the required thawing of FFP and the unpredictable INR normalization. Additional complications include transfusion-associated circulatory overload (TACO) from the colloid load and transfusion-associated lung injury (TRALI).
Thus, recent AHA recommendations for VKA-associated ICH include IV vitamin K plus PCC as potentially preferable over FFP.
Reversal of Target Specific Oral Anticoagulants
These agents can be placed into two categories based on their Mechanism of Action:
- Direct Thrombin Inhibitors (DTI)
- Factor Xa inhibitors
DTIs include:
- oral agent Dabigatran
- parenteral agents
- bivalirudin
- argatroban
- desirudin
Xa inhibitors in clinical use include:
- rivaroxaban
- apixaban
- edoxaban.
Until recently, no rigorous clinical evidence existed to guide reversal of the target-specific oral anticoagulants (TSOACs), and recommendations are based on studies targeting normalization of laboratory parameters not clinically used and expert opinion.
PCC may reverse these agents by activating thrombin on the platelet surface. DTIs may be cleared by hemodialysis, but this is often impractical in the emergency setting.
Antidotes are currently being developed, such as the newly FDA-accepted antibody fragment idarucizumab, which showed promise in a recent observational clinical trial for reversal of dabigatran.
Antiplatelet Agents Reversal
Concerning antiplatelet agents, consensus on reversal is less clear, but many experts assert that since these agents tend to increase bleeding, their action should similarly be reversed. While clinical trials are ongoing, recommended treatments include transfusion of functioning platelets and DDAVP (desmopressin), which induces the release of von Willebrand factor and factor VIII, augmenting hemostasis.
Key Points
- Rapid anticoagulant reversal is critical in life-threatening hemorrhage.
- A warfarin reversal strategy should include 10 mg IV vitamin K plus PCC or FFP (PCC preferable).
- TSOAC reversal currently includes PCC based on limited data, and antibody fragment antidotes are currently being developed.
- While controversial, antiplatelet agent reversal includes platelet transfusion plus DDAVP.

![Read more about the article All About Leukemia: From Diagnosis to Treatment [A Comprehensive Overview]](https://manualofmedicine.com/wp-content/uploads/2023/04/Classification-of-Leukemias-According-to-Cell-Type-and-Lineage-300x213.png)