Table of Contents
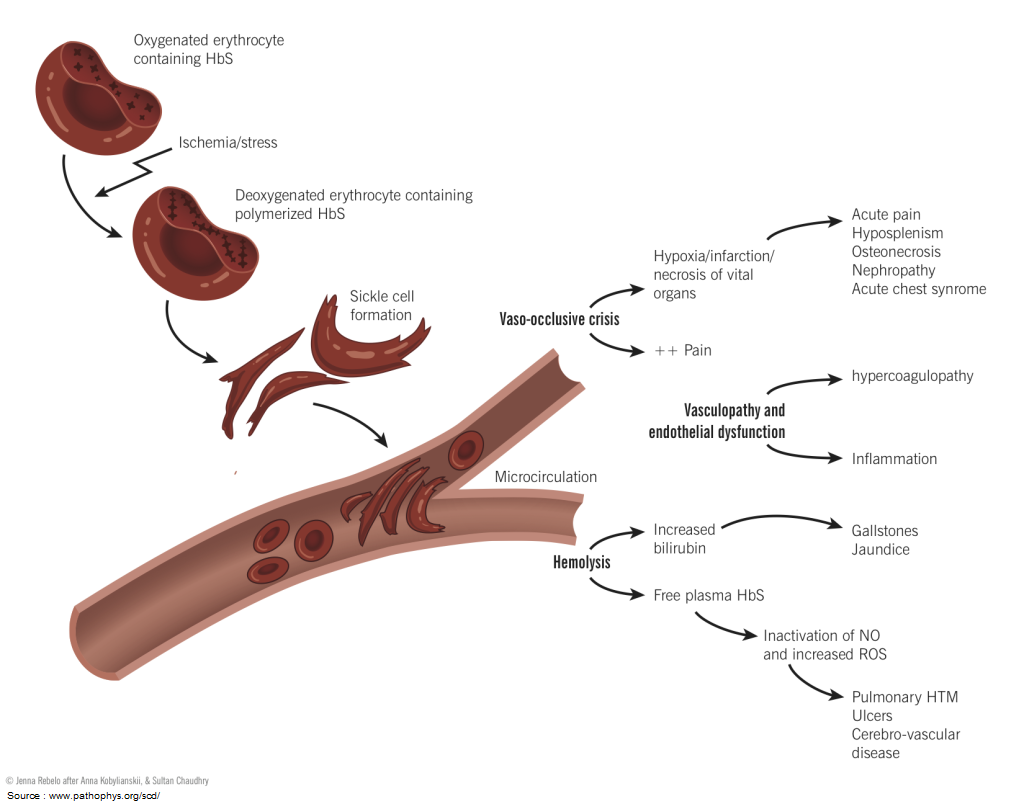
Pain in a patient with sickle cell disease (SCD) can be an indicator of lifethreatening pathology. The provider can be lured into diagnosing and treating pain as a vaso-occlusive episode (VOE) without assessing for signs of impending clinical deterioration.
A vaso-occlusive episode (VOE) is a diagnosis of exclusion; you must first rule out the emergent conditions associated with SCD by relying on a thorough history and physical exam.
This article is not a comprehensive article on sickle cell disease (SCD) but highlights the complications that could quickly turn a suspected vaso-occlusive episode (VOE) into a catastrophic emergency.
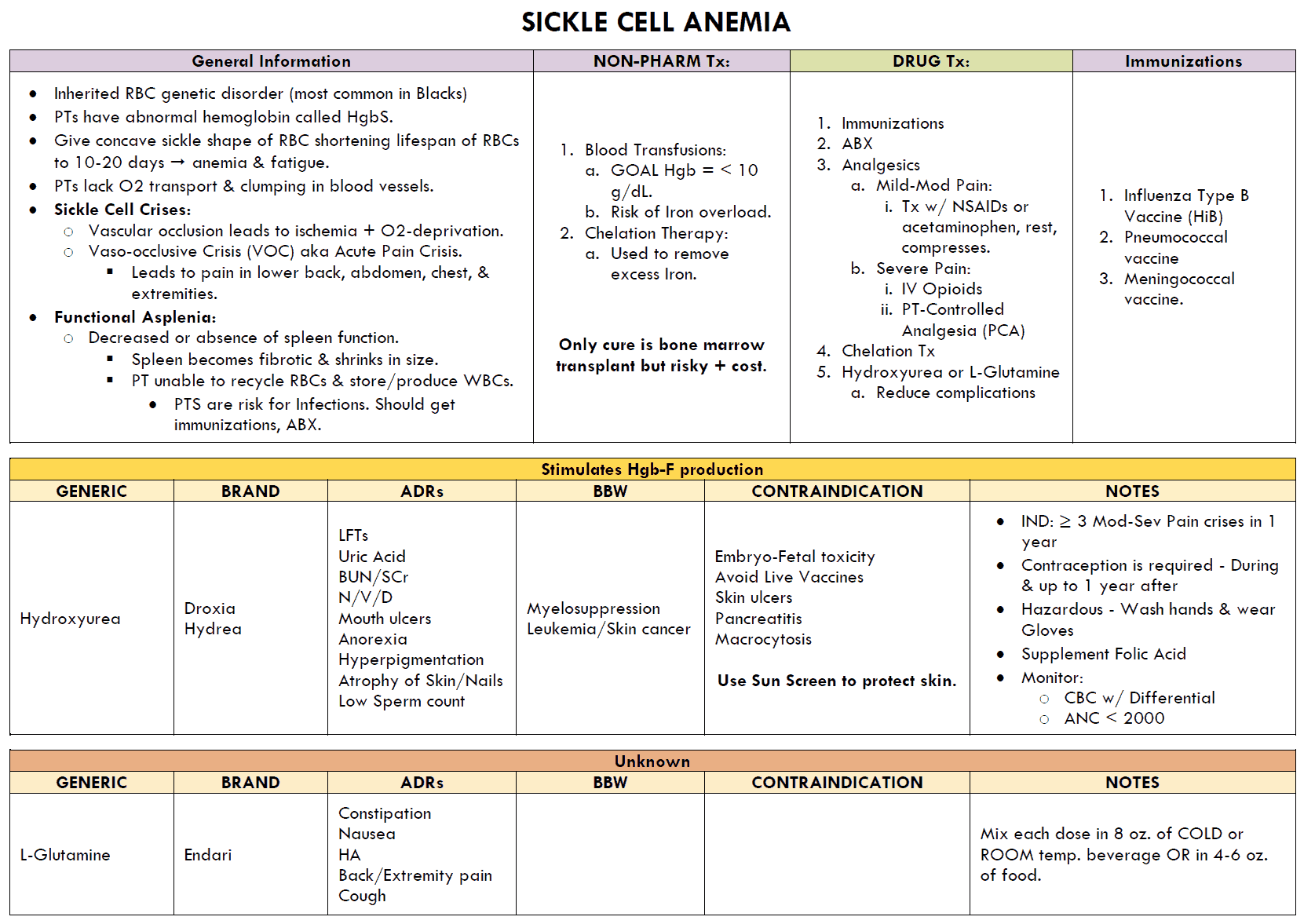
Acute Chest Syndrome
- Acute chest syndrome (ACS) is the leading cause of death in patients with sickle cell anemia.
- ACS should be on the differential for any SCD patient with chest pain.
- Be reluctant to attribute a patient’s tachypnea to pain.
- It is important to assess for ACS by acquiring a chest x-ray and performing a thorough physical exam; listen for rales (most common physical exam sign), decreased breath sounds, or wheezing. Fever and cough are common symptoms of ACS.
- Continuous pulse oximetry should be initiated upon arrival to the ED to assess and monitor for development of hypoxia due to ACS.
- When assessing chest pain in a patient with sickle cell anemia, keep your differential wide. These patients have a high risk for ACS, but that does not exclude them from common causes of chest pain seen in the general population such as acute myocardial infarction, pulmonary embolus, or pneumothorax.
- Rapid detection of ACS is important as early initiation of exchange transfusion and antibiotics can drastically improve outcomes.
Stroke
It is absolutely crucial to test for disability during the primary assessment of a patient in a pain episode. A VOE is not confined to the peripheral circulation; these patients are a high risk for stroke due to cell adhesion and inflammatory changes in cerebral vasculature. A thorough assessment of mental status and neurological deficit should be performed.
Stroke is not just an adult problem. Children with SCD between 2 and 9 years of age are at significant risk for stroke. Young children who are unable to comply with a neurologic exam, parents, or caregivers can be your best source of information regarding changes in neurologic status.
Splenic Sequestration
- A thorough physical exam can make a lifesaving difference. It is imperative to palpate for the patient’s spleen.
- Splenic sequestration is equivalent to major hemorrhage; these patients lose a significant amount of blood from their intravascular volume into their spleen.
- The spleen is a dangerously capable reservoir for blood; it can rapidly enlarge to several times its normal size due to pooling.
Children with SCD are more likely to develop splenic sequestration as most still have adequate blood flow to the spleen. This is less common in adults with SCD because they often have splenic atrophy or fibrosis due to infarcts earlier in life. Even with functional asplenia, adults are still at risk for hepatic sequestration.
The initial tachycardic response to hypovolemia can be falsely attributed to pain. More specific symptoms for acute splenic sequestration include:
- Hypotension
- Fatigue
- Abdominal distention
- Back pain refractory to pain medication.
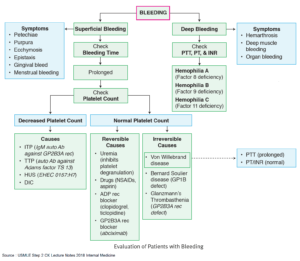
A CBC will show:
- Severe anemia
- Thrombocytopenia
- Elevated reticulocyte count.
If you see these symptoms or indications of poor perfusion, palpate for splenomegaly and hepatomegaly. If no spleen is palpable but suspicion is high, consider a bedside ultrasound or abdominal xray to assess for splenic or hepatic enlargement. Early detection allows for early transfusion and prevention of severe shock.
Infection
Infection is a common contributory factor to the RBC sickling that triggers a VOE. As mentioned above, numerous infarcts can leave a patient functionally asplenic early in life, impairing his or her defense against encapsulated bacteria.
It is crucial to determine if a VOE has been triggered by an infection. Scrutinize for signs of meningitis, osteomyelitis, and septic arthritis. In patients who present with fever or localizing signs of infection, obtain blood and urine cultures and chest x-ray, and then administer empiric antibiotics as soon as possible.
It is important to have a low threshold for an infectious workup when treating pediatric patients under age 5 years. Younger patients may have not received all of the vaccinations that help protect from common encapsulated organisms.
There are many other serious manifestations of SCD seen the in the ED:
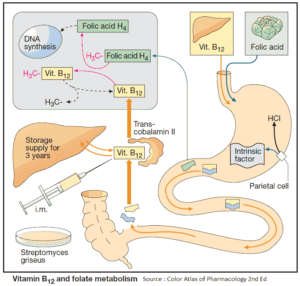
- Keep aplastic crisis on the differential if the patient has a low hemoglobin.
- Depressed hematopoiesis due to Parvovirus B19 can be life threatening to a patient with SCD.
- A patient who presents with extremity pain may be experiencing avascular necrosis, commonly mistaken for simple VOE.
- Lastly, young children are at risk of dactylitis caused by vaso-occlusion in the digits.
In all of these complications of SCD, early involvement of a hematologist in the treatment plan is important for patient outcome and transition of care from the emergency department
Key Points
- VOE is a diagnosis of exclusion; keep a wide differential for causes of pain in a patient with SCD.
- Initiate continuous pulse oximetry, and obtain CXR early if suspicious of ACS.
- Patients with SCD are at high risk for stroke; always assess for neurologic disability.
- Hypotension, abdominal distention, and back pain refractory to pain medication are signs of acute splenic sequestration.