Table of Contents
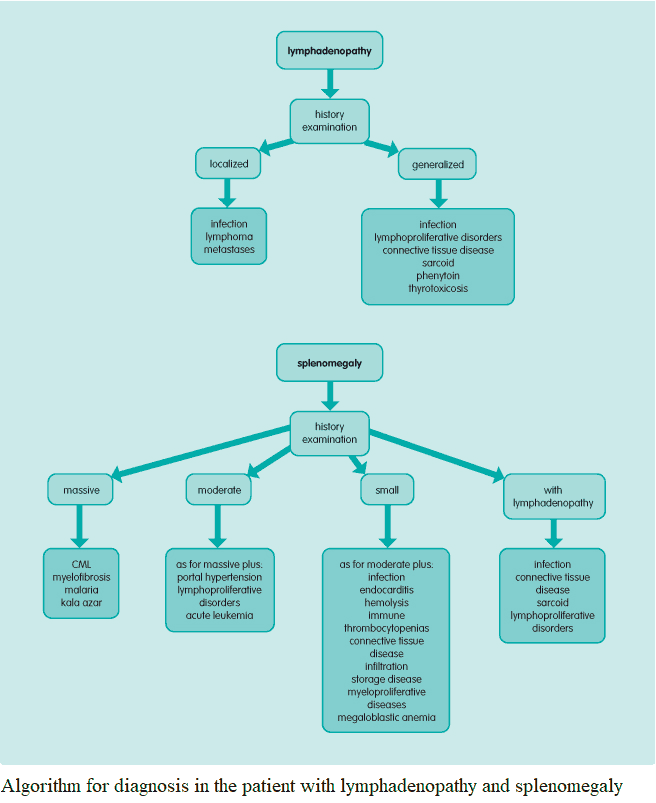
Splenomegaly is often a focus of short case examinations since many of its causes are chronic. Lymphadenopathy may be localized or generalized.
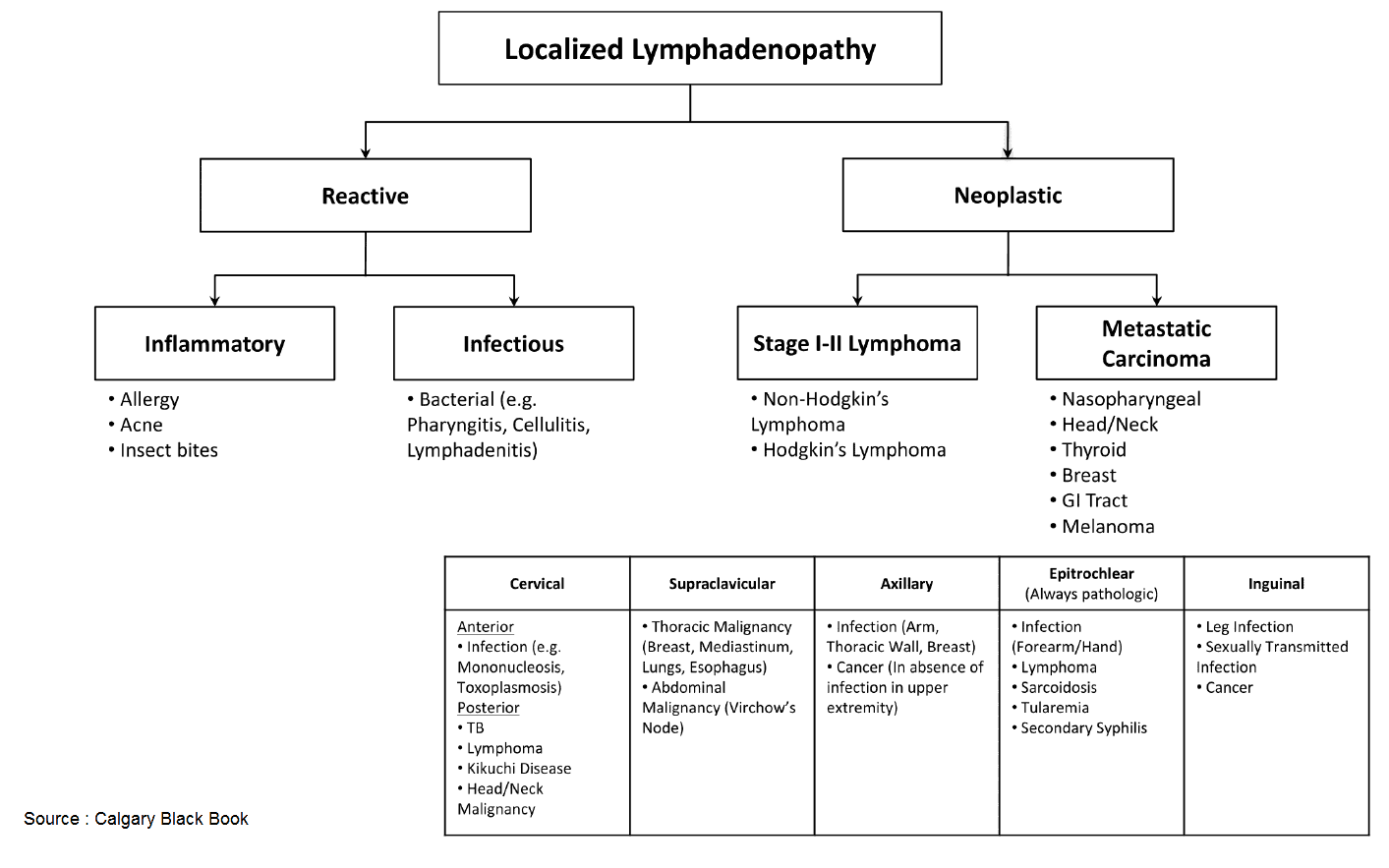
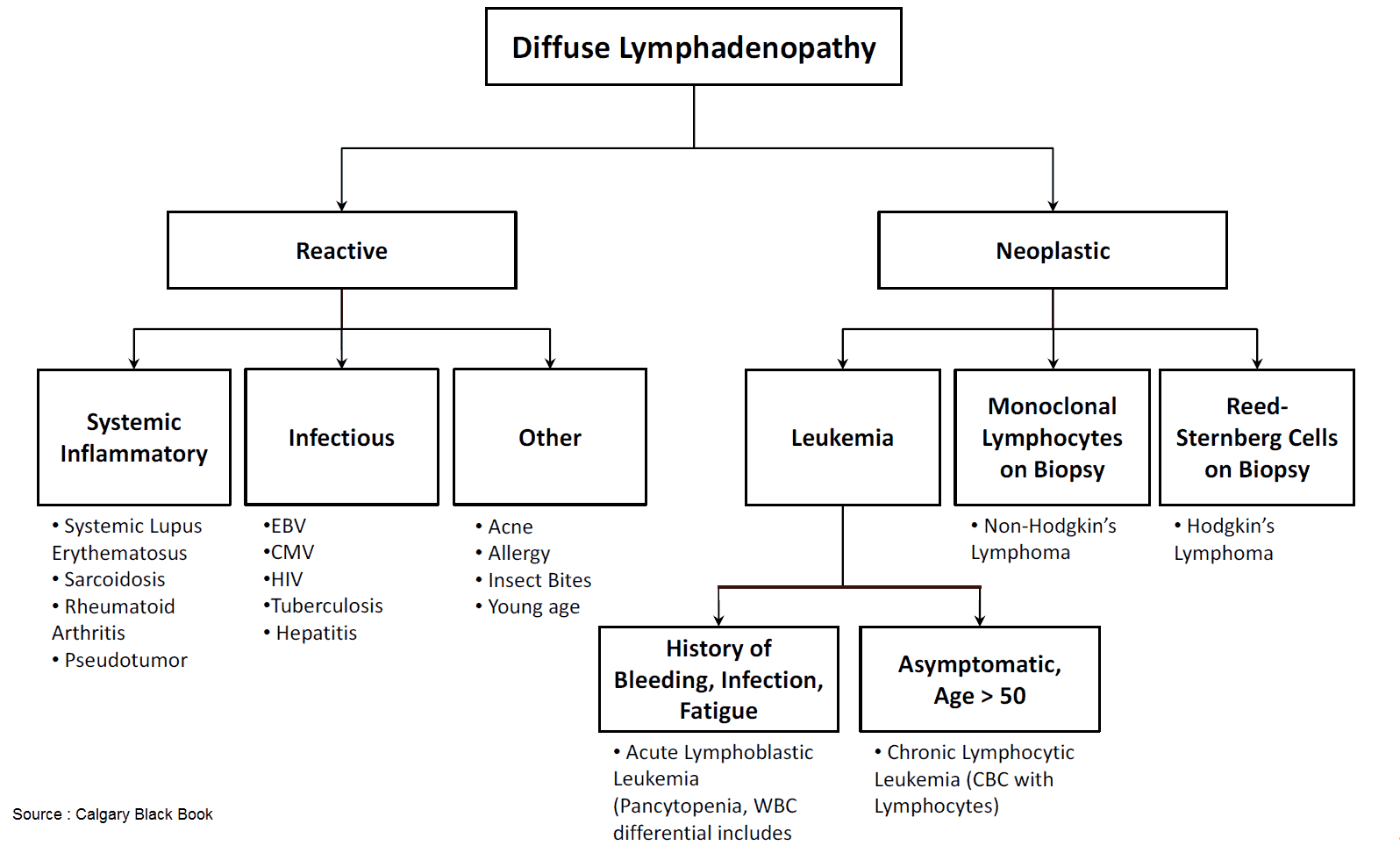
Causes and Differential Diagnosis of Lymphadenopathy
Localized lymphadenopathy
Consider which structures have lymphatic drainage to the nodes affected and examine these carefully for the following:
- Local infection: bacterial (e.g., otitis media, tuberculosis) or viral.
- Metastases: local malignancy.
- Lymphoma: Hodgkin’s disease or non-Hodgkin’s lymphoma.
Generalized lymphadenopathy
- Infection: particularly viral (Epstein-Barr virus [EBV], cytomegalovirus [CMV], human immunodeficiency virus [HIV], rubella), but also bacterial (tuberculosis [TB], syphilis, brucellosis) and protozoal (toxoplasmosis).
- Lymphoproliferative: Hodgkin’s disease or non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, acute lymphoblastic leukemia.
- Connective tissue disorders: systemic lupus erythematosus, rheumatoid arthritis.
- Infiltration: sarcoidosis.
- Drugs: phenytoin (“pseudolymphoma”).
- Endocrine: thyrotoxicosis (rare).
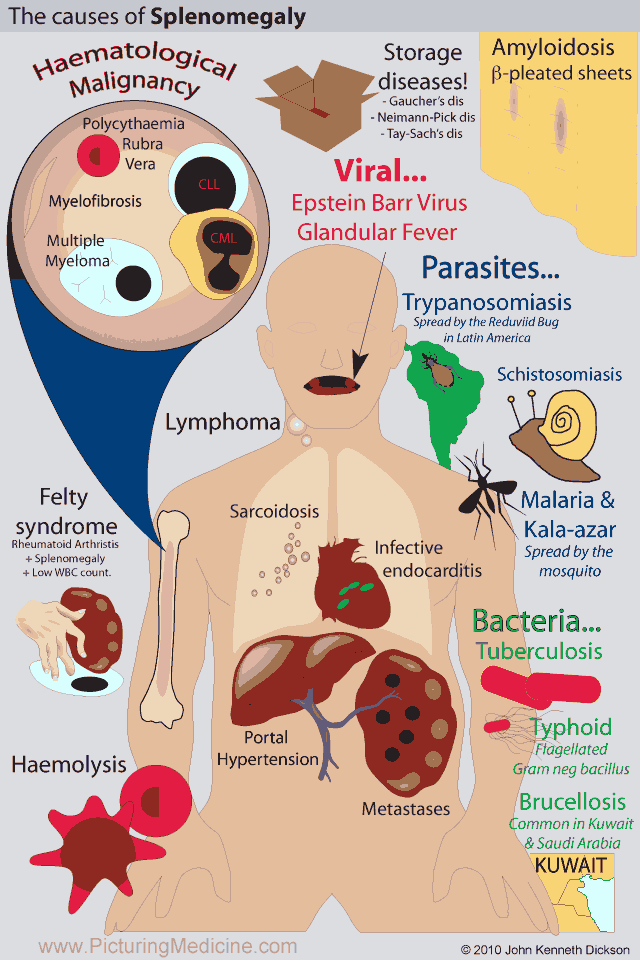
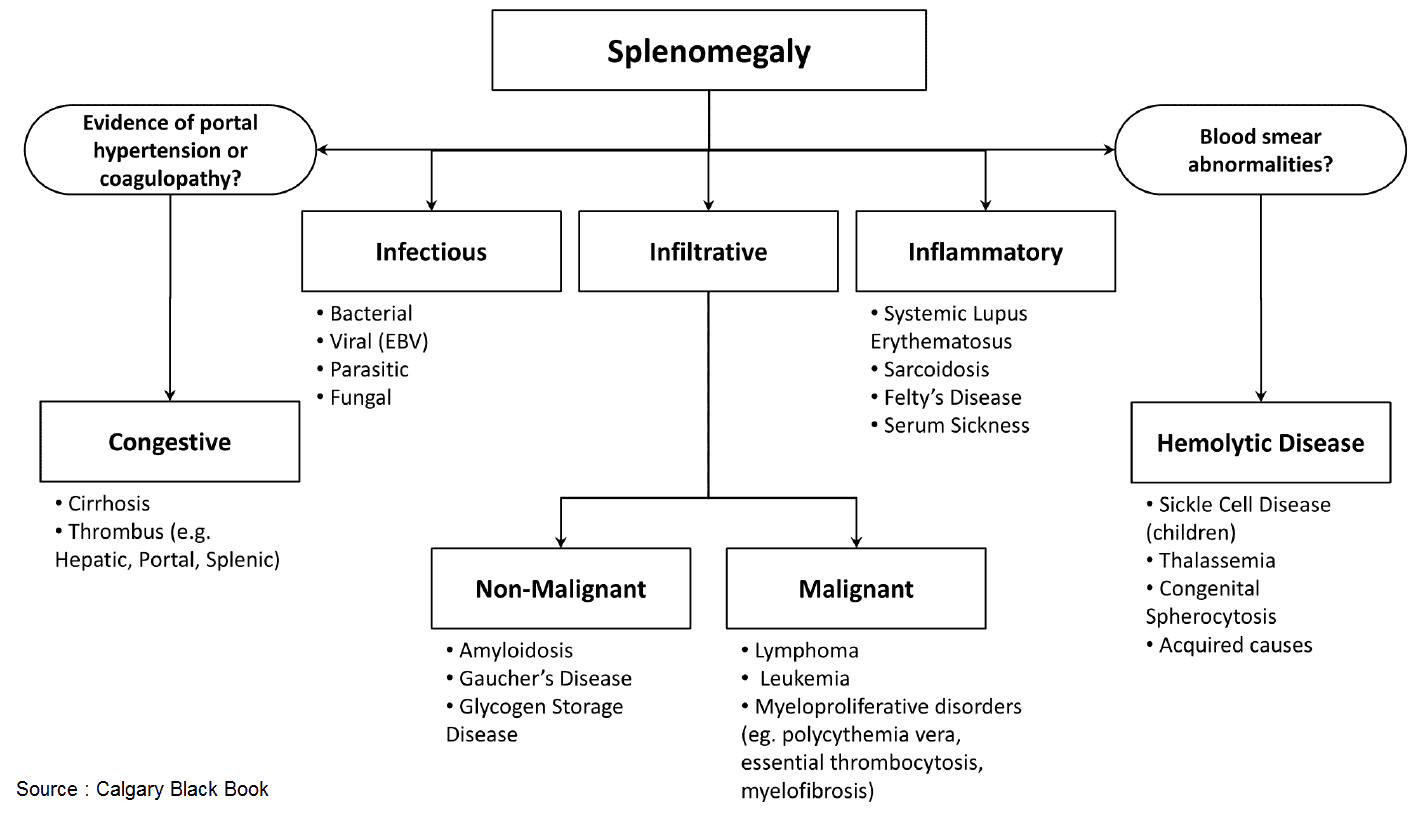
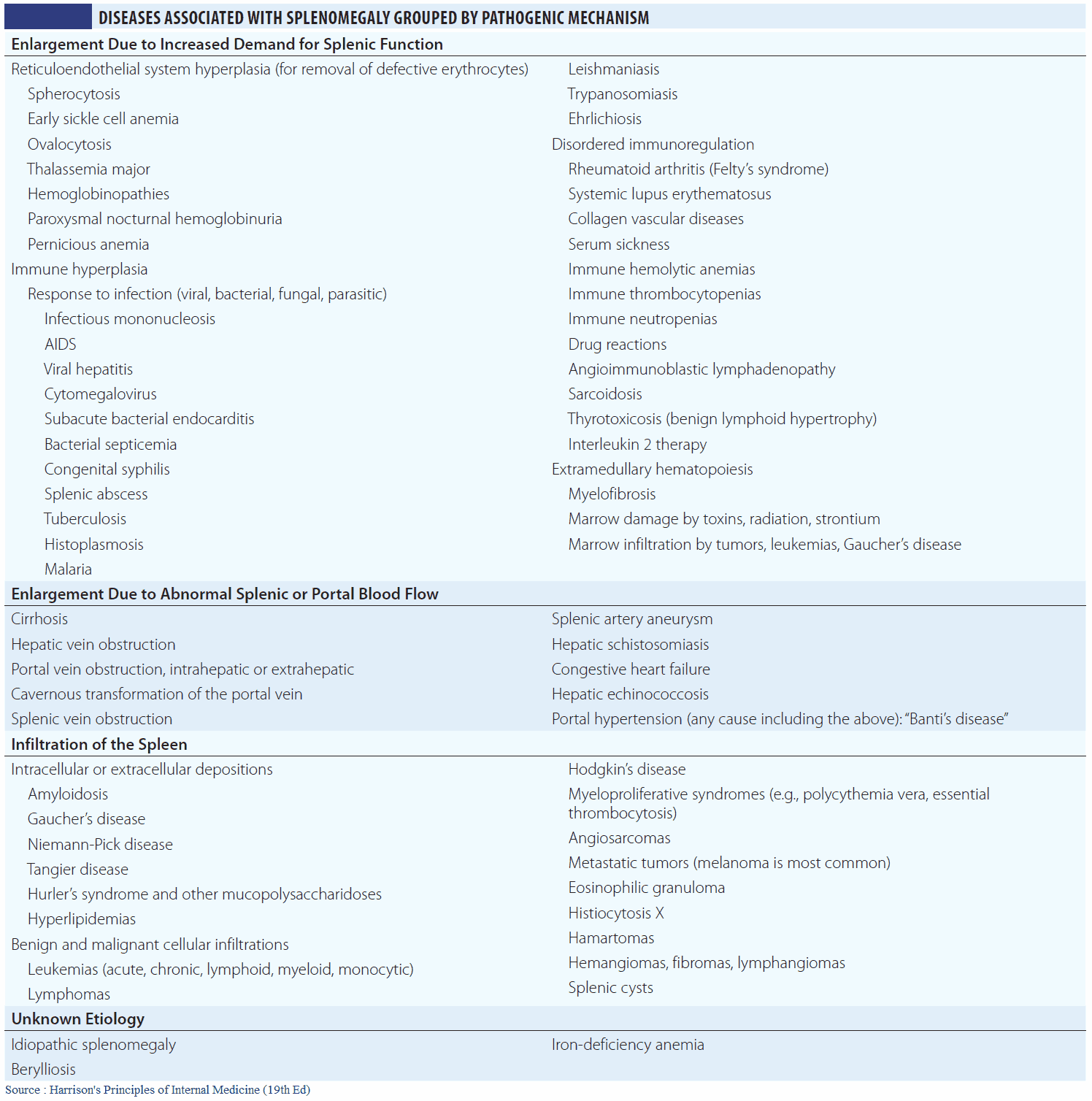
Causes and Differential Diagnosis of Splenomegaly
In general, different diseases cause different degrees of splenomegaly, as follows.
Massive splenomegaly is caused by:
- Chronic myeloid leukemia.
- Myelofibrosis.
- Malaria: rarely.
- Kala azar (leishmaniasis, caused by a parasite transmitted by the sand fly): rarely.
Moderate splenomegaly is caused by all of the above plus:
- Portal hypertension.
- Lymphoproliferative disorders (see above).
- Acute leukemias.
Just palpable splenomegaly is caused by all of the above plus:
- Infection: infectious mononucleosis, infectious hepatitis, subacute bacterial endocardititis, TB, brucellosis, schistosomiasis.
- Hemolytic anemias.
- Immune thrombocytopenias.
- Connective tissue disease: SLE, rheumatoid arthritis.
- Infiltration: amyloid, sarcoid.
- Storage disorders: Gaucher’s disease.
- Myeloproliferative disorders: polycythemia rubra vera, essential thrombocythemia.
- Megaloblastic anemias.
Symptoms and History in the Patient with Lymphadenopathy or Splenomegaly
It is often not possible to make a diagnosis on the basis of the history in these patients. However, important clues in the history can help to focus the clinical examination and further investigations.
Symptoms and History in Localized lymphadenopathy
Rate of node enlargement
Lymphadenopathy associated with infection often develops quickly and may be painful. When due to lymphoma or malignancy, the rate of enlargement tends to be slower and can wax and wane in the case of lymphoma. Sometimes the lymphadenopathy will not be noticed until it becomes large and causes disfigurement or rubs against clothes.
Lymphadenopathy may also result in lymphedema. This is a nonpitting edema caused by blockage of the lymph channels. Lymphedema may be the presenting sign of lymphadenopathy as the increasing size of the lymph nodes cuts off flow of regional lymph channels.
Symptoms in local structures
Has the patient noticed pain, erythema, or a mass in any of the structures draining into the affected node (e.g., cellulitis in inguinal lymphadenopathy or a breast mass in axillary lymphadenopathy)?
Systemic symptoms
In lymphoma the patient may experience “B symptoms” (fever, night sweats, weight loss), which indicate a poorer prognosis.
Symptoms and History in Generalized lymphadenopathy
A full systemic inquiry is essential in these patients as most of the causes of generalized lymphadenopathy can affect multiple systems. Special attention should be paid to the following:
- Malaise, anorexia and general debility: common but nonspecific.
- “B symptoms”: hematologic malignancy.
- Ask about tender lymph nodes after consumption of alcohol (can be seen in Hodgkin’s disease).
- Skin rash: rubella, SLE, and sarcoidosis.
- Arthragia and arthropathy: SLE, rheumatoid arthritis, syphilis (Charcot’s joints).
- Infectious contacts: rubella, TB, and EBV.
- Risk factors for HIV infection
- Drug history: to exclude phenytoin or beryllium as a cause. Also ask about any history of IV drug use.
- Symptoms of thyrotoxicosis: heat intolerance, weight loss, increased appetite, diarrhea, irritability.
Symptoms and History in Splenomegaly
Previous medical history
Is the patient known to have a pre-existing illness that can cause splenomegaly, such as chronic liver disease resulting in portal hypertension, connective tissue disease, thalassemia (hemolysis), Gaucher’s disease, or damaged cardiac valves (rheumatic fever or prosthetic valve) with subacute bacterial endocarditis?
Recent travel abroad or infectious contacts
Consider infectious mononucleosis, TB, schistosomiasis, and malaria.
Systemic symptoms
Systemic symptoms suggestive of an underlying cause include arthralgia, rash, and “B symptoms” (as above).
Symptoms of hematologic disturbance
- Anemia may be present due to marrow infiltration, chronic disease, hemolysis, vitamin deficiency, or hypersplenism.
- Leukopenia causing recurrent infections may result from marrow infiltration, hypersplenism, or infection.
- Thrombocytopenia may be due to immune platelet destruction, marrow infiltration, or hypersplenism.
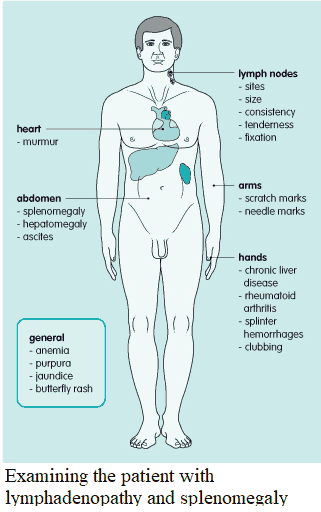
Examination and Signs in the Patient with Lymphadenopathy and Splenomegaly
When lymphadenopathy or splenomegaly is present, a full clinical examination of the lymphatic system should be made. The examination should then focus on possible underlying causes
Which lymph nodes are affected?
Firstly, the extent, sites, sizes, consistency, tenderness, and fixation of enlarged lymph nodes should be documented. Cervical, occipital, supraclavicular, axillary, and inguinal areas should be palpated carefully.
- Normal reactive nodes are generally less than 1 cm in diameter, feel soft, are not fixed, and can be tender.
- Lymphomatous nodes are often larger and feel rubbery but are not fixed.
- Lymph nodes infiltrated by carcinoma feel hard and may be fixed to surrounding tissue.
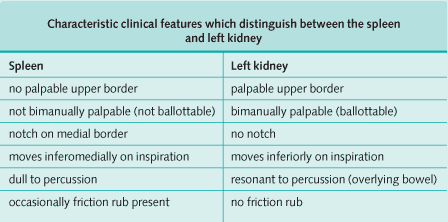
Is there splenomegaly?
If splenomegaly is present, the size (in cm) from the left costal margin must be recorded. It is important to distinguish the left kidney from the spleen when palpating a mass in the left hypochondrium and the differences between the two are commonly asked for in examinations (see Image bellow). A palpable spleen is at least twice its normal size.
Is there evidence of an underlying cause?
- Anemia and purpura may be present as described above.
- Jaundice may result from chronic liver disease, hemolysis, or infective hepatitis.
- Cachexia heralds underlying malignancy.
- Needle marks may indicate previous exposure to HIV and hepatitis B or C or provide a source of bacteria in infective endocarditis.
Localized lymphadenopathy
Examine those structures with lymphatic drainage to the affected nodes. Erythema, increased temperature, and tenderness suggest infection, while a hard, nontender mass may indicate malignancy. When there is isolated cervical lymphadenopathy, a formal ear, nose, and throat examination should also be performed since oropharyngeal malignancies commonly metastasize to these nodes.
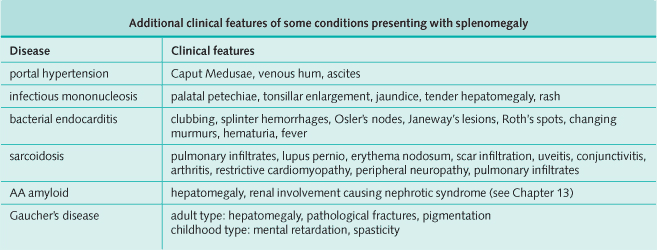
Splenomegaly and generalized lymphadenopathy
Where there is both splenomegaly and generalized lymphadenopathy consider lymphoproliferative disorders, infection, connective tissue disease, and sarcoidosis.
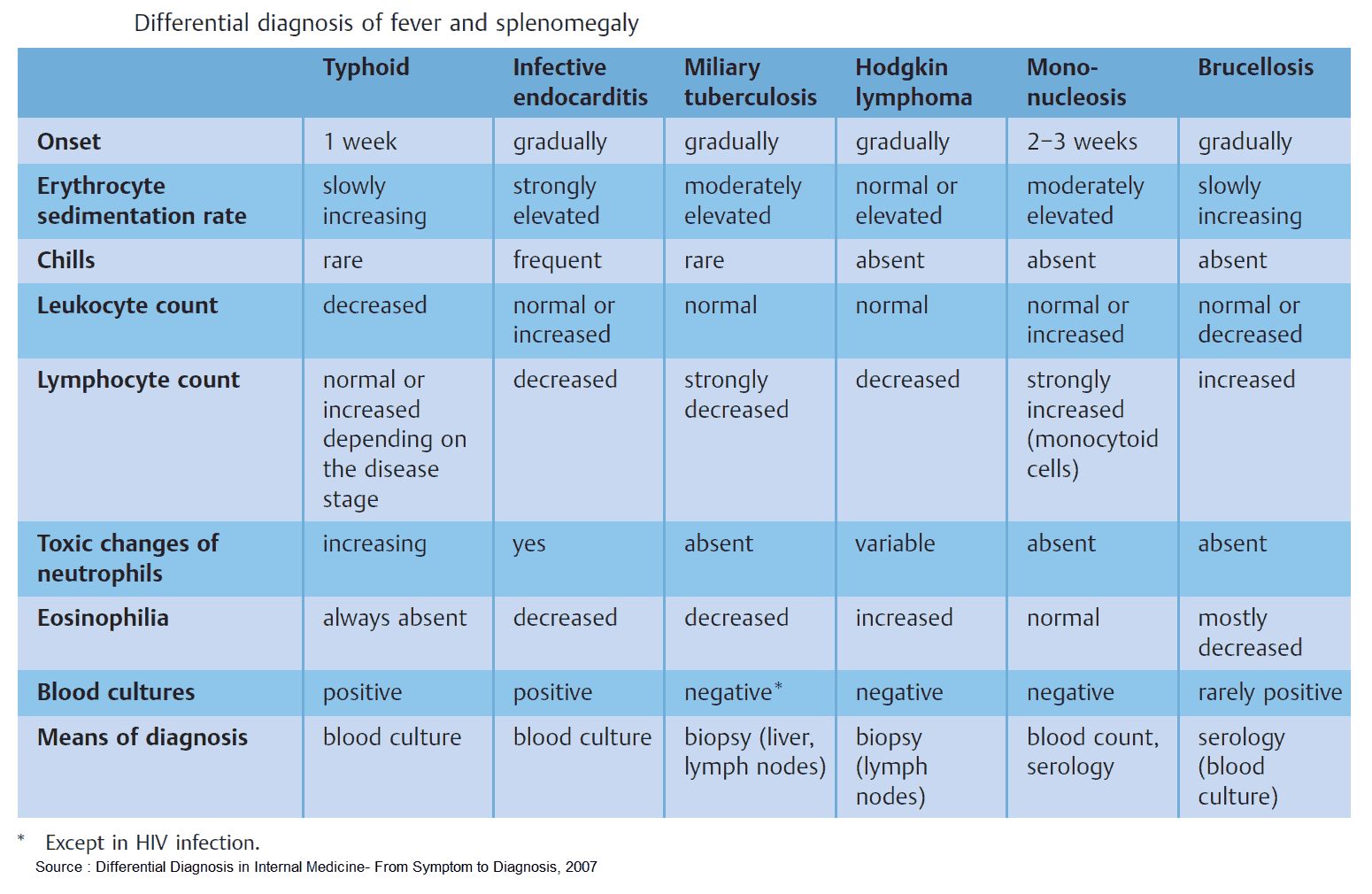
Investigating and Diagnosing the Patient with Lymphadenopathy and Splenomegaly
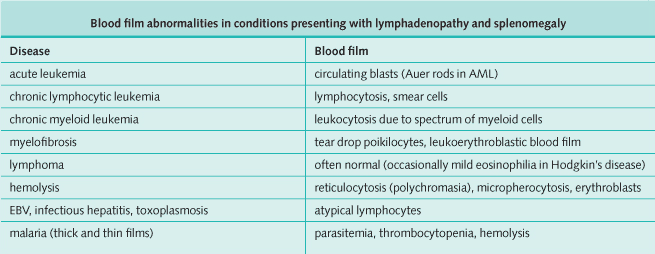
Hematology
- A complete blood count may show anemia, leucopenia, thrombocytopenia, or a combination of these.
- Blood film can provide diagnostic information (see Image bellow).
- Erythrocyte sedimentation rate will be elevated in infection, malignancy, and inflammation.
- Bone marrow examination includes aspiration, trephine, and cytogenetic analysis. It is indicated if the blood count or film suggest hematological abnormalities, and it is useful in the diagnosis of leukemias, myeloproliferative disorders, immune thrombocytopenias, and pancytopenia. Occasionally it is helpful in storage diseases, lymphoma, and carcinoma, where there is marrow infiltration.
Biochemistry
- Liver function tests:
- transaminases will be abnormal in infective hepatitis and sometimes in EBV and CMV;
- elevation in alkaline phosphatase and γ-glutamyl transpeptidase will occur when the porta hepatis is obstructed by enlarged lymph nodes;
- unconjugated hyperbilirubinemia will be present in hemolysis;
- an elevated lactate dehydrogenase indicates a poor prognosis in lymphoma.
- Serum calcium: raised in malignancy, sarcoidosis, and sometimes lymphoma.
- Serum uric acid: raised when there is rapid cell turnover such as in malignancy.
- Thyroid function tests: thyrotoxicosis.
Infection screen
- Monospot test: EBV.
- Serology: EBV, CMV, HIV, rubella, hepatitis, toxoplasmosis, and brucellosis.
- Blood cultures: repeated if infective endocarditis is suspected.
- Sputum culture: TB.
Autoantibody screen
This is useful in the detection of connective tissue disord.
Imaging
- Chest x-ray: bilateral hilar lymphadenopathy (caused by lymphoma, sarcoidosis, and TB).
- Abdominal ultrasound scan: will confirm the presence of splenomegaly.
- Computed tomography scan of the chest, abdomen, and pelvis: gives clear staging information in malignancy and particularly lymphoma where retroperitoneal lymphadenopathy may often be missed by ultrasound scan.
- MRI can evaluate intra-abdominal lymph nodes, look for a primary malignancy, and determine whether masses are cystic.

![Read more about the article All About Leukemia: From Diagnosis to Treatment [A Comprehensive Overview]](https://manualofmedicine.com/wp-content/uploads/2023/04/Classification-of-Leukemias-According-to-Cell-Type-and-Lineage-300x213.png)