Table of Contents
Chest pain is a common cause for admission to hospital. Taking a clear history is essential in making the correct diagnosis. Different diseases present with different types of chest pain.
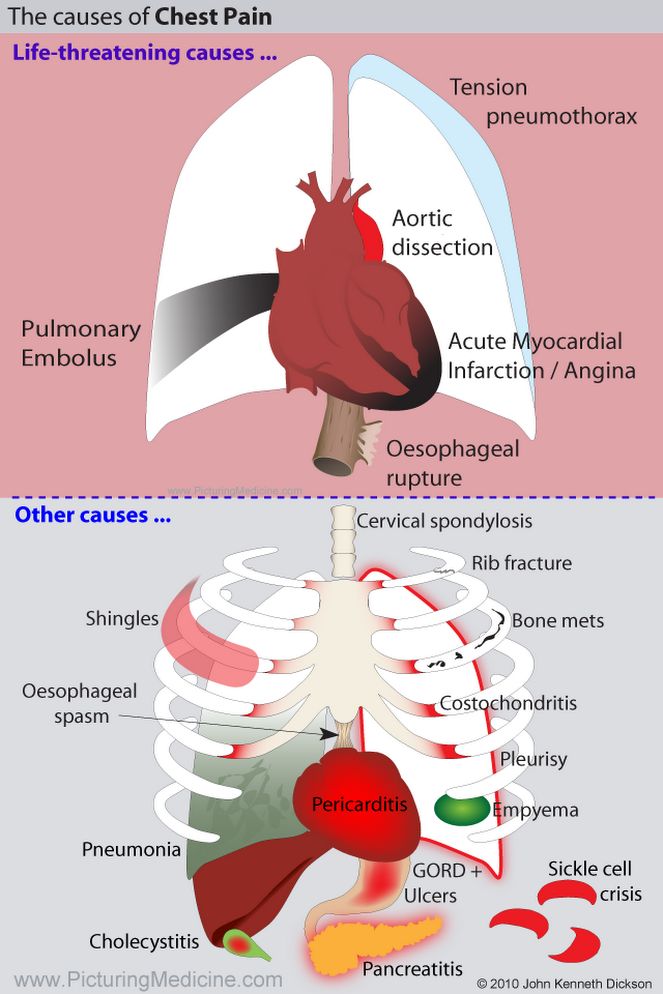
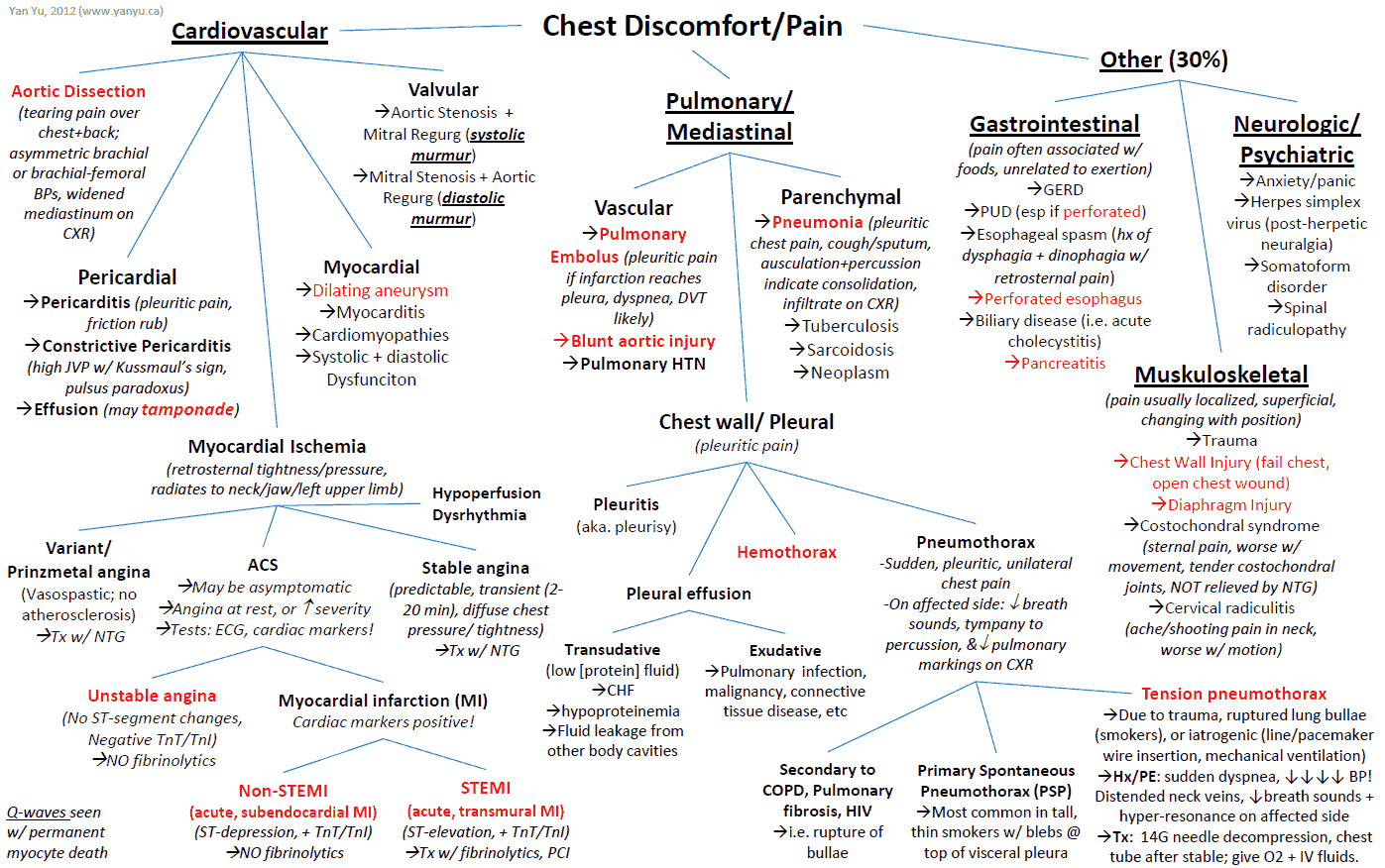
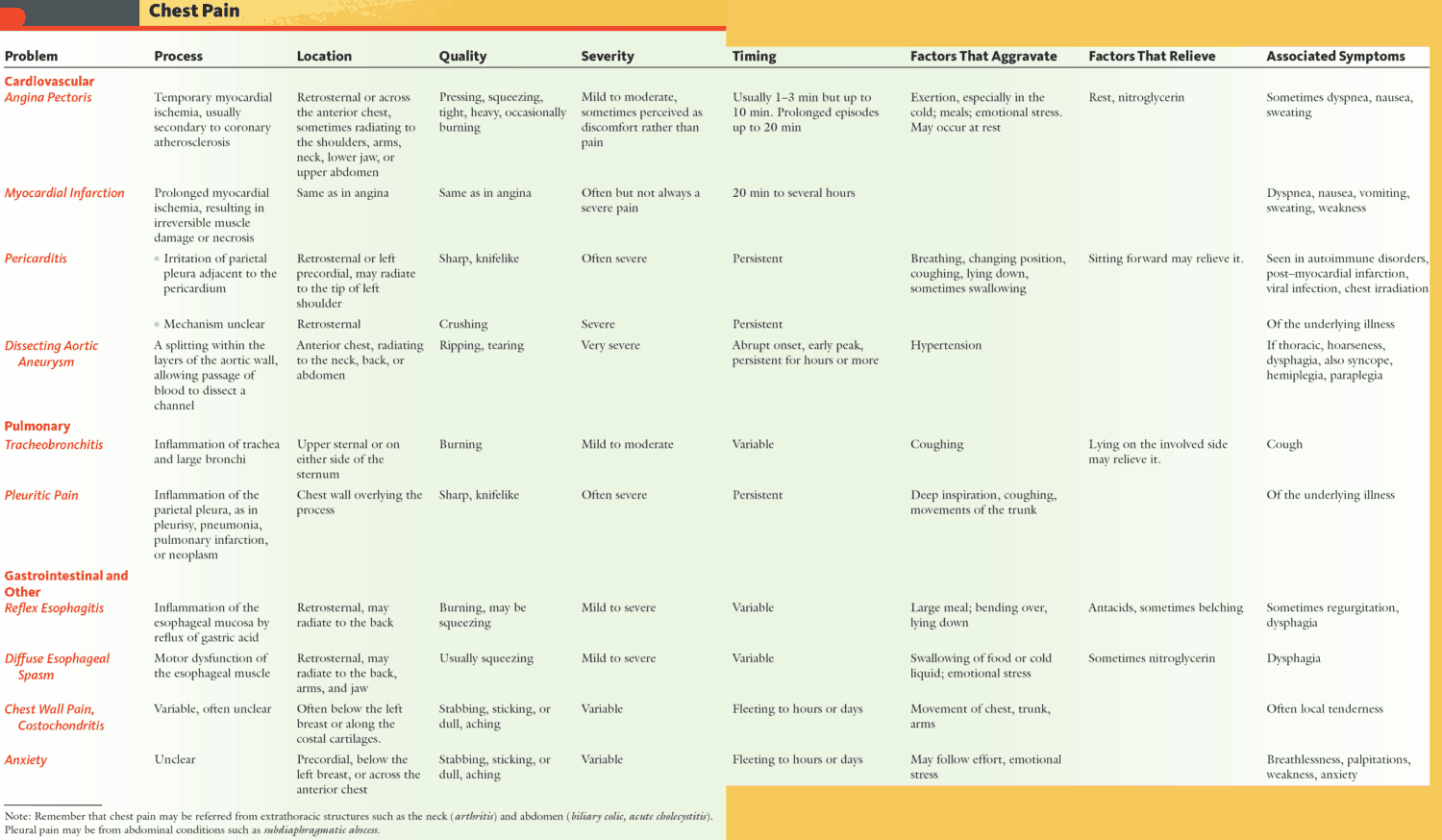
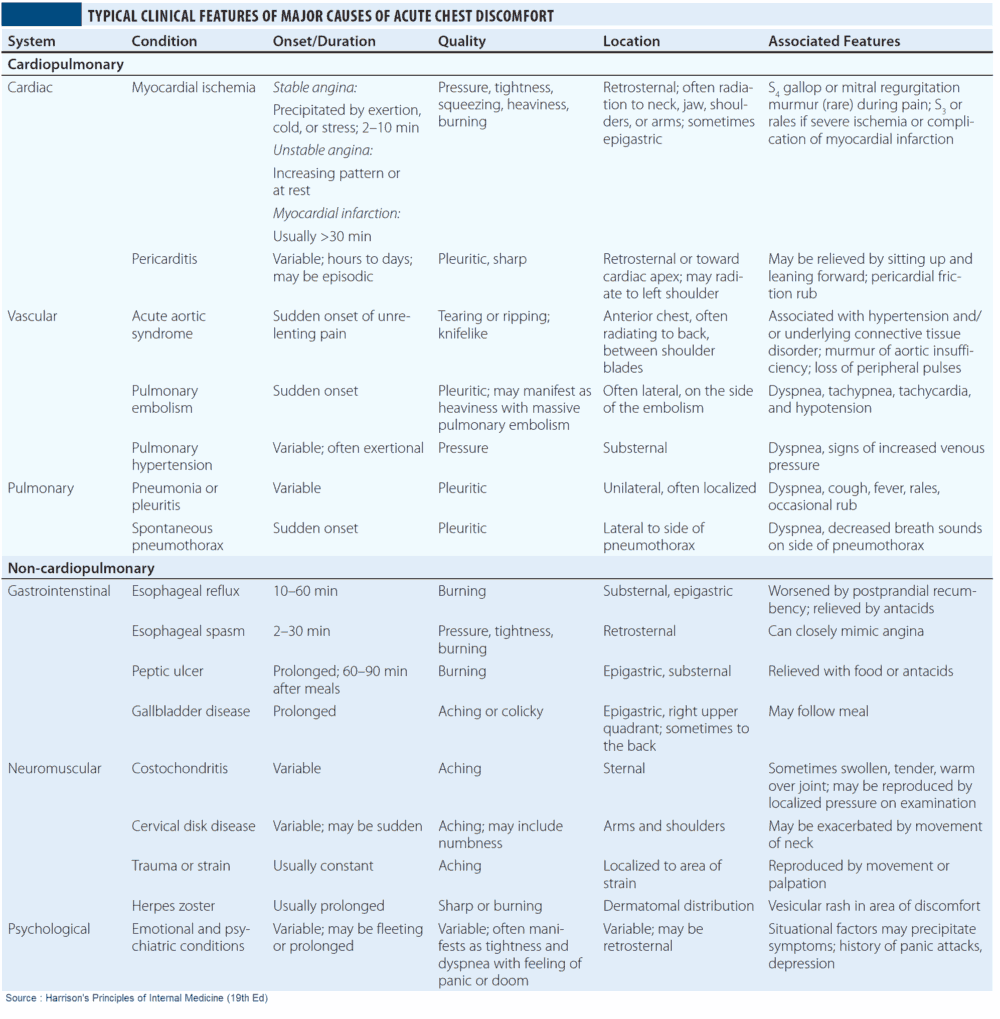
Causes and Differential Diagnosis of Chest Pain
Causes of Pleuritic Chest Pain
This is a sharp pain that is worse on deep inspiration, coughing, or movement. The differential diagnosis includes the following:
- Pneumothorax.
- Pneumonia.
- Pulmonary embolus (PE).
- Pericarditis: retrosternal.
- Bornholm disease (Coxsackie B unilateral infection of respiratory muscles).
Causes of Dull Central Chest Pain
The differential diagnosis of dull central pain includes the following:
- Angina: crushing.
- Myocardial infarction (MI): crushing.
- Dissecting aortic aneurysm: tearing interscapular pain.
- Aortic Dissection (tearing pain)
- Esophagitis: burning.
- Esophageal spasm.
- Esophageal tear (Boerrhave’s syndrome).
READ MORE:
Causes of Chest Wall Tenderness
The differential diagnosis of chest wall tenderness includes the following:
- Rib fracture.
- Shingles (herpes zoster): pain precedes rash.
- Costochondritis (Tietze’s syndrome).
- Nerve root compression.
READ MORE about: Non-Cardiac Causes of Chest Pain
Chest Pain as an Atypical Presentation
The differential diagnosis of chest pain as an atypical presentation (or in any of the above) includes:
- Anxiety and Panic Disorder
- Referred pain from vertebral collapse, causing nerve root irritation
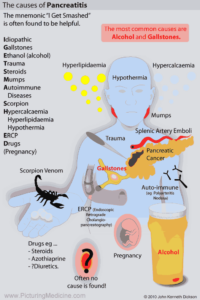
- Intra-abdominal pathology (e.g., pancreatitis, peptic ulcer, or the biliary tree)
In addition, any of the above diagnoses can present in an atypical manner. For instance, MI can present as epigastric or jaw pain. For this reason, the most serious causes of chest pain should always be added to the differential diagnosis and considered to avoid missing a potentially life-threatening problem.
READ MORE: Be Cautious Diagnosing Anxiety and Panic Disorder in Patients with Chest Pain and Anxiety
History and Symptoms in the Patient with Chest Pain
1. What type of chest pain does the patient have?
Onset and progression of chest pain
- Cardiac ischemic pain typically builds up over a few minutes and may be brought on by exercise, emotion, or cold weather.
- In stable angina the pain resolves on resting or with sublingual nitroglycerin (NTG).
- In unstable angina the pain may come on at rest and commonly waxes and wanes, becoming severe at times.
- In MI the pain is severe, often associated with systemic symptoms such as nausea, vomiting, and sweating, and lasts for at least 30 minutes.
- Spontaneous pneumothorax and pulmonary embolism usually causes sudden onset of pleuritic pain (patients often remember exactly what they were doing at the time).
- Esophageal disease is suggested by pain that follows an episode of vomiting, especially if hematemesis is present.
Always ask the patient what he or she was doing when the pain came on. This generally gives valuable information!
Site and radiation of chest pain
- Cardiac ischemia and pericarditis cause retrosternal pain
- In ischemia, the pain often radiates to the jaw, neck, or arms
- Dissecting aortic aneurysm causes a tearing interscapular pain
- Pulmonary disease causes unilateral pain which the patient can often localize specifically.
- Esophageal disease can also cause retrosternal pain and may mimic cardiac pain.
- Referred pain from vertebral collapse or shingles will follow a dermatome pattern.
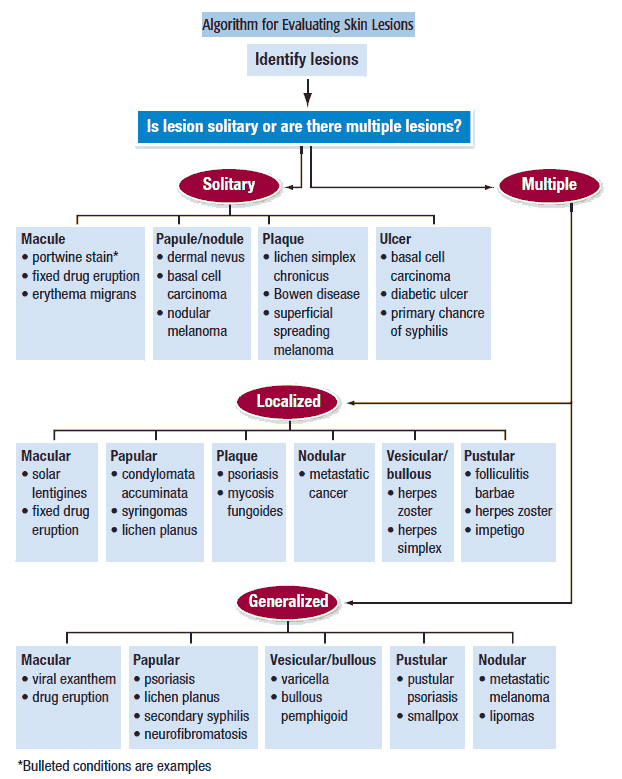
A note about shingles: Lesions never cross the midline except in patients with immunocompromise, which may be iatrogenic (e.g., steroid use) or due to another cause. In addition, the pain of shingles can begin before the rash appears. Patients complain of “electrical” type pain. Treatment with acyclovir is effective only if given within 24 hours of the initial rash.
Nature of chest pain
The precise nature of the pain gives important clues as to the underlying diagnosis-for instance, crushing, sharp, pleuritic, burning, or stabbing (see above).
2. Are there any associated symptoms?
Important associated symptoms include:
- Dyspnea: pulmonary embolism, pneumonia, pneumothorax, pulmonary edema in cardiac ischemia, hyperventilation in anxiety.
- Cough: purulent sputum in pneumonia, hemoptysis in pulmonary embolism, frothy pink sputum in pulmonary edema.
- Rigors: pneumonia (particularly lobar pneumonia).
- Calf swelling: has PE arisen from deep vein thrombosis? Bilateral swelling suggests heart failure.
- Palpitations: arrhythmia can cause angina or result from cardiac ischemia, PE, or pneumonia.
- Clamminess, nausea, vomiting, and sweating are features of myocardial infarction or massive pulmonary embolism.
Do not forget about anginal equivalents
Do not forget about anginal equivalents, such as those listed above, or jaw pain/tightness or indigestion. Anginal equivalents may be the only presenting symptoms of an MI, especially in elderly and diabetic patients. When in doubt, get an ECG and cardiac enzymes.
READ MORE about: Atypical Presentations of Acute Coronary Syndrome (ACS)
3. Are risk factors for diseases that cause chest pain present?
Important risk factors include:
- Ischemic heart disease: smoking, family history, cholesterol, hypertension, diabetes, male sex, age over 50 years.
- PE: recent travel, immobility, or surgery, family history, pregnancy, malignancy.
- Pneumothorax: spontaneous (young, thin men), trauma, emphysema, asthma, malignancy, staphylococcal pneumonia, cystic fibrosis.
READ MORE about: Nontraditional Risk Factors for Coronary Artery Disease (CAD) in Patients with Chest Pain
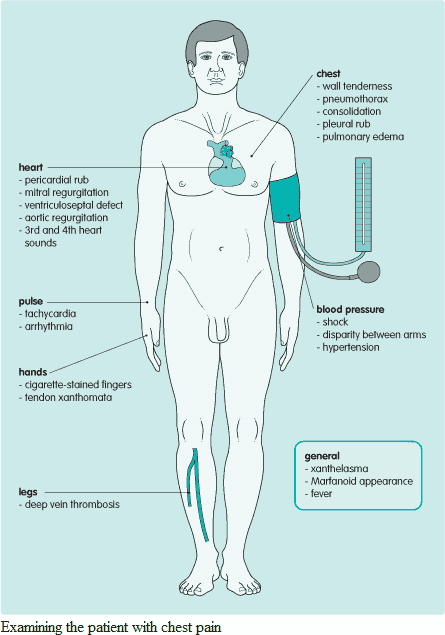
Examination and Signs in the Patient with Chest Pain
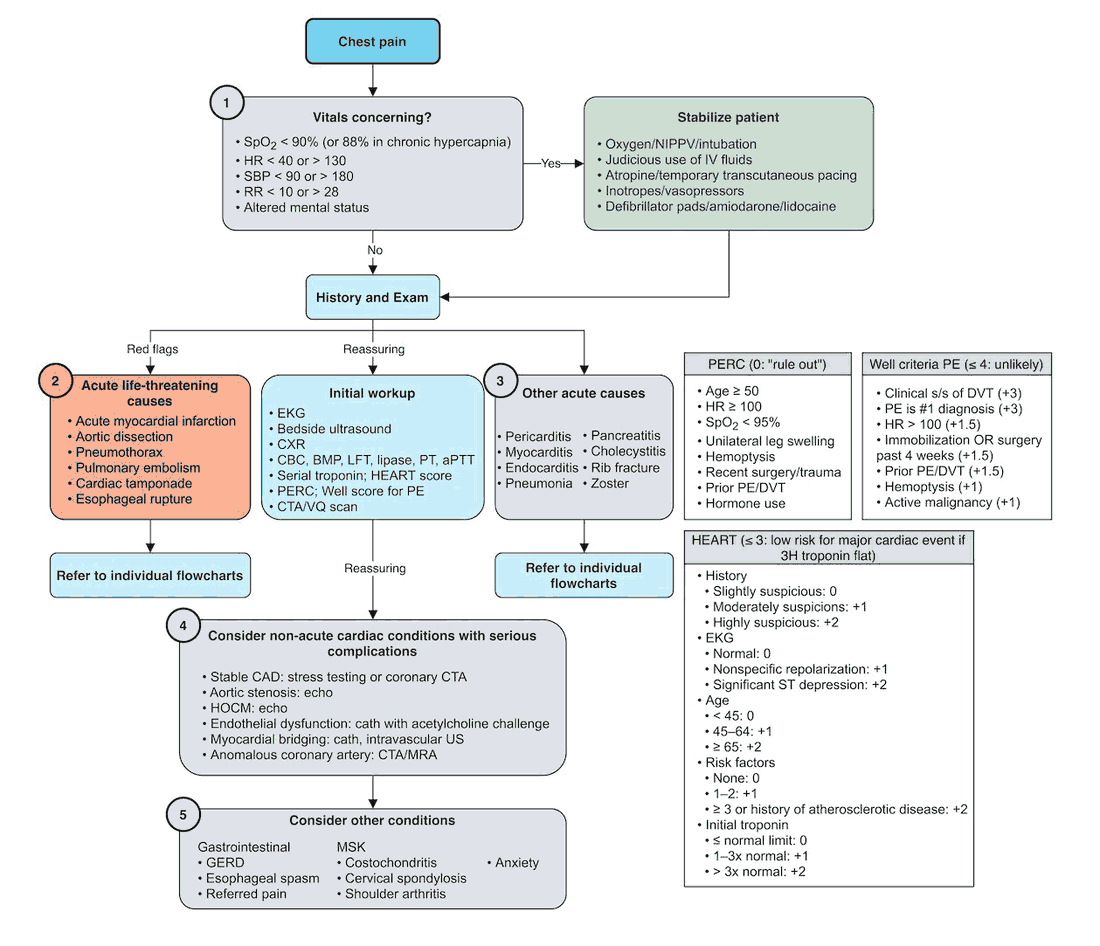
Vital signs are vital and therefore should be checked first. Get in the habit of checking the vital signs yourself to avoid error. The examination should focus on determining the cause of the pain and then looking for risk factors and consequences of the underlying problem. A schematic guide to examining the patient with chest pain is given in the image below.
What is the cause of the pain?
Pay particular attention to:
- Pulse: tachycardia or arrhythmia.
- Blood pressure: discrepancy between left and right arms in aortic dissection.
- Chest wall tenderness: rib fracture, costochondritis, anxiety, shingles.
- Chest examination: pneumothorax, consolidation, pleural rub.
- Cardiac examination: fourth heart sound (PE or MI), rub (pericarditis).
Are there risk factors?
The following risk factors may be present:
- Abnormal lipids: xanthelasma, tendon xanthoma.
- Nicotine-stained fingers: predisposition to ischemic heart disease.
- Hot, edematous, tender calf, suggesting deep vein thrombosis.
- Hypertension: ischemic heart disease.
Also look for signs of venous stasis and arterial insufficiency in the lower extremities. Is there a brown discoloration (hemosiderin staining due to blood pooling) of the ankles? Does the patient have palpable lower extremity pulses.
What are the complications?
Complications may include:
- Pulse: arrhythmia, tachycardia.
- Blood pressure: shock in tension pneumothorax, massive pulmonary embolism, MI.
- Heart failure: pulmonary edema and 3rd heart sound.
- Murmurs: acute mitral regurgitation and ventricular septal defect after MI; aortic regurgitation in dissecting aortic aneurysm.
READ MORE about: Heart Murmurs – Differential Diagnosis, Examination and Investigations
Investigating and Diagnosing the Patient with Chest Pain
All patients with chest pain should have an electrocardiogram (ECG), chest x-ray (CXR), and cardiac enzymes. Further investigation will be directed by findings in these tests in conjunction with the history and clinical examination. An algorithm for the investigation of the patient with chest pain is given in the image below.
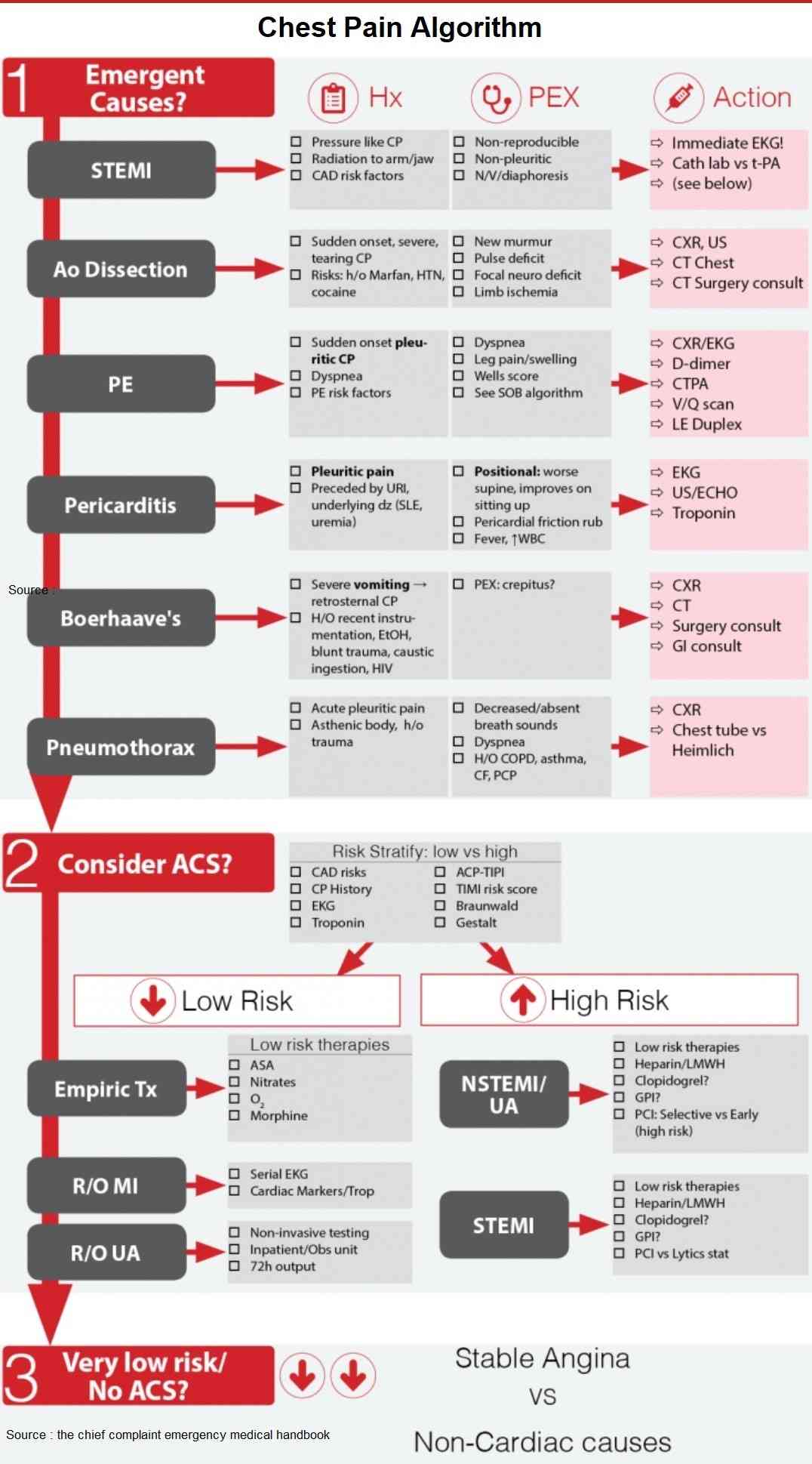
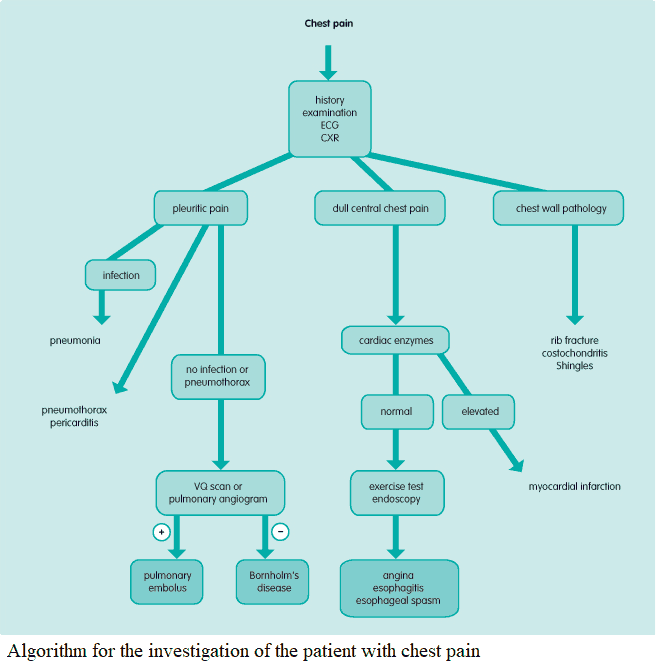
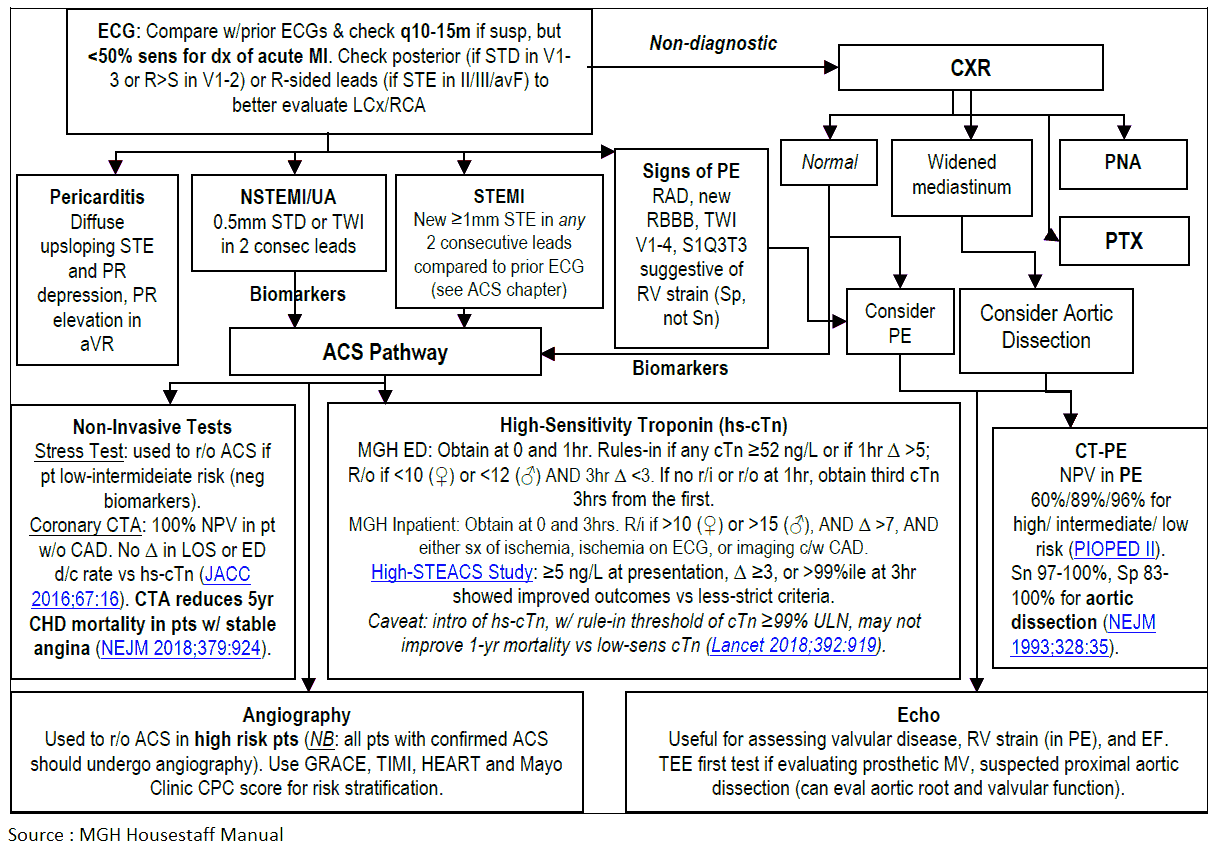
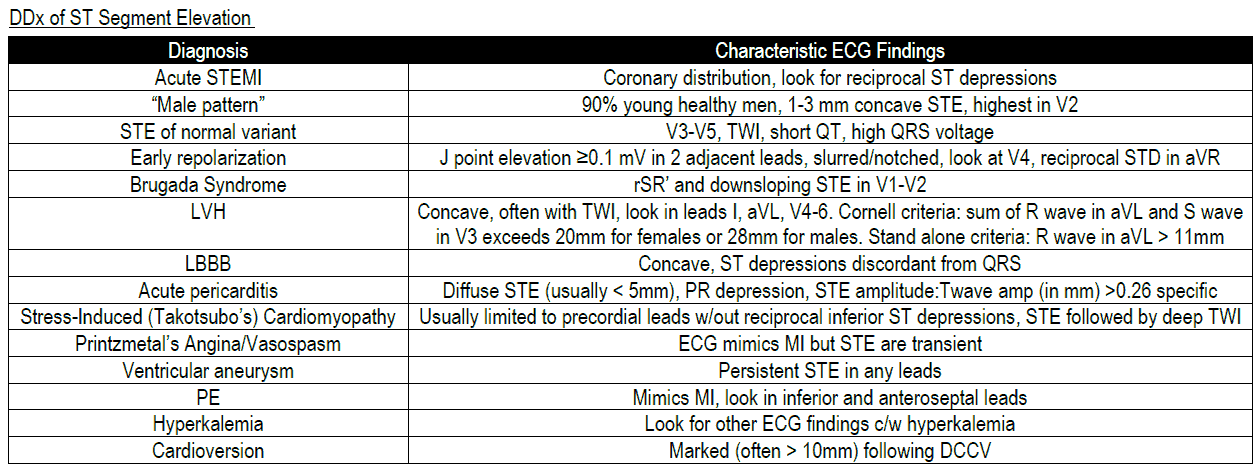
Electrocardiogram (ECG)
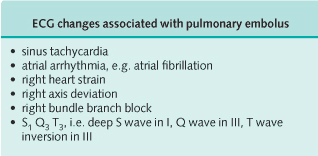
ST depression and elevation on ECG are suggestive of myocardial ischemia and acute MI, respectively. Changes suggestive of PE are shown in the image below. Arrhythmia may also be detected on ECG.
Chest x-ray
Pneumothorax, consolidation (pneumonia, PE), widened mediastinum (aortic dissection), pulmonary edema (myocardial ischemia/infarction) and fractured ribs may be detected on CXR.
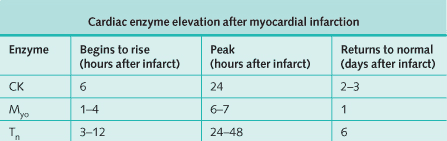
Cardiac enzymes
Serial cardiac enzymes should be assessed every 8 hours for 24 hours if MI is considered.
READ MORE about: Beware of the “Highly Sensitive” Troponin
Stress Test
An exercise test may be diagnostic when angina is suspected. Patients walk, ride a bike, or receive medication to increase the heart rate. These tests are done in conjunction with ECG monitoring, and a rest and stressed echocardiogram may also be used during this exam.
Any sign of ischemia, such as ST elevation/depression, a drop in blood pressure, chest pain, or arrhythmia, is grounds for stopping the exam.
Of note, exercise stress tests with ECG monitoring have a high false-negative rate in women. Therefore, it is often advantageous for a female patient either to undergo a nuclear medicine test, such as an adenosine/thallium stress test, or to go directly to catheterization. In the adenosine/thallium stress test, the heart is medically stressed and a radiolabeled tracer (thallium or sestimibi) is introduced to detect areas of low flow during stressed conditions.
READ MORE about: Don’t Stress the Stress Test in Suspected ACS
Coronary angiography
Coronary angiography allows direct visualization of the coronary arterial tree. It should be used in severe angina to determine whether angioplasty or coronary artery bypass grafting might be beneficial.
Angiography is becoming more and more common as the number of centers with interventional cardiologists increases. Patients with equivocal or positive findings on exercise stress tests, along with those who have “good stories” (i.e., risk factors for coronary artery disease) are taken to catheterization regularly.
Patients should undergo catheterization if they have two of the following three characteristics:
- Good clinical picture of angina/MI.
- Positive cardiac markers (troponin, CK-MB).
- ST segment changes on ECG or new left bundle-branch block (LBBB).
Arterial blood gases
The assessment of arterial blood gases is useful in determining the severity of PE, pneumonia, or pulmonary edema, showing hypoxia and occasionally hypocapnia. In hyperventilation related to anxiety, the pO2 will be elevated while there will be hypocapnia and a respiratory alkalosis.
Ventilation-perfusion scan
Ventilation-perfusion scan is used to diagnose PE. In some circumstances (e.g., when there is pre-existing obstructive airways disease) interpretation of this test can be difficult, so pulmonary angiography should then be performed. PE protocol CT can be used in addition to angiography in evaluating the patient with pre-existing pulmonary disease.
Echocardiogram
The presence of a dissecting aortic aneurysm should be confirmed by urgent echocardiography (particularly transesophageal echocardiography) or by computed tomography scan.
Urgent echocardiography is now used to help detect cardiac effusions and tamponade. Echocardiography also can be used to assess for possible sequelae of MI, such as myocardial dyskinesia, papillary rupture, or ventricular thrombus.
Upper gastrointestinal endoscopy
Upper gastrointestinal endoscopy will confirm esophagitis and should be considered when the cause of chest pain is unclear.