Diabetic kidney disease (DKD), or diabetic nephropathy, is a major contributor to chronic kidney disease (CKD). As the prevalence of diabetes continues to rise, so too does the burden of diabetes-related complications, especially those affecting renal function.
Despite advances in diagnostics and therapeutics, many patients with DKD remain undiagnosed or poorly managed until the disease has progressed to an advanced stage.
This article explores the latest developments in diabetic kidney disease management. We’ll focus on strategies that healthcare professionals can adopt to optimize patient care.
Understanding the Burden of Diabetic Kidney Disease
DKD poses a significant health burden, contributing to higher rates of cardiovascular events, hospitalizations, and mortality. Approximately one in three adults with diabetes has chronic kidney disease, and both type 1 and type 2 diabetes can lead to progressive kidney damage.
DKD is typically marked by albuminuria and a decline in estimated glomerular filtration rate (eGFR), yet early stages are often symptomless, making timely diagnosis difficult. High blood sugar levels gradually damage the nephrons, and coexisting high blood pressure accelerates this process.
Key contributors to DKD progression include:
- Hypertension
- Dyslipidemia
- Smoking
- Poor dietary habits
- Sedentary lifestyle
The Role of Early Detection and Risk Stratification
Early detection remains one of the most critical steps in improving outcomes for DKD. Screening should follow this timeline:
- At diagnosis for individuals with type 2 diabetes
- Five years after diagnosis for individuals with type 1 diabetes
Annual monitoring allows clinicians to identify renal decline early, enabling timely interventions that can slow disease progression and prevent complications. According to Nature, over 850 million people worldwide are estimated to have kidney disease. Alarmingly, up to 90% of individuals with CKD in these settings are unaware of their condition.
As the global population ages, CKD prevalence and mortality continue to rise, making it the third fastest-growing cause of death. Risk stratification, using biomarkers, glycemic control measures, and genetic indicators, improves personalized care. While artificial intelligence (AI) and machine learning show promise in enhancing early DKD diagnostics, current models for predicting disease progression remain limited.
Treatment Options
Management of diabetic kidney disease now includes both established and emerging therapies. They are:
- CE inhibitors and ARBs remain standard treatments for managing DKD.
- SGLT2 inhibitors such as canagliflozin and dapagliflozin have proven effective in slowing disease progression.
- Clinical trials like CREDENCE and DAPA-CKD support the use of these medications even in patients with controlled glucose.
- GLP-1 receptor agonists are beneficial for patients with cardiovascular comorbidities, supporting glycemic control and weight loss.
- Wearable biosensors offer continuous glucose monitoring, enhancing accessibility and patient engagement.
Together, these innovations enhance DKD treatment. However, success depends on consistent delivery through coordinated healthcare systems to ensure these therapies reach those who need them most.
Strengthening Care Delivery Through Interdisciplinary Collaboration
Improving outcomes in diabetic kidney disease (DKD) depends not only on the treatments prescribed but also on how care is delivered. Fragmented care often leads to delayed referrals, therapeutic inertia, and poor adherence.
In contrast, bringing together endocrinologists, nephrologists, primary care physicians, and nurse practitioners (NPs) can promote cohesive care and timely interventions. Multidisciplinary clinics and shared-care models are increasingly effective in managing DKD, helping to reduce disease progression and improve patient satisfaction.
NPs, with their advanced clinical training, play an essential role in patient education and medication management. They often serve as the connection point between various specialties, ensuring coordinated and comprehensive care. For nurses looking to step into these impactful roles, RN to MSN programs offer a direct path.
According to Wilkes University, an MSN is required to become an NP or advanced practice registered nurse. The program’s coursework prepares individuals for leadership roles and advanced clinical responsibilities.
Empowering Patients Through Education and Self-Management
Effective diabetic kidney disease management depends on patient engagement. When individuals understand their condition and participate actively in their care, outcomes improve significantly. Education should cover recognizing early symptoms, interpreting lab results, managing comorbidities, and adhering to prescribed treatments.
According to the CDC, diet plays a major role in controlling diabetes and protecting kidney function. A diabetes-friendly diet resembles a generally healthy one:
- Eat fruits, vegetables, lean proteins, and healthy fats
- Limit sugar, refined carbs, and salt
- Customize carbohydrate intake based on age, medications, and activity level
For chronic kidney disease (CKD):
- Reduce sodium to control blood pressure and prevent fluid buildup
- Limit high-phosphorus foods like dairy, beans, and dark sodas
- Be cautious with potassium-rich foods (e.g., tomatoes, potatoes)
- Balance protein intake; too much or too little can worsen CKD
Digital self-management tools and mobile apps further empower patients, encouraging real-time tracking and more proactive, informed care.
Frequently Asked Questions (FAQs)
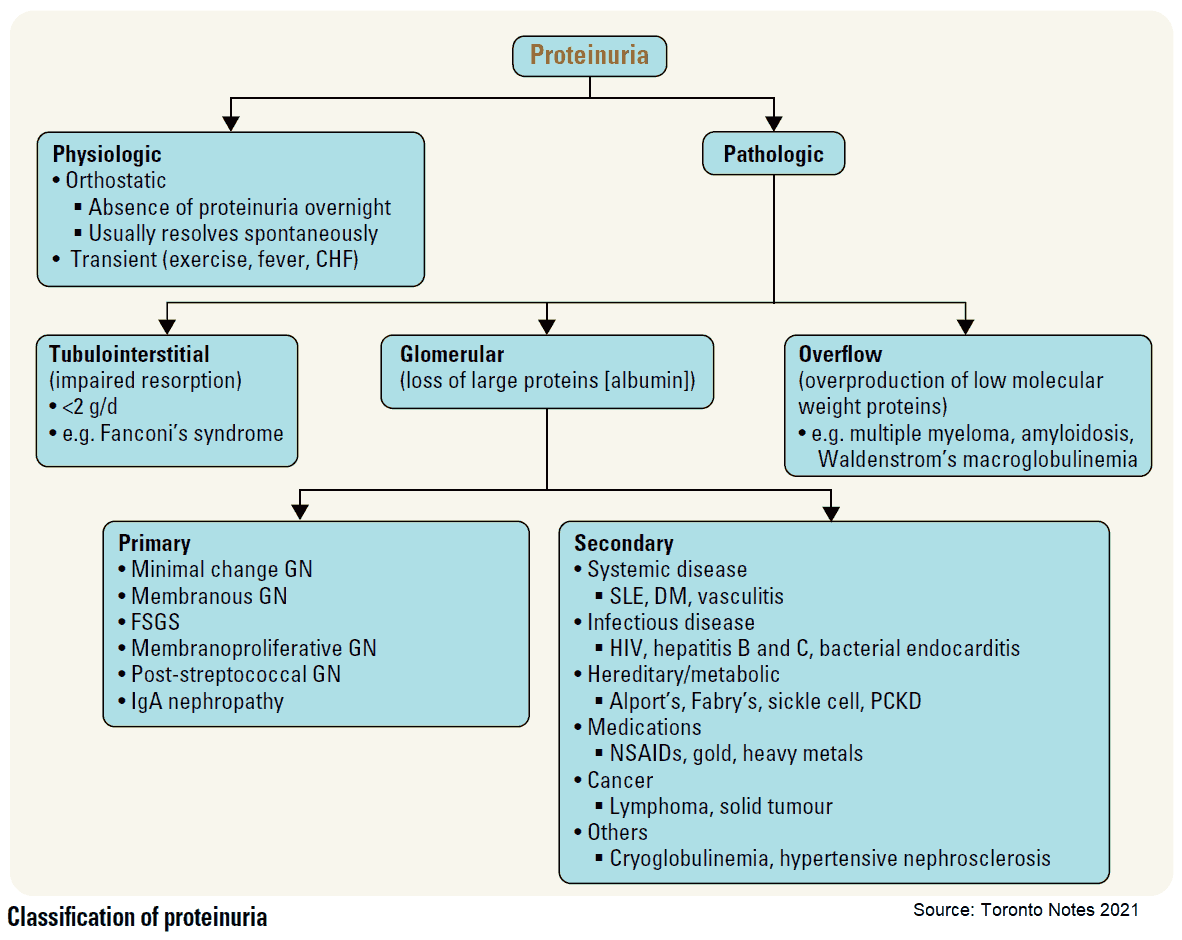
What is the earliest indicator of diabetic kidney disease?
The earliest indicator of diabetic kidney disease is microalbuminuria, which refers to the presence of small amounts of albumin in the urine. Detectable through urine tests, it signals early kidney damage even before noticeable symptoms appear and often precedes a decline in glomerular filtration rate (GFR).
How do SGLT2 inhibitors help in managing DKD?
SGLT2 inhibitors reduce blood glucose by preventing renal glucose reabsorption and have been shown to provide additional kidney and cardiovascular protection. They slow the progression of kidney disease, reduce proteinuria, and lower the risk of ESRD in patients with DKD.
What role do nurse practitioners play in diabetic kidney disease care?
Nurse practitioners perform critical functions in DKD care, including patient assessment and medication management. They also provide lifestyle counseling, coordinate chronic care, and conduct regular monitoring. With advanced training, they are integral to interdisciplinary teams aiming to slow disease progression and improve quality of life for patients.
Diabetic kidney disease presents a growing global health challenge that demands coordinated, evidence-based strategies across the continuum of care. From early detection to advanced therapies and integrated, education-driven care, multiple pillars must align to change the course of this progressive condition.
As care demands intensify, the value of interdisciplinary teams is more evident than ever. Through innovation, collaboration, and patient empowerment, healthcare providers can significantly improve DKD outcomes and reduce its long-term burden.
This article is a guest contribution submitted by a professional healthcare writer and reviewed for accuracy.