Table of Contents
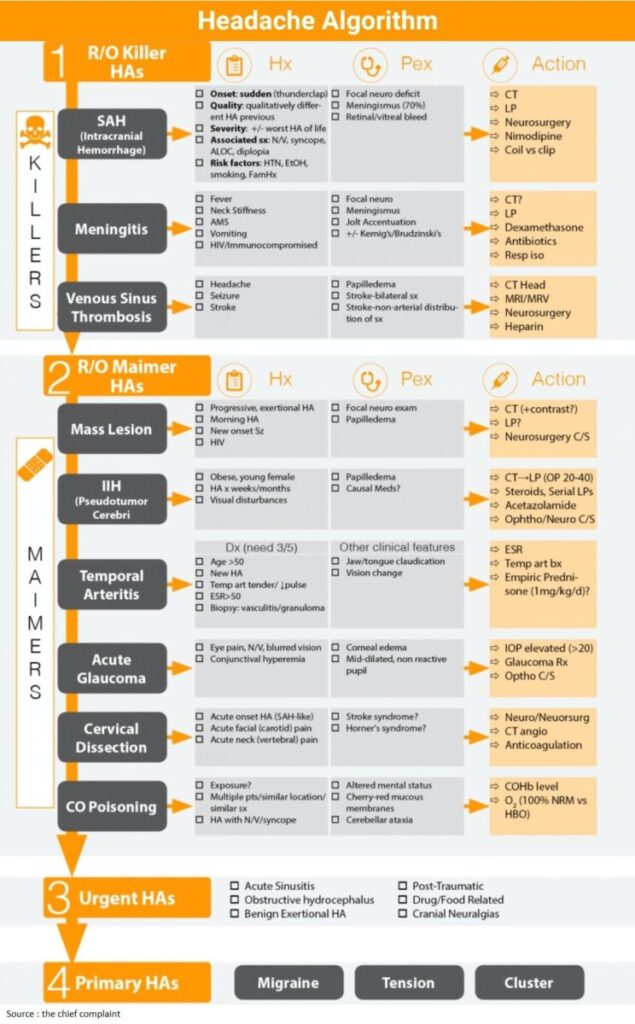
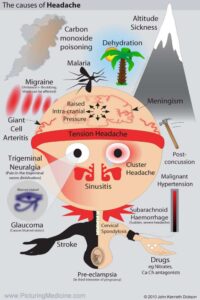
Critical / Killer Headaches
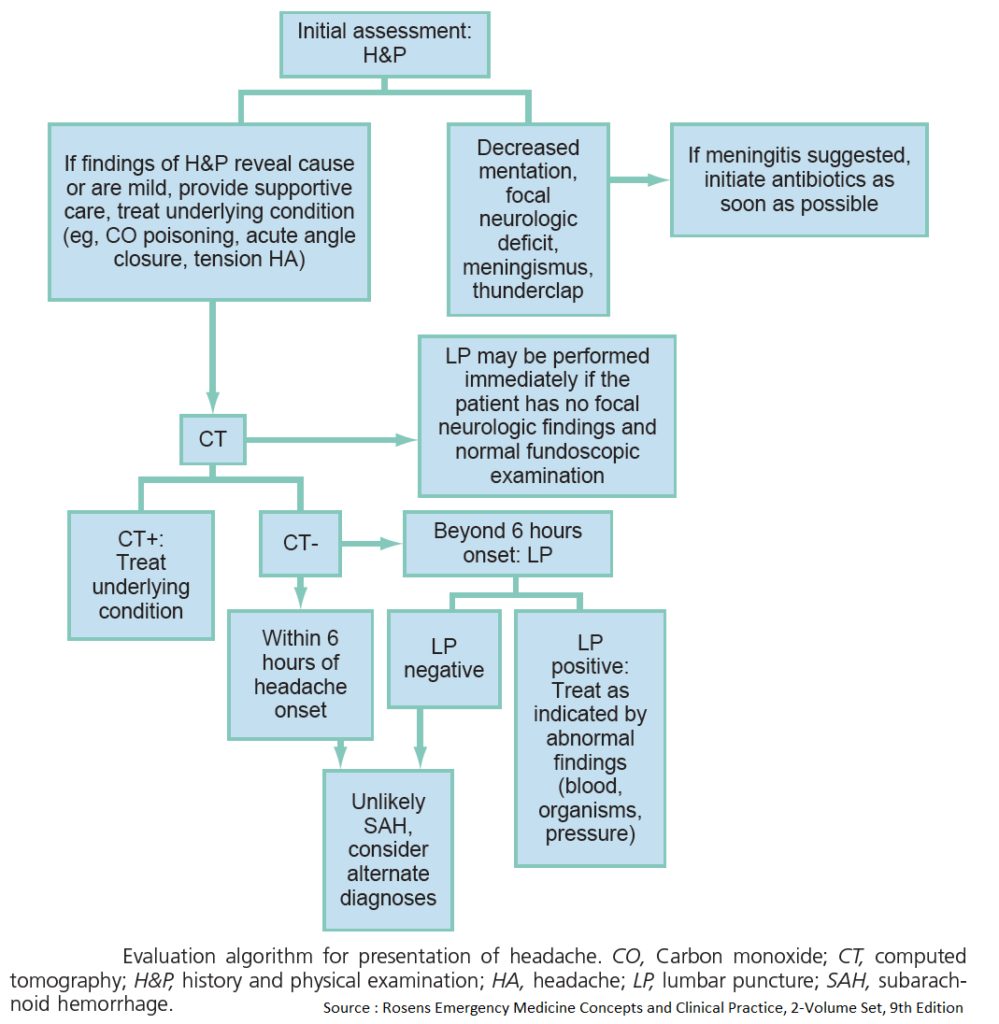
General Approach:
- Emergency department evaluation relies on excluding life-threatening causes of Headache (killers), specifically SAH and meningitis
- Then consider other serious causes of headache that can debilitate the patient (the maimers)
- When these have been excluded, we can then diagnose primary headache syndromes.
Testing
- Question 1: Does this patient need a CT? (ACEP Guidelines Ann Emerg Med 2008;52:407)
- Neuro exam-new abnormal findings (focal deficit, Altered mental status) (ACEP Level B)
- New, sudden, severe Headache
- HIV + with new Headache
- Patients older than 50 with new type of Headache (ACEP Level C)
- Question 2: Does this patient need an Lumbar Punction?
- R/O SAH: Sudden-onset, severe headache + CT Head (-) → LP to exclude SAH (ACEP Level B)
- Concern for Meningits (Cell count, OP, gram stain)
- Concern for Idiopathic Intracranial Hypertension (Opening pressure)
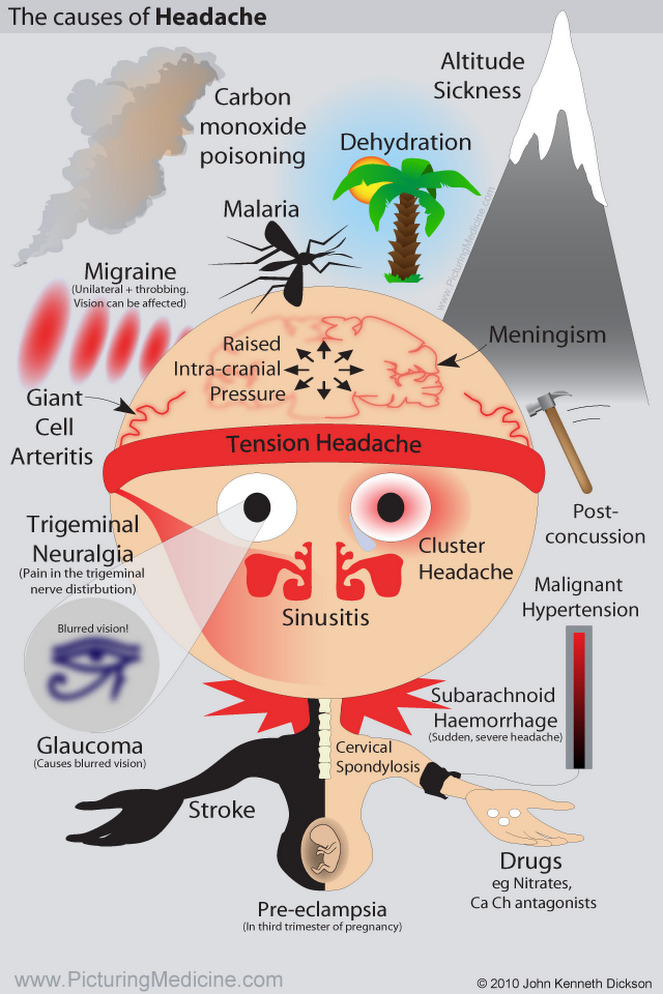
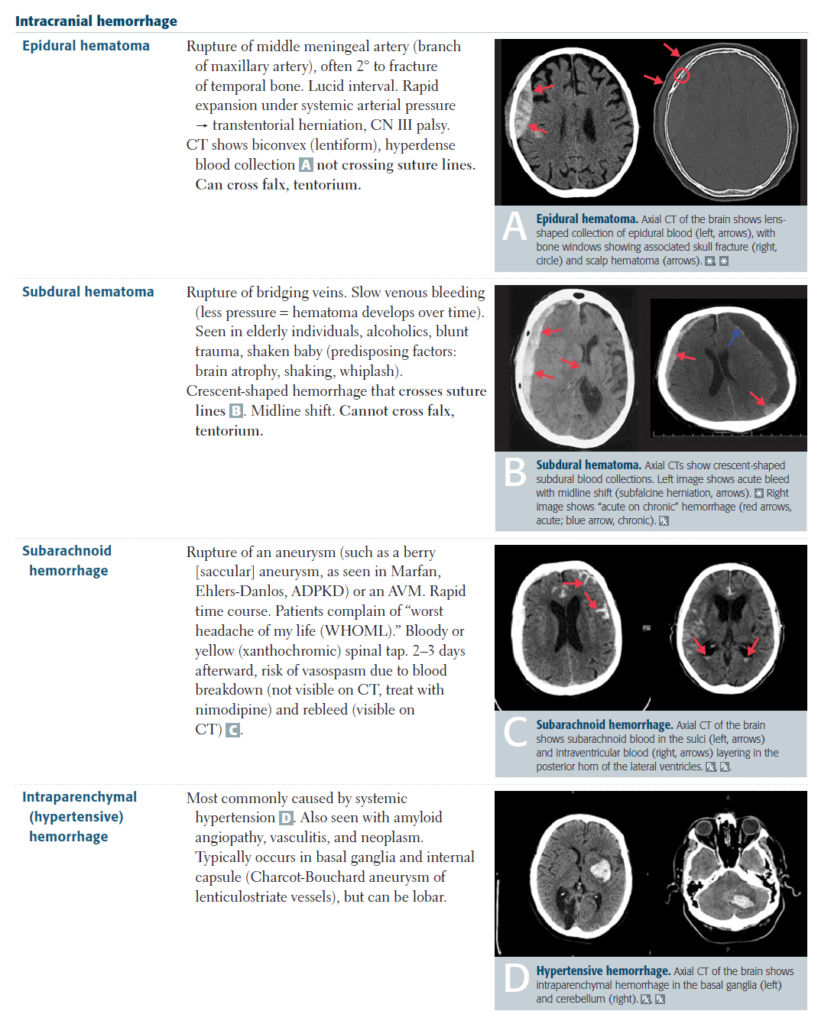
1. Subarachnoid Hemorrhage (SAH)
Clinical presentation
- Onset: sudden (thunderclap)
- Maximum severity is reached instantaneously in 50% and within 1-5 minutes in 19% of patients with SAH. (J Neurol Neurosurg Psychiatry 1998;65:791-3)
- Sudden severe Headache: (Lancet 1994:344:590-3)
- SAH in 25%
- Benign thunderclap headache in 40%
- Remaining will have another primary or secondary HA
- Therefore, all patients with sudden severe Headache need to be worked-up for SAH
- Other qualities
- Quality: qualitatively different headache from previous
- Severity: +/- worst headache of life
- Associated sx: Nausea / Vomitus, syncope, Altered Level of Consciousness, diplopia
- Risk factors: HTN, EtOH (alcohol), smoking, Family History
- Physical Examination:
- Focal neuro deficit
- Meningismus (70%)
- Retinal/vitreal bleed
- Clinical Presentation of SAH lies on a spectrum (Emerg Med Clin N Am 2003;21:73-87)
- The classic (middle of the spectrum) presentation is that of sudden onset and distinct HA, worst of their life associated with neck pain, Nausea / Vomitus
- On the extreme end, they can present with focal neuro deficit and Altered Level of Consciousness / Altered mental status
- On the subtle end 1/3 present with only Headache without neuro deficits, and are likely to be misdiagnosed
SAH Red Flags
□ Sudden onset
□ Maximal at onset
□ Different from previous Headaches
Work-up
- CT Head
- CT sensitivity is extremely high early but rapidly diminishes with time
- Misses about 2% of SAH within 12 hours and 7% by 24 hours
- Therefore anyone with suspected SAH and normal CT requires an Lumbar Puncture
- Journal Club (EM:RAP 3/14; 12/13)
- CT within 6 hours (BMJ 2011;343:d4277)
- Overall CT sensitivity is 93% (Sensitivity after 6h is 86%)
- CT within 6 hours of HA onset → Sensitivity 100%, Specificity 100%, NPV 100%
- Prospective cohort study
- CT within 6 hours (Stroke 2012;43:2115)
- CT within6 hours of HA onset → Sensitivity 100% with 2 caveats
- Caveat1: <6h rule only applies to pts with HA (not neck pain)
- Caveat2: Experienced neuroradiologists needed to interpret CT
- Editorial (Stroke 2012;43:2031)
- … we believe that practice should change. Neurologically intact patients who present with thunderclap headache and undergo CT scan within 6 hours of symptom onset no longer need an LP to exclude SAH if the CT scan is negative.”
- CT within 6 hours (BMJ 2011;343:d4277)
- Lumbar Puncture
- Timing: Results depends on timing of HA (J Emerg Med 2002;23:67-74)
- <12h:
- Xanthochromia may/may not be present; large RBCs should be present
- Incompletely clearing RBCs ?? (if suspected traumatic tap → repeat at different interspace)
- 12h-2weeks:
- Xanthochromia highly suggestive of SAH; large RBC +/- present 2weeks: Both may be absent.
Treatment (See ICH Algorithm)
- ABC/Resus/Airway
- Treat like ICH patient
- Intubate if Altered mental status, not protecting airway → document good neurologic exam prior
- Emergent Neurosurgical consultation
- Vasospasm prevention
- Nimodipine 60 mg po/NG q4h x 21d
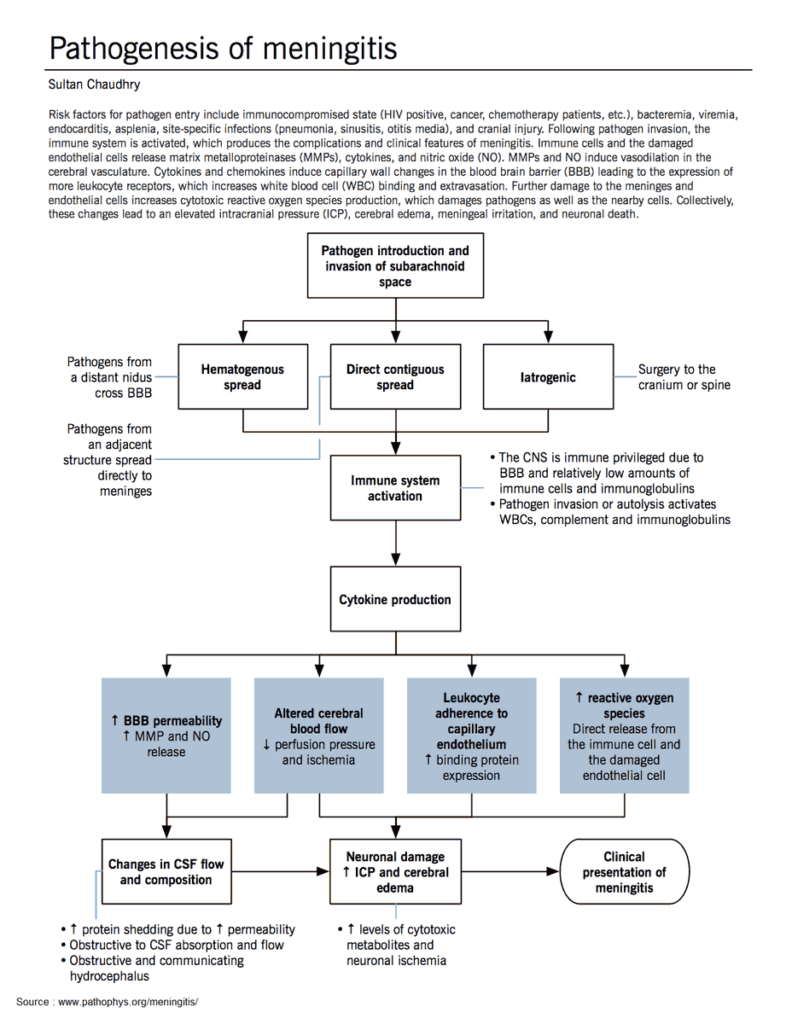
2. Meningitis
Read Also : Diagnosing and Treating Meningitis
Etiology
- Bacterial
- Meningococcus (Neisseria meningitidis)
- Streptococcus pneumoniae
- Haemophilus influenzae
- Listeria monocytogenes
- Viral
- Enteroviruses (≈ 85% of meningitis)
- Arboviruses (West Nile, etc…)
- Herpes viruses
- Others (Mumps, LCMV etc…)
Meningitis symptoms
Fever 85%
Stiff neck 70%
Altered mental status 67%
HeadAche 50%
Focal neuro 23%
Rash 22%
Clinical Presentation
- Classic triad
- All 3: fever, neck stiffness and Altered mental status present in only 44%
- Absence of all 3 virtually eliminates a diagnosis of meningitis
- 95% patients had 2 out of 4 of: (NEJM 2004;351:1849-59)
- Headache
- Fever
- Neck stiffness
- AMS
- All 3: fever, neck stiffness and Altered mental status present in only 44%
- Meningismus
- Jolt accentuation (JAMA 1999;282(2):175-81)
- Procedure: Ask patient to turn head right/left, 2-3 rotations per second
- Positive test: Worsening of headache
- Absence of jolt accentuation has a sensitivity of 100% for ruling out meningitis
- Kernig’s sign (inability to straighten the leg when the hip is flexed to 90 degrees)
- Brudzinski’s sign (forced flexion of the neck elicits a reflex flexion of the hips)
- Kernig/Brudzinski both have very low sensitivity ≈ 5%
- Jolt accentuation (JAMA 1999;282(2):175-81)
- Other symptoms:
- Abnormal neurologic exam
- Leg pain, refusal to walk (Meningococcus)
- Photophobia, N/V, lethargy
- Petechial rash (Meningococcus)
Bottom Line
- Triad: Absence of all of the triad (fever, Altered mental status, neck stiffness) → eliminates a diagnosis of meningitis
- Meningismus: Kernig/Brudzinski are not helpful in ruling out meningitis (low sensitivity)
- If they are positive → can rule in meningitis (high specificity)
- Jolt accentuation negative essentially eliminates a diagnosis of meningitis
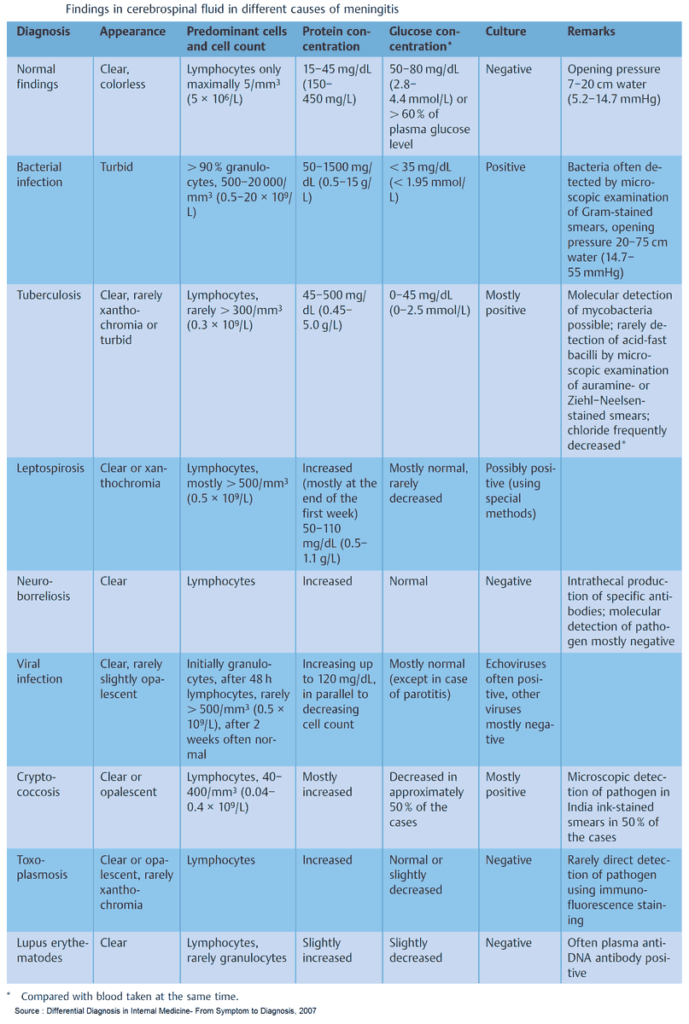
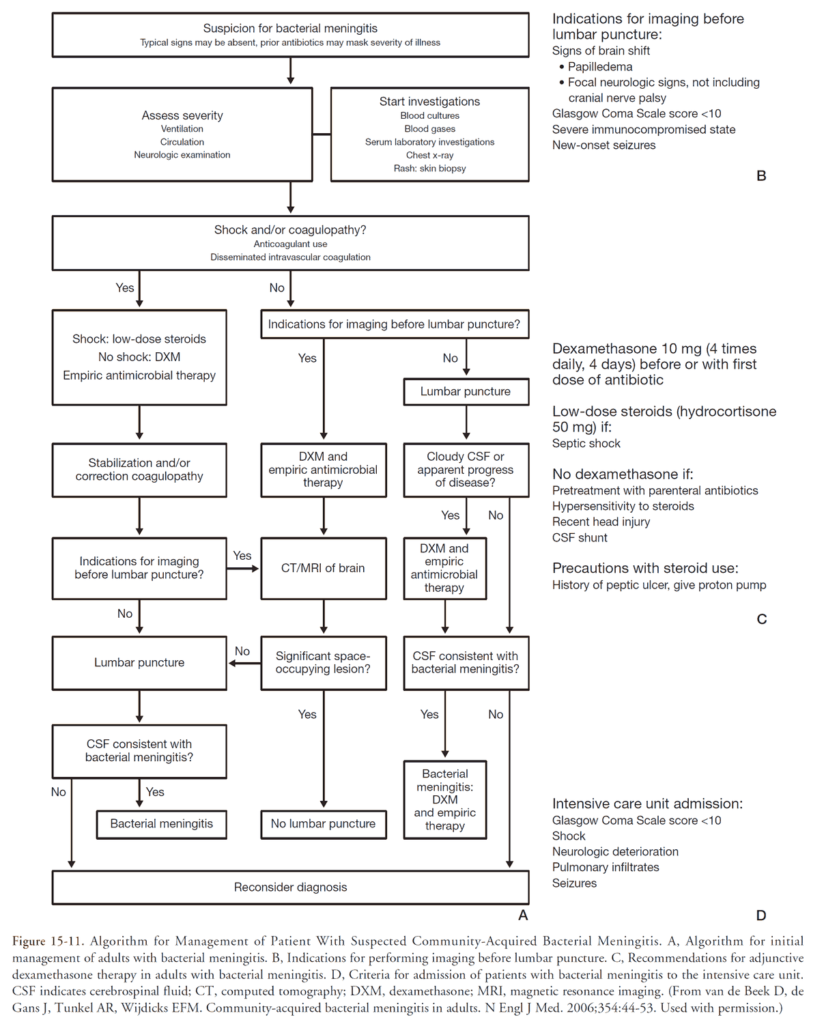
Work-up
- Lumbar puncture
- Tube 1&4: Cell count and diff
- Tube 2: glucose and protein
- Tube 3: Gram stain, culture, HSV PCR
- Do I need a CT before LP? (2 studies say not always) MAY omit if:
- Age<60, no immunocompromised/CNS disease/seizure within 1 week and has a nonfocal neuro exam (NEJM 2001;345:1727-1733)
- Absence of AMS, focal neuro exam, papilledema and favorable clinical impression by doctor (Ann Int Med 1999;159:2681-2685)
- CSF analysis (predictive of bacterial meningitis) (JAMA. 1989;262(19):2700)
- ↑ WBC > 2000
- Multiple studies show bacterial meningitis incidence of 5-19% in patients with CSF WBC < 100!
- No single variable can r/o meningitis
- Neutrophil > 1180
- CSF glucose <34mg/dL
- CSF protein > 220 mg/dL
- Gram stain +
- ↑ WBC > 2000
Treatment
- Antibiotics
- Timing
- Administer as soon as possible-before Lumbar puncture
- Multiple studies have shown an association between time of antibiotic administration and poor outcome (greater than 4-6 hours)
- Empiric antibiotics
- Ceftriaxone 2gm IV or Cefotaxime 2gm IV immediately +
- Vancomycin 1gm IV (15-20mg/kg) +
- Ampicillin 2gm IV (adults > 50yo)
- Timing
- Dexamethasone
- Dose: 10mg IV q 6 hour x 4 days; start 15 minutes prior to, or with first dose of antibiotics
- Journal club (Cochrane Database 2010;9:CD00405)
- No mortality benefit but helps prevent hearing loss and short-term neurologic sequelae
- Benefits seen mostly in patients with S. pneumoniae
- Acyclovir
- Dose: 10mg/kg q 8h for HSV
Special Case: HA and HIV (CD4 < 200?)
- CT w/wo contrast:
- R/O mass lesion, toxo, lymphoma
- Serum
- If serum crypto Ag(-) → likely do not need Lumbar puncture (patient very unlikely to have crypto infection)
- Lumbar puncture
- Use: r/o cryptococcal meningitis
- India ink: round encapsulated yeast (75% patients)
- CSF crypto Ag: Sensitivity 93 to 100% and specificities 93 to 98%
- CSF culture: definitive diagnosis
- Treatment: Amphotericin + Fluconazole
3. Cerebral Venous Thrombosis
General
- CVT = DVT of the brain = blood clots in brain (venous)
- CVT = Dural sinus thrombosis, (superior, sagittal, inferior) sinus thrombosis, cortical vein thrombosis
Risk factors
- Thrombophilia/Hypercoagulable state
- Pregnancy/Puerperium
- Medications (Oral contraceptive pills, Doxycycline)
- Cancer/Inflammatory/Hematologic disease
Clinical
- Presentation spectrum: Headache → Seizure → Stroke
- Headache
- Headache type: No characteristic history, multiple types of headache symptoms
- Physical Exam – Papilledema present in most cases (fundoscopic, pan-optic or US)
- Seizure
- Stroke
- Bilateral neuro deficit
- Non-arterial distribution
Diagnosis
- D-dimer – low sensitivity, not useful
- CT Head – normal in 30% of cases
- Highly suggestive:
- Dense triangle sign (thrombosed sup sag sinus posteriorly)
- Cord sign (thrombosed cortical vein)
- Bilateral edema/ICH
- Diagnostic (CT w/ contrast-venogram): Empty delta sign (flow defect in sup sag sinus)
- Highly suggestive:
- MR Brain with venography (study of choice)
Complications
- Intracranial Hypertension (ICH) → Coma → Death
- PE (pulmonary embolism)
Treatment
- Neurosurgical consultation
- Anticoagulation
- Heparin safe, even with hemorrhagic infarcts
- Journal Club-Heparin anticoagulation
- Cochrane Review of Heparin anticoagulation (Cochrane Database Syst Rev 2001;(4))
- RR of death 0.33 (95% CI 0.08-1.21) → not statistically significant
- Conclusion: CVT is a rare and fatal disease and no other treatment exists
- ISCVT-International Study on Cerebral vein and Dural Venous Thrombosis (Stroke 2004;35:664-70)
- Prospective observational study 624 patients → 80% received anticoagulation
- 6.8% mortality
- Cochrane Review of Heparin anticoagulation (Cochrane Database Syst Rev 2001;(4))
Emergent Diagnoses / Emergent Causes of Headache
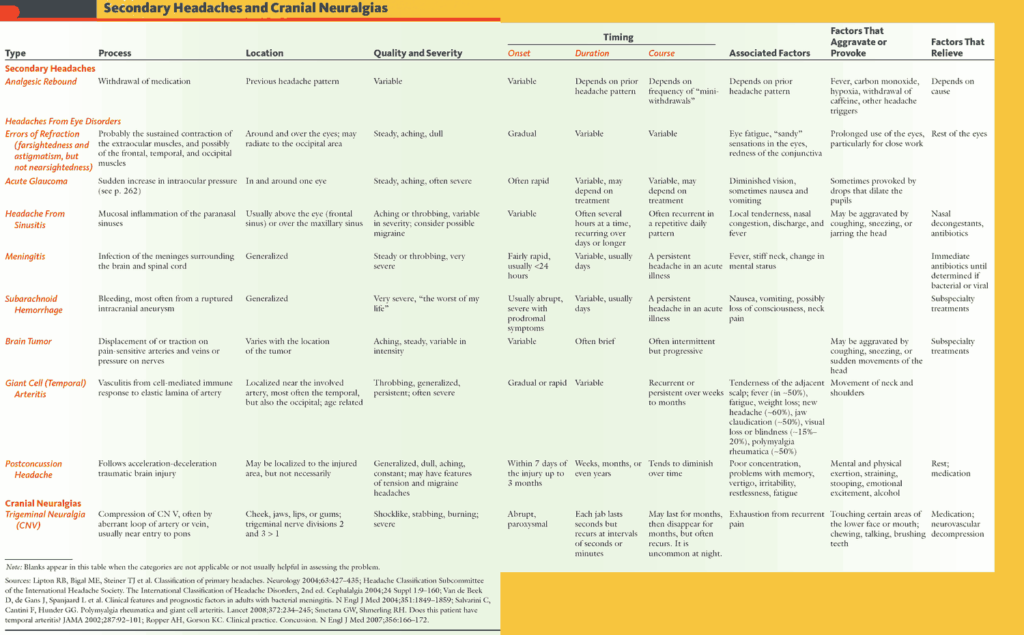
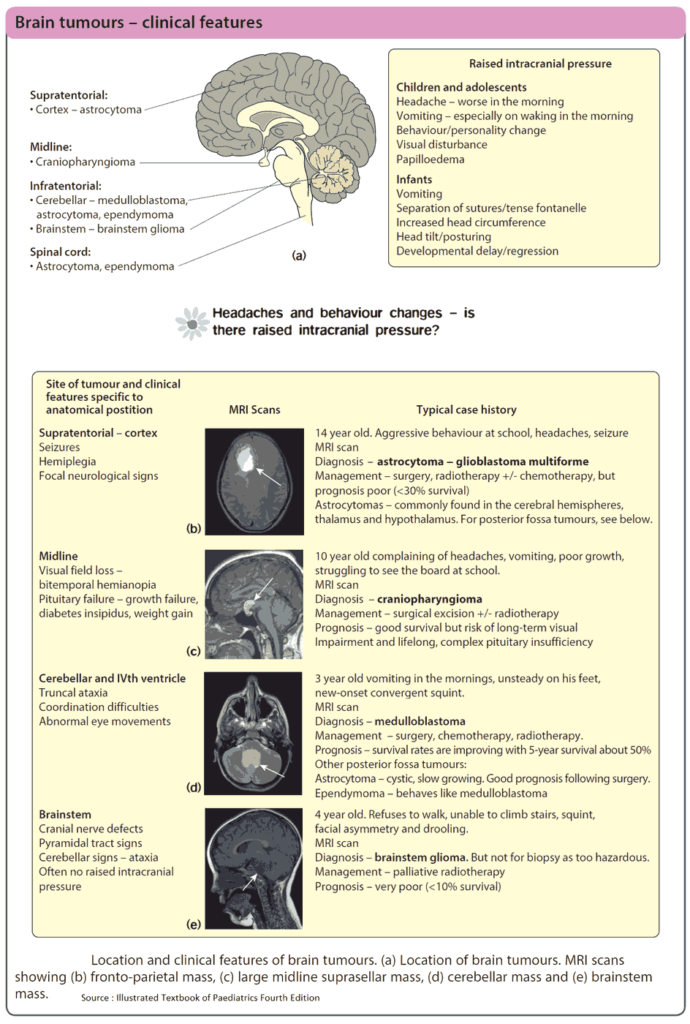
1. Brain Mass Lesion
Etiology
- Tumor, abscess, chronic subdural hematoma (SDH)
Clinical Presentation
- Progressive, exertional headache, morning headache
- New onset seizure, nausea/vomiting
- H/O HIV (cryptococcus, toxoplasmosis, lymphoma, and tuberculosis)
- Physical Exam : Focal neuro exam, papilledema, aphasia
Work-up
- CT Head w/wo contrast, MRI
Treatment
- Neurosurgical consultation, steroids, ventriculostomy
Vasogenic edema
- Etiology: tumor related disruption of BBB
- Treatment:
- Glucocorticoids – indicated in all patients with peri-tumor edema
- Dexamethasone 10mg IV x 1 then 4mg IV q6h
HYDROCEPHALUS
- Cause: CNS infection, hemorrhage, tumor
- Types
- Communicating hydrocephalus
- Symmetric dilation of all 4 ventricles
- Extraventricular obstruction or impaired CSF absorption, usually in neonates/infants;
- Adult causes: pseudotumor cerebri
- Non-communicating (Obstructive) hydrocephalus
- Asymmetric dilation of ventricles
- Communicating hydrocephalus
- Treatment
- Third Ventriculostomy – only effective for obstructive hydrocephalus
- Shunt (VP-Shunt) – can be used to treat either cause of hydrocephalus
SHUNT COMPLICATIONS
- Shunt Infection (Ventriculitis)
- 5 to 15 percent of procedures, most occurring in first 6 months
- Persistent fever → tap shunt
- Antibiotics, shunt may need removal
- Shunt mechanical failure (obstruction at the ventricular catheter)
- CT: Hydrocephalus
- Overdrainage
- Presentation: neurological symptoms → postural headache and nausea
- CT: Slit ventricle syndrome (small or slit-like ventricles)
2. Idiopathic Intracranial Hypertension (IIH)
General
- AKA Idiopathic Intracranial Hypertension, Pseudotumor cerebri
Presentation
- Obese, young female
- Headache x weeks/months
- Visual disturbances
- Papilledema
- Not all patients with IIH have papilledema
Diagnosis
- Diagnostic criteria for IIH: (Neurology 2002;59:1492-95)
- S/Sx of elevated intracranial pressure
- Non focal neuro exam (except abducens nerve paresis)
- Normal neuroimaging study (CT w/ con or MRI/MRV)
- Increased CSF pressure (nonobese>200; obese>250 mm water)
- No other cause of increased intracranial pressure (CNS tumor, encephalitis, right heart failure)
- Vision loss secondary to papilledema is the only serious complication of IIH, is avoidable with appropriate treatment
- MRI/MRV to exclude CVT
Treatment
- Indications for treatment: Vision loss (emergent tx), headache (therapeutic)
- Weight loss
- Medications
- Acetazolamide (carbonic anhydrase inhibitor) reduces CSF pressure
- Topiramate (partial CAI) reduces CSF pressure
- Surgical
- VP Shunt (vision loss and HA refractory to treatment)
- Optic nerve sheath fenestration
- Venous stenting
3. Temporal Arteritis
Clinical Presentation
- New headache
- Temporal artery tender / decrease pulse
- Jaw/tongue claudication
- Vision change
Diagnosis (need 3/5)
- Age >50
- New headache
- Temporal artery tender / decrease pulse
- ESR > 50
- Biopsy: vasculitis/granuloma
Treatment
- No ischemic organ damage (eg, visual loss) → begin empiric prednisone 40-60mg if medium or high suspicion until ESR or biopsy results return.
- Ischemic organ damage (AION) – Vision loss → Methylprednisolone 1000mg IV daily x 3 days
4. Acute Glaucoma
Clinical Presentation
- Eye pain, Nausea / Vomitus, blurred vision
- Conjunctival hyperemia
- Corneal edema, mid-dilated, non reactive pupil
- Elevated IOP (>20)
Treatment
- Emergent Ophthalmology consultation
- Decrease IOP (intra ocular pressure)
- 0.5% timolol maleate (Timoptic)
- 1% apraclonidine (Iopidine)
- 2% pilocarpine (Isopto Carpine)
- Acetazolamide 500mg IV then 500mg po
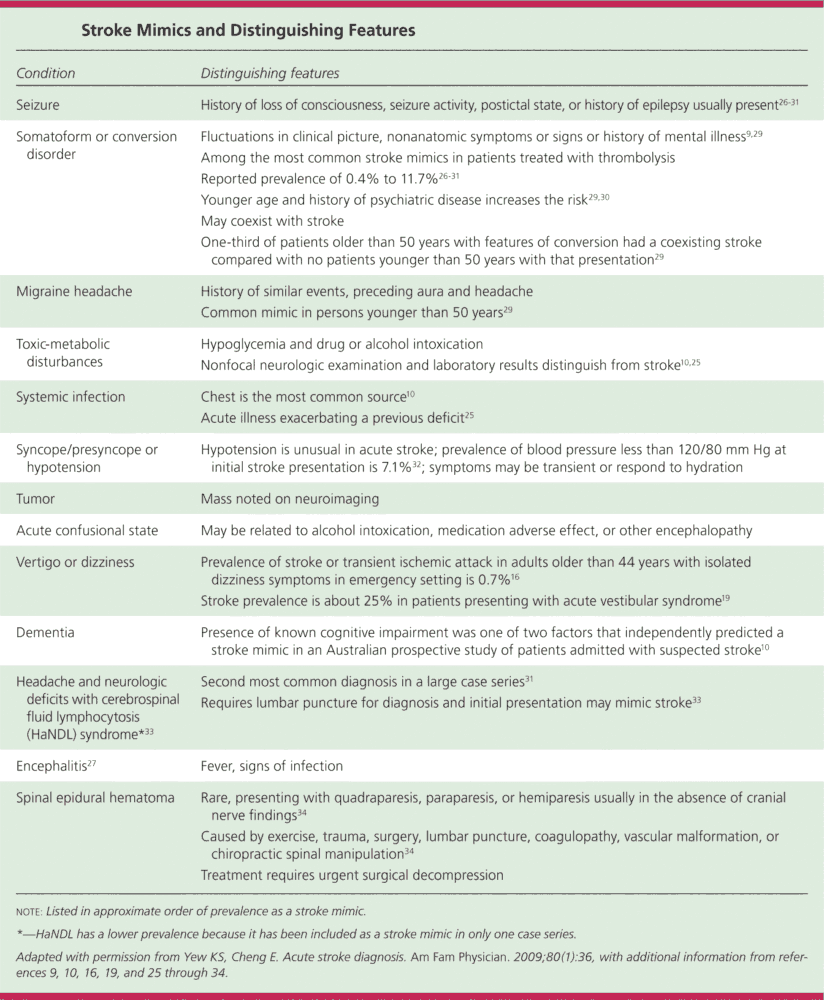
5. Cervical Artery Dissection
General
- Cervical artery dissection = carotid artery dissection + vertebral artery dissection
- Common cause of pediatric strokes (1 in 5)
- Cause:
- Major trauma: penetrating or blunt
- Minor trauma: coughing, whiplash, cervical seatbelt signs, rotational routine neck movement, chiropractor manipulation
Presentation
- Stroke syndromes:
- Carotid artery dissection: MCA (Middle cerebral artery), anterior circulation stroke syndromes (hemiplegia)
- Vertebral artery dissection: posterior fossa symptoms (ataxia, vertigo, dysmetria)
- Wallenberg Syndrome: ipsilateral facial numbness, contalateral body numbness
- Horner’s Syndrome: miosis, ptosis, anhydrosis (vertebral & carotid artery dissection)
- Facial (carotid), neck (vertebral) pain
- SAH like acute onset
- Cranial nerve abnormalities
Diagnosis
- Carotid duplex – poor sensitivity
- CT Angiography
- MRI/MRA
- Angiography
Treatment
- Neurological/Neurosurgery consultation
- Anticoagulation
- Contraindicated if concomitant cerebral hemorrhage
- Used to decrease risk of thrombus formation and embolization
6. Carbon Monoxide Poisoning
History and Physical
- Exposure ?
- Multiple patients / similar location /similar symptoms
- Headache with N/V/ syncope
- Altered mental status
- Cherry-red mucous membranes
- Cerebellar ataxia
Action
- COHb level
- O2 (100% NRM vs HBO)
Urgent Headaches
- Acute Sinusitis
- Obstructive hydrocephalus
- Benign Exertional HA
- Post-Traumatic
- Drug/Food Related
- Cranial Neuralgias
Primary Headaches
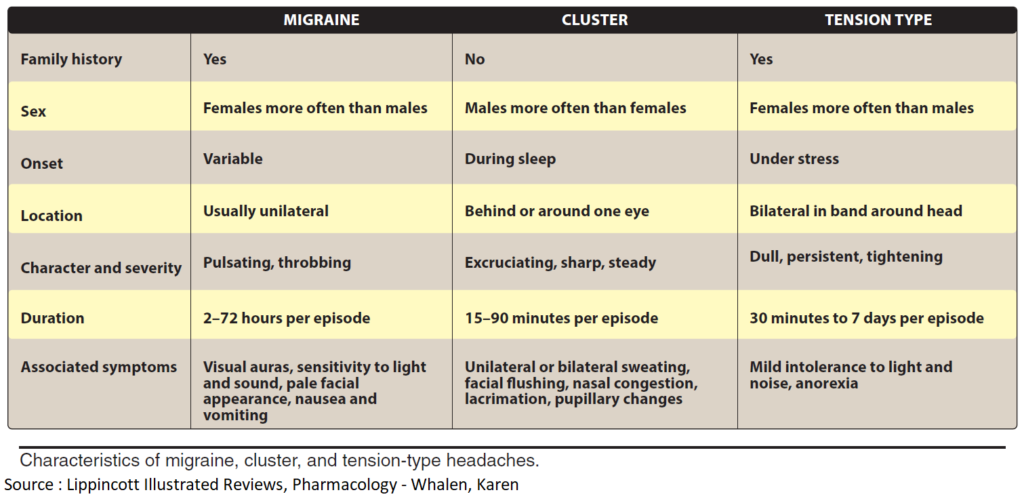
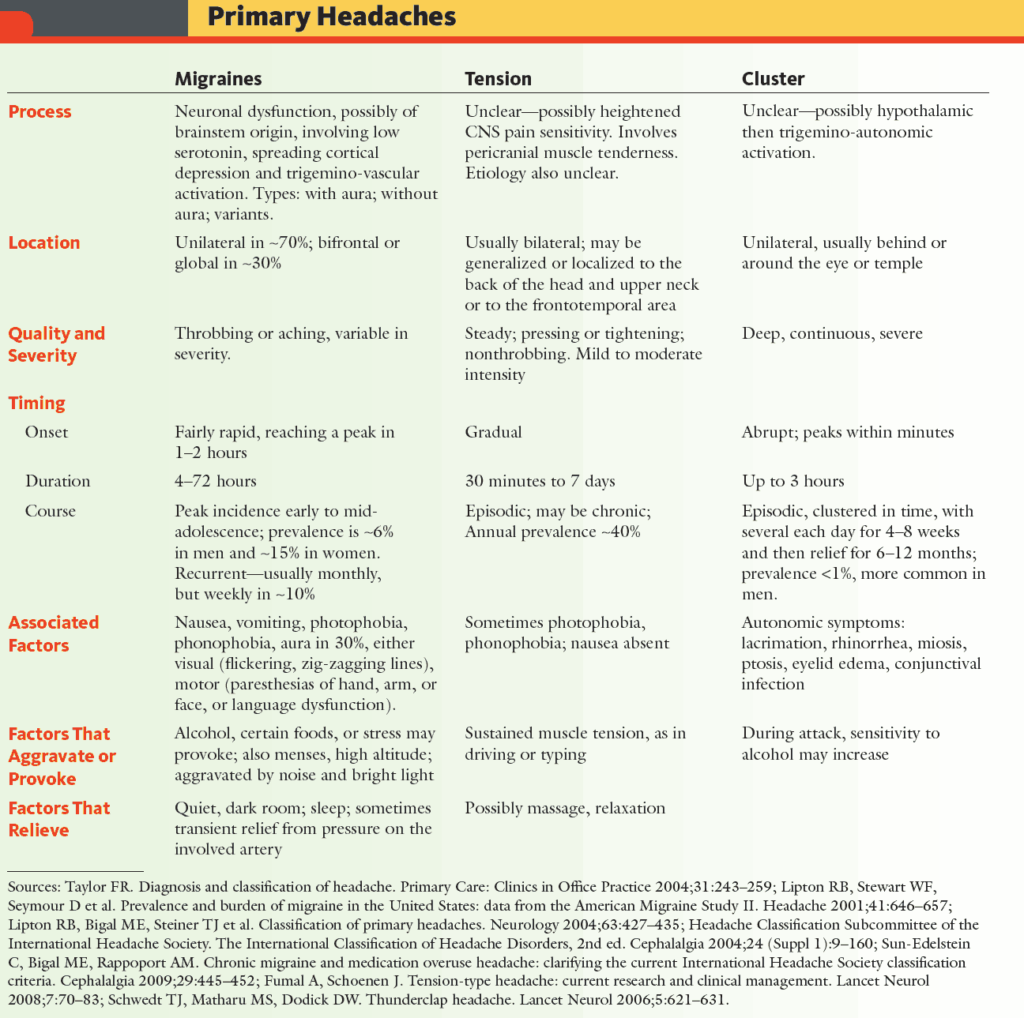
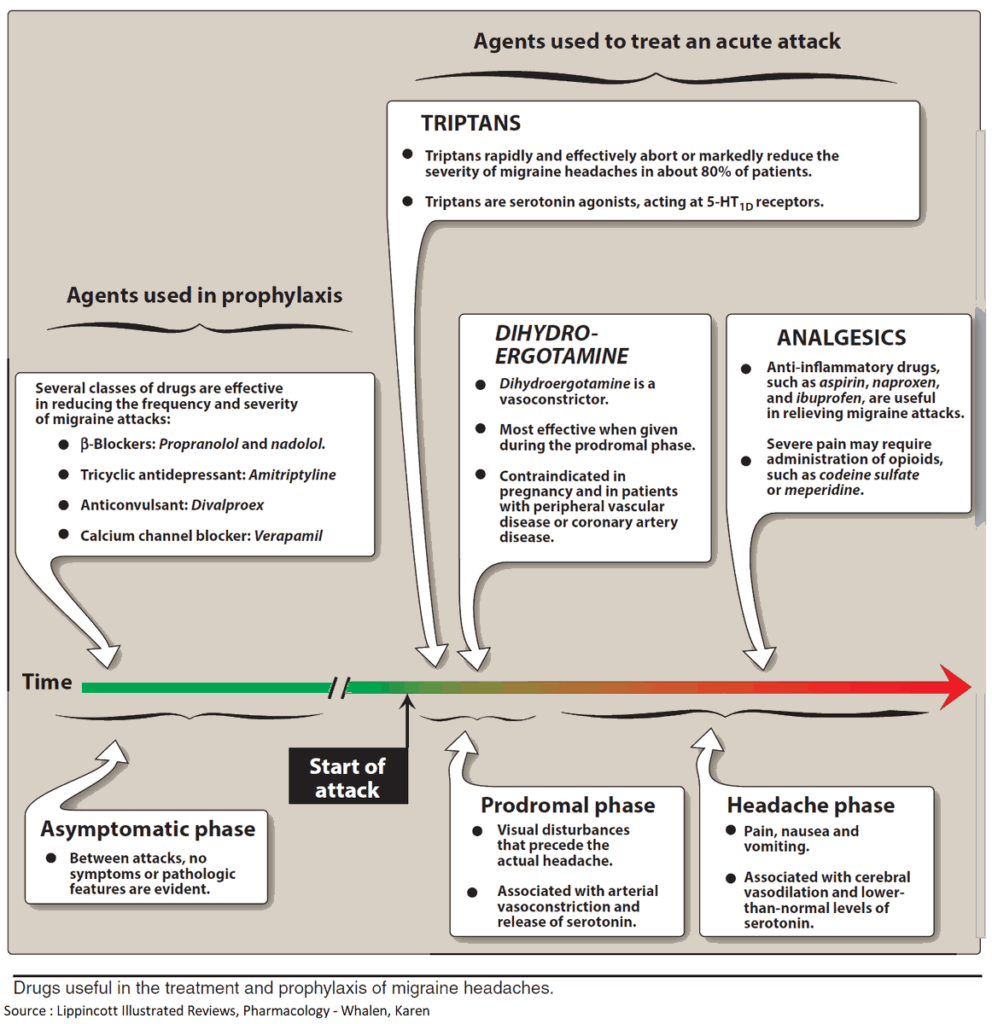
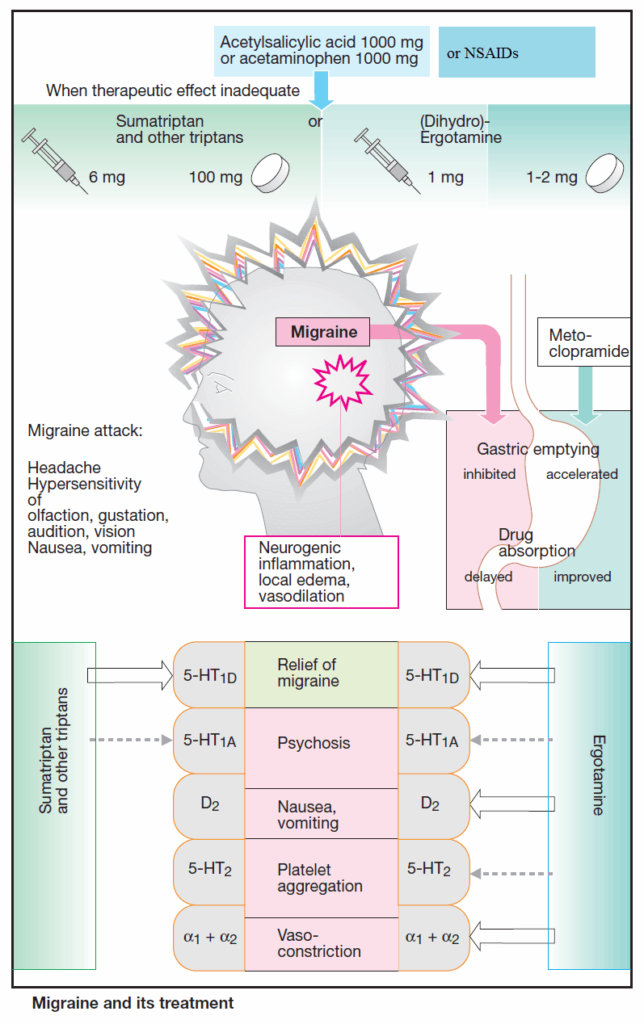
1. Migraine Headache
Presentation
- Common migraine
- Severe, throbbing, unilateral HA
- Photo/Phonophobia
- Hours to days
- Classic migraine
- Preceded by aura
- +/- GI distress
- POUNDing mnemonic
- Pulsating, duration 4-72 hOurs, Unilateral, Nausea, Disabling
- Highly predictive of migraine headache (JAMA 2006;296:1274-83)
Treatment
- IV Dopamine antagonist (Compazine, Reglan)
- IVF (Normal Saline)
- Opiates
- Triptans/NSAIDS
- Dexamethasone
2. Cluster Headache
Presentation
- Middle aged men
- Sudden onset Headache
- Unilateral blur vision / nasal congest / lacrimate / salivate / sweat
- Lasts hours, recur same time of day
- Precipitated by exertion / stress
Treatment
- O2
- Symptomatic relief
- Intranasal lidocaine
- Neurology referral
3. Tension Headache
Presentation
- Frontal/occipital/band-like
- No preceding event
Treatment
- Symptomatic relief (NSAIDS, Tylenol)