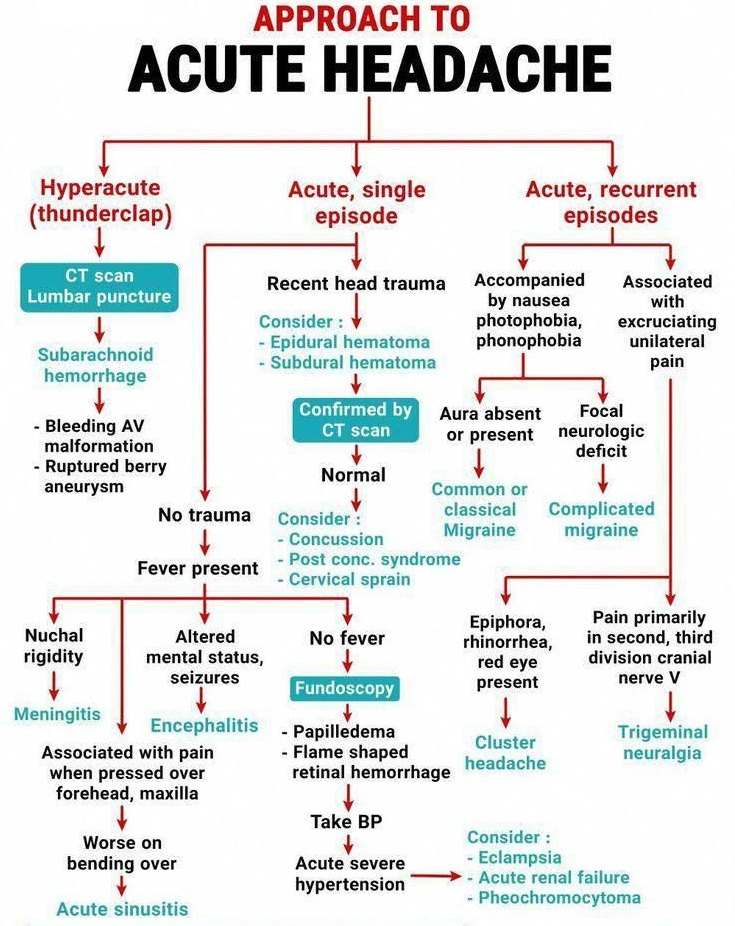
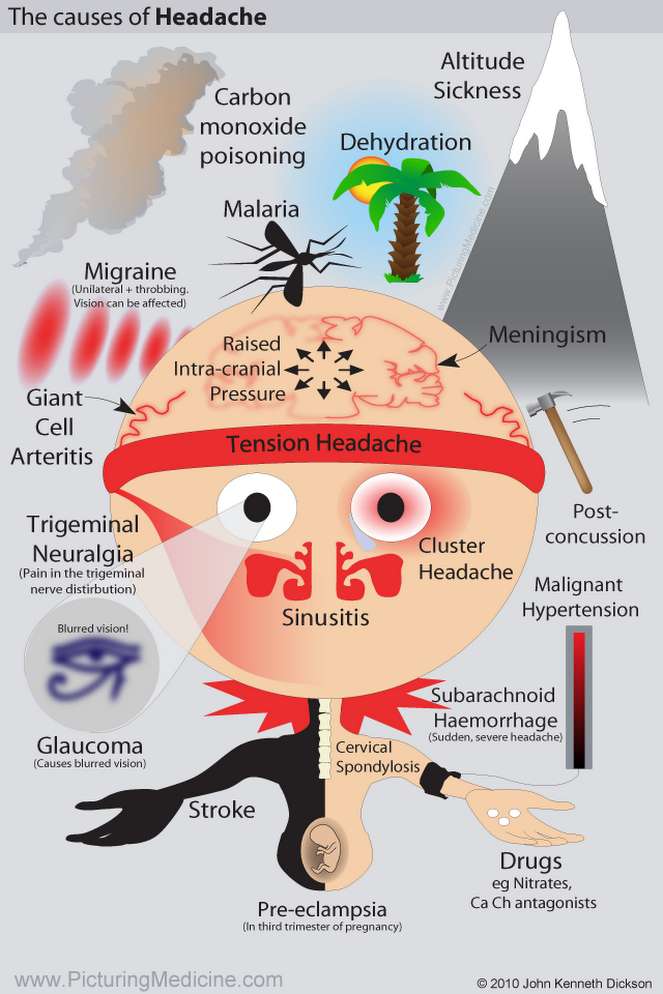
Headache is one of the most common presenting symptoms. There are often few clinical signs, and the history is the main diagnostic tool. Many different pathologic processes can result in headache or facial pain.
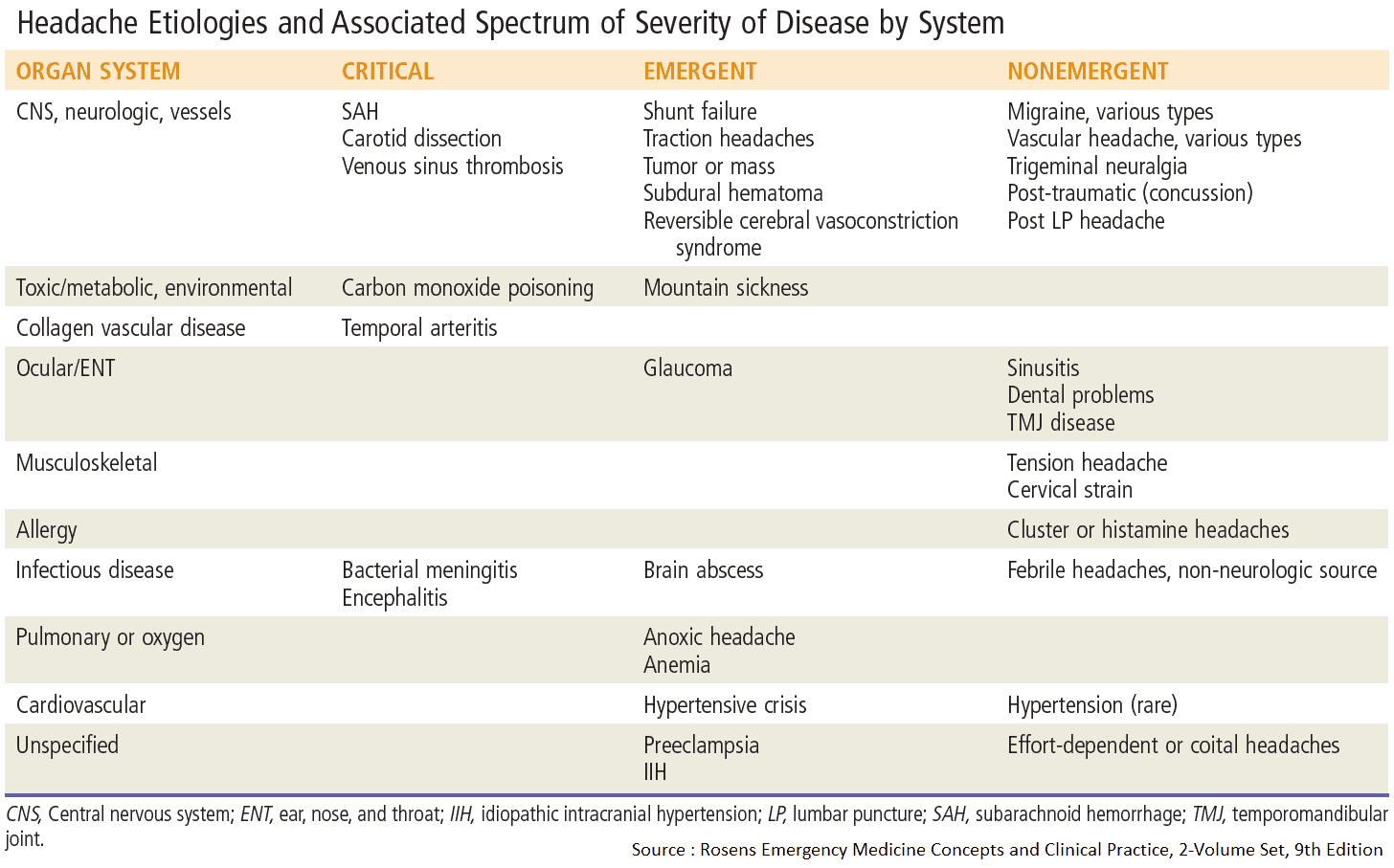
Differential Diagnosis of Headache
- Tension headache.
- Migraine.
- Cluster headache.
- Tumor: primary, secondary.
- Infection: abscess, meningitis, encephalitis, sinusitis, herpes zoster.
- Bleeding: subdural, extradural, intracerebral hematoma, subarachnoid hemorrhage.
- Vasculitic: temporal arteritis.
- Thrombosis: dural sinus thrombosis.
- Skull: fracture, tumor, Paget’s disease.
- Drugs: nitrates.
- Others: benign intracranial hypertension, hydrocephalus, post-traumatic, coital cephalgia, withdrawal from coffee.
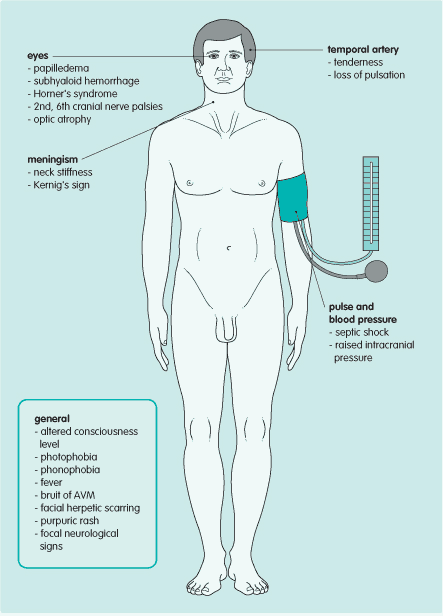
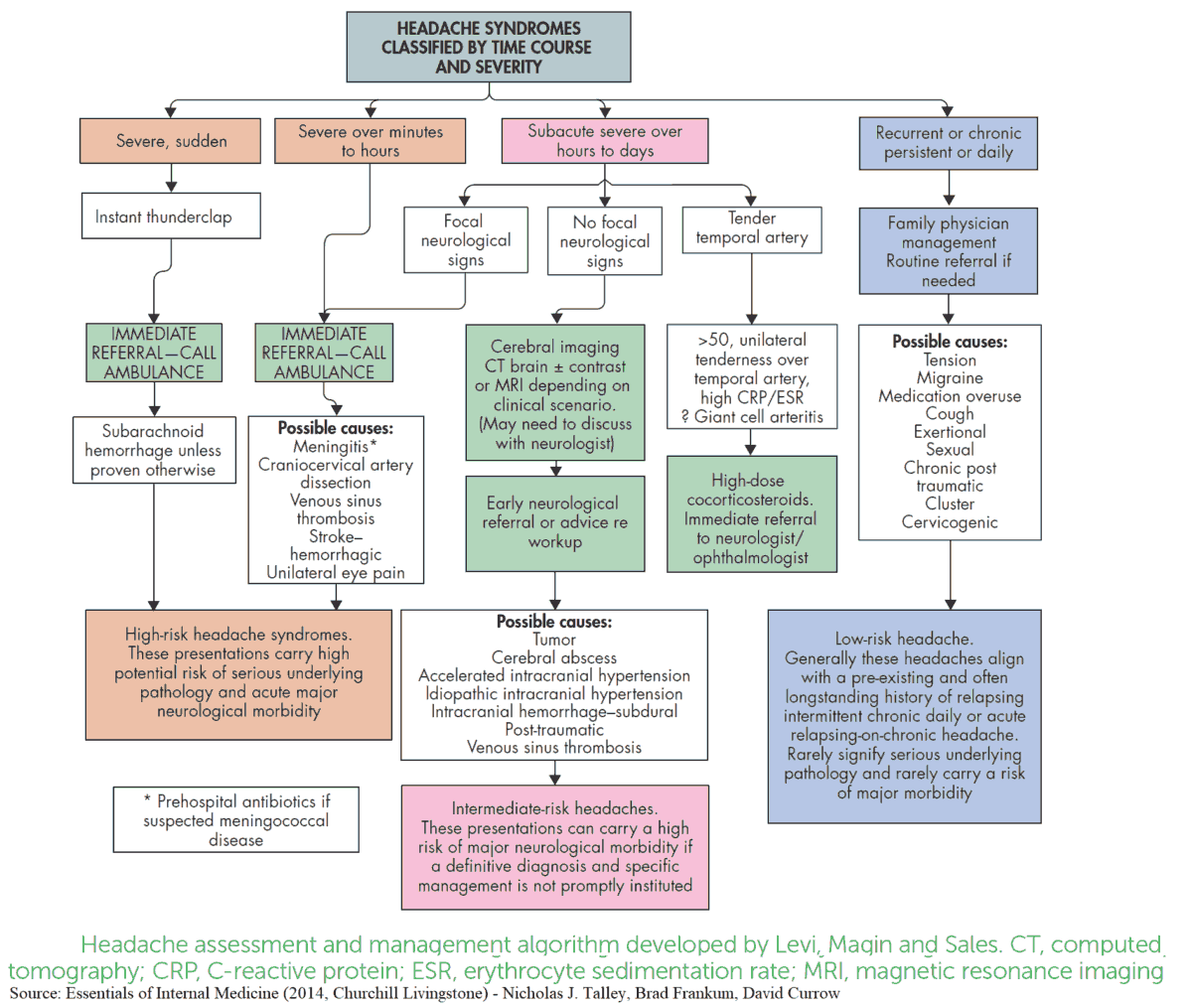
Read Also: Headache Algorithm
Differential Diagnosis of Facial Pain
Diseases affecting the teeth, temporomandibular joint, cervical spine, sinuses, eye, ear, nose, and even heart (myocardial ischemia) can cause pain which radiates to the face. Other causes are disease of the trigeminal nerve such as trigeminal neuralgia and postherpetic neuralgia.
History and Symptoms in the patient with headache or facial pain
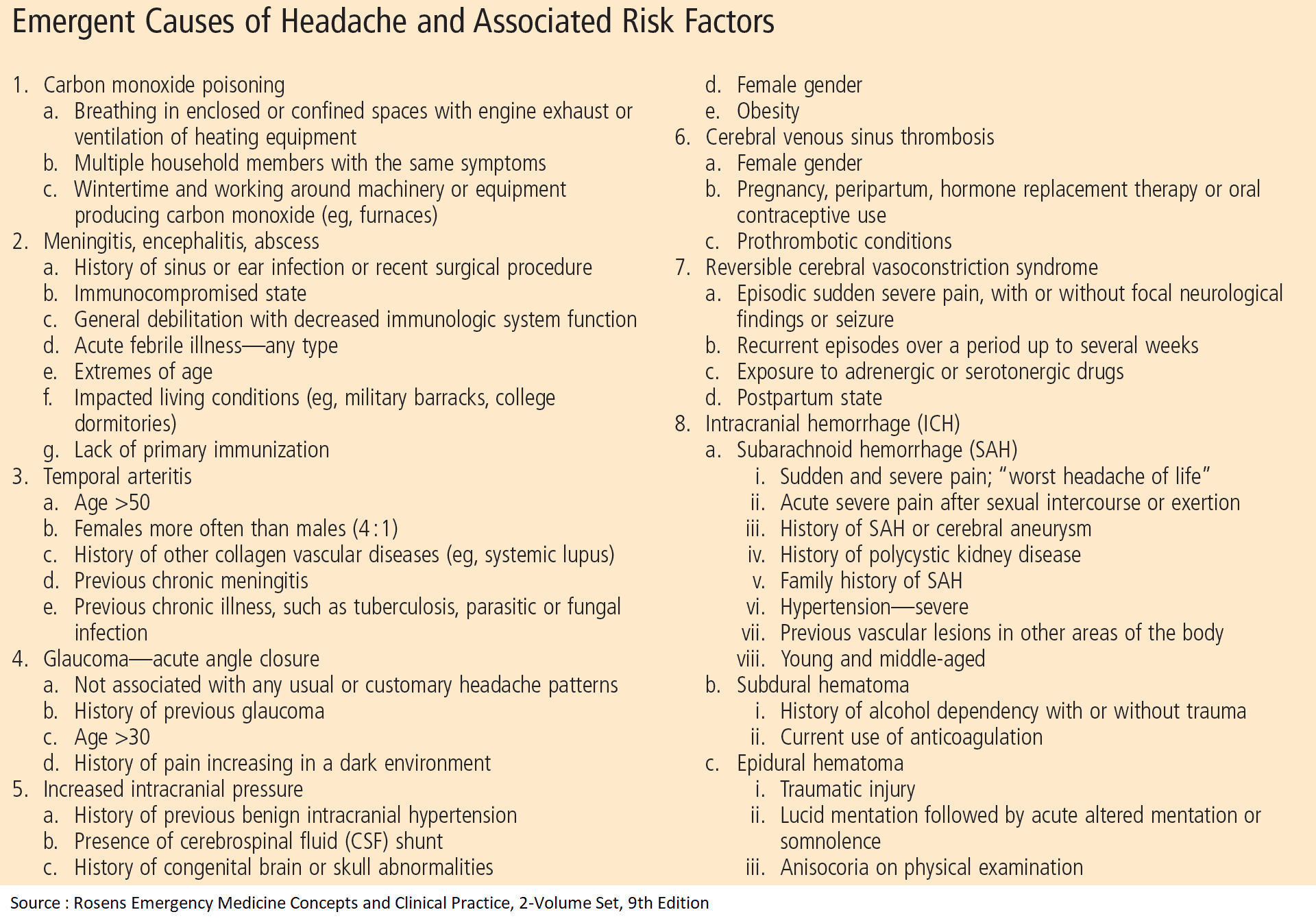
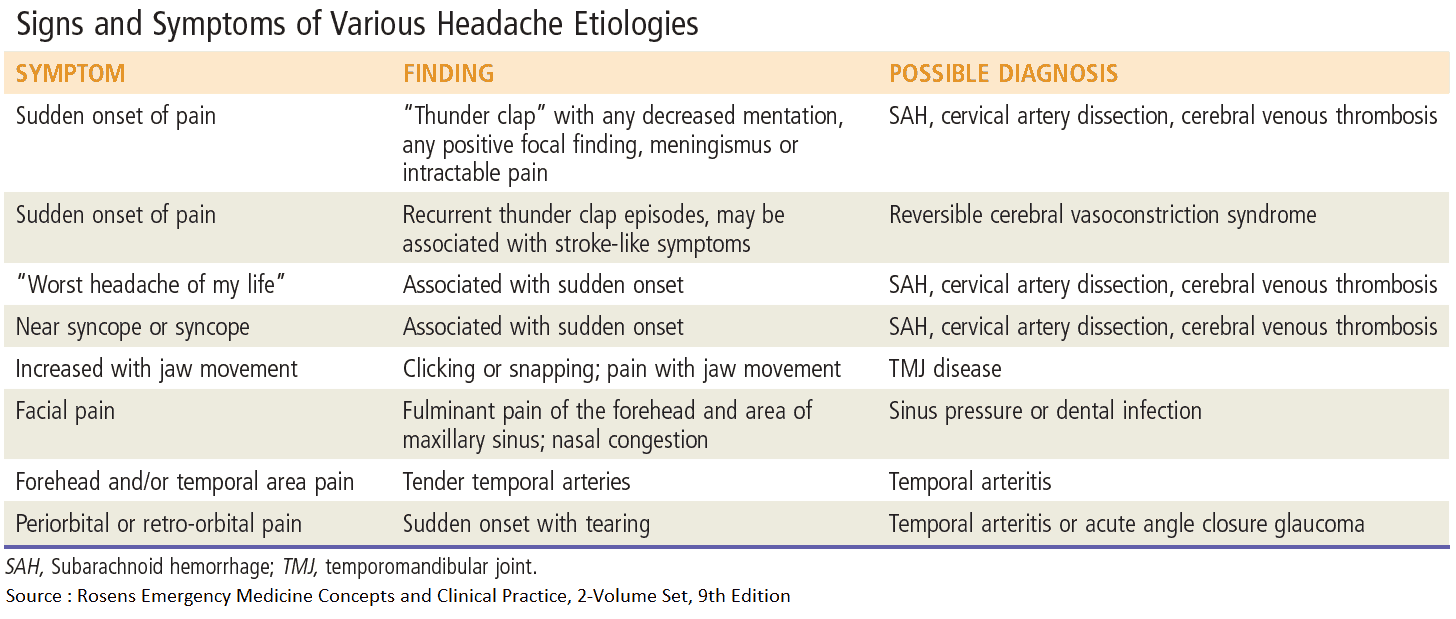
The onset, nature, and subsequent pattern of pain will usually provide a good short list of likely causes. The presence of additional symptoms and risk factors may add further weight to this list. It is important to rule out the most dangerous causes of headache below.
Headache danger signs include:
- acute onset with extreme pain
- headache after strenuous exercise
- the “first” or “worst” headache of the patient’s life
- any signs of increased intracranial pressure
- any associated neurologic deficits (including vision)
- concurrent infection at another site
- association with trauma
Solitary acute episode of Headache
This pattern is seen in :
- Infection (Infective meningitis, cerebral abscess),
- Hemorrhage (Subarachnoid hemorrhage), or
- Thrombosis (Dural venous sinus thrombosis).
(Note that it may also be the first presentation of the other causes of headache).
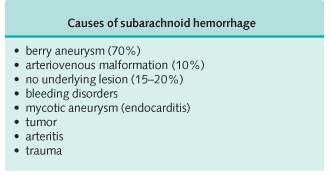
Subarachnoid hemorrhage presents with:
- Sudden onset of severe pain. It may be described as “the worst headache of my life” or “as if someone had hit me on the back of the head.”
- Nausea (from meningeal irritation)
- vomiting (from meningeal irritation)
- neck stiffness (from meningeal irritation)
- photophobia (from meningeal irritation)
- Altered consciousness level and
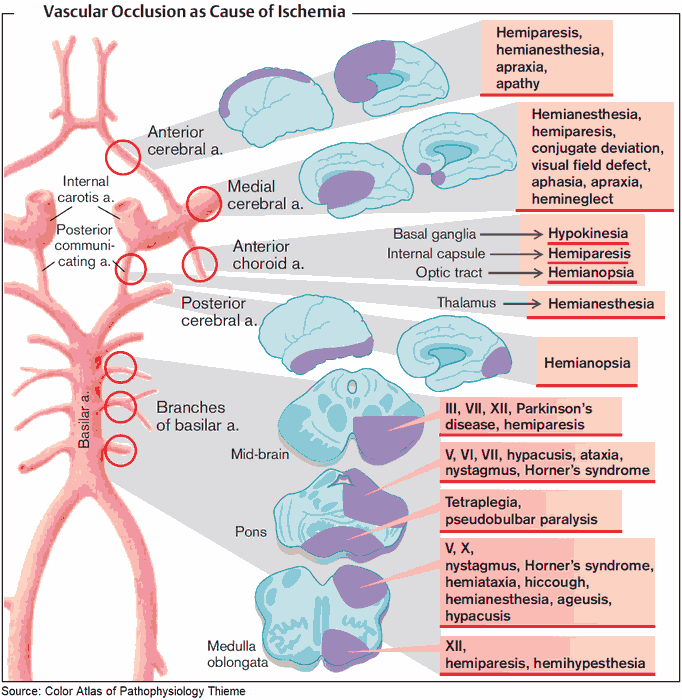
- focal neurologic deficits may also occur depending on the site and size of the bleed.
Infective meningitis presents with:
- short history of headache,
- symptoms of infection (malaise, fever, and rigors)
- symptoms of meningeal irritation (vomiting, photophobia, and neck pain and stiffness).
However, tuberculous and malignant meningitis have a more subacute presentation which can be easily missed.
READ MORE about : Diagnosing and Treating Meningitis
Cerebral abscess causes:
- headaches
- seizures
- symptoms of infection
- symptoms of raised intracranial pressure as the lesion expands.
The infection may have spread from a primary focus, such as the lung in bronchiectasis, middle ear, or paranasal sinuses.
Dural venous sinus thrombosis presents with: seizures, focal neurologic symptoms, and symptoms of raised intracranial pressure can also result from . This is a rare complication of pregnancy, oral contraceptive pill use, dehydration, paranasal sinus infection, and severe intercurrent illness.
Progressive Headache
A headache that comes on gradually over days or weeks and increases in severity is often a feature of a:
- Tumor
- Benign intracranial hypertension
- Hydrocephalus
In all three the headache results from raised intracranial pressure and has the characteristic features shown in Fig. 1.
Temporal arteritis also presents gradually, but the nature of the headache is very different.
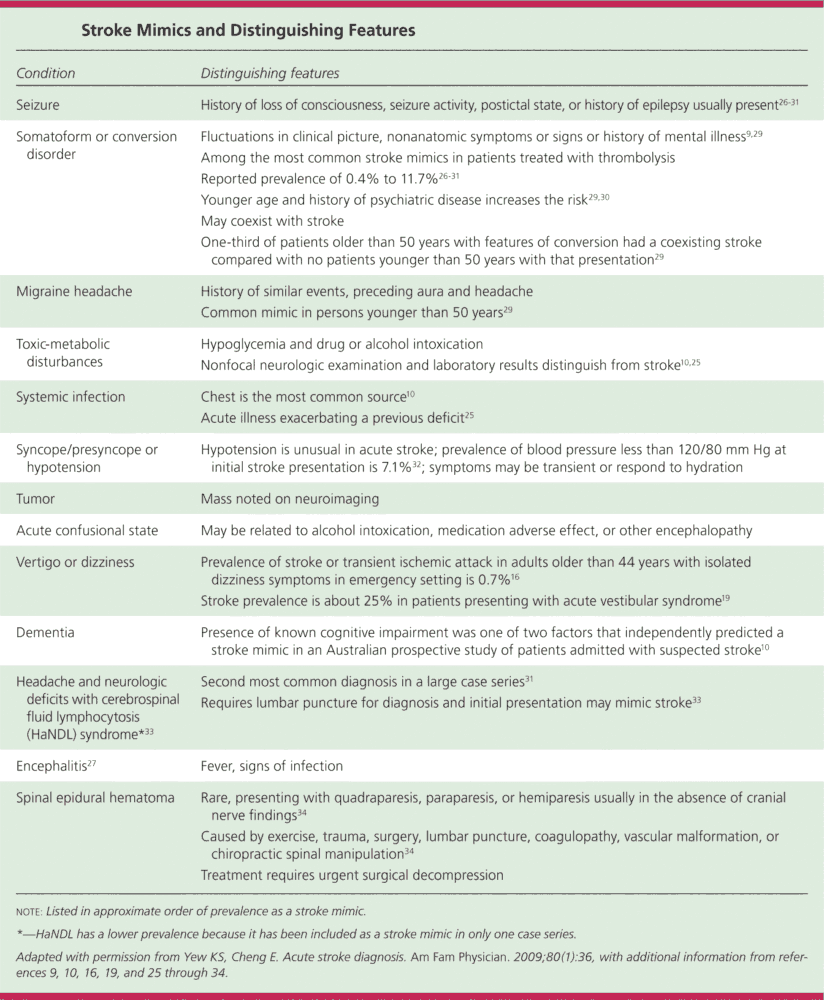
Cerebral tumors can be primary or secondary. The patient may have a history of malignancy elsewhere. The most common tumors to metastasize to the brain are those of the thyroid, bronchus, and breast, as well as gastric, renal and prostate tumors. In addition to headache, the patient may also develop seizures and focal neurologic deficits related to the site of the lesion.
Benign intracranial hypertension (pseudotumor cerebri) is most common in young women. Headache, nausea, and visual disturbance are the presenting symptoms. There is an association with obesity, empty sella turcica, and certain drugs. If left untreated, the patient may become blind due to infarction of the optic nerve.
Temporal arteritis (TA) affects predominantly the elderly. It is extremely rare before the age of 50 years. The patient presents with:
- Superficial headache overlying the temporal arteries. The pain may be exacerbated by brushing or combing the hair
- Jaw claudication may arise as a consequence of inflammation of the branches of the external carotid artery
- Visual loss may be temporary (amaurosis fugax) or permanent if the ciliary or central retinal artery is affected
- Weight loss
- Anorexia
- Fever
- Proximal muscle pain
Treatment with high-dose IV steroids should begin as soon as TA becomes number one on the differential diagnosis. If you plan to get a TA biopsy, the steroids should be started before the procedure because they can be vision-sparing. Consider temporal arteritis in any patient over 50 years old with a headache.
Episodic Headache or Facial Pain
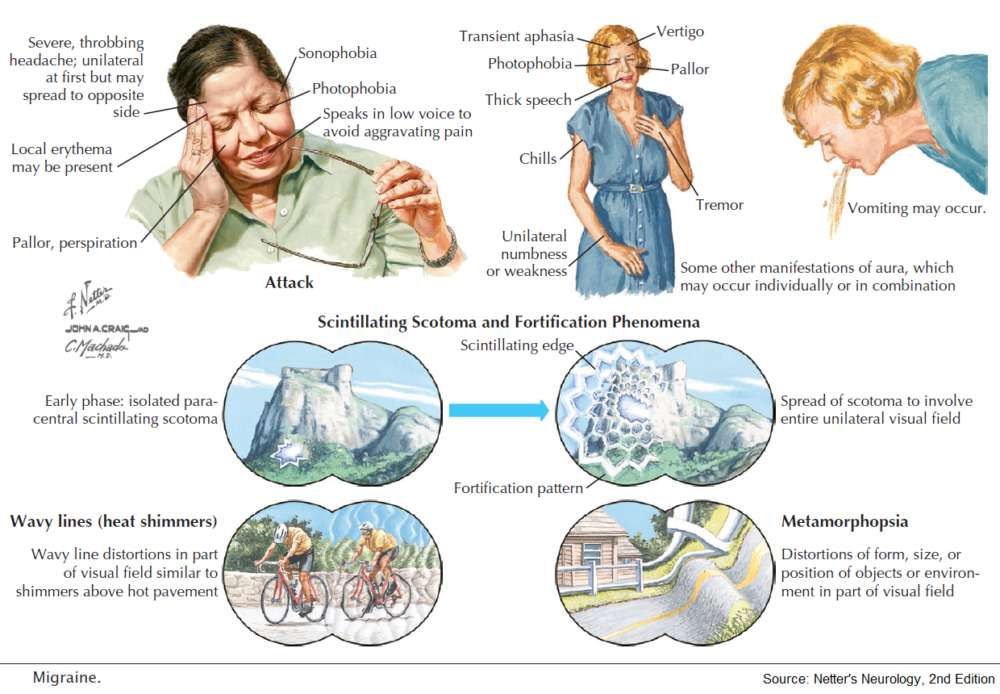
- Migraine
- Cluster headaches
- Trigeminal neuralgia
Migraine and cluster headaches present with episodes of pain (often severe) interspersed with long symptom-free periods. Paroxysms of pain are also a feature of trigeminal neuralgia.
Classic migraine usually starts with a prodrome lasting 5-60 minutes, characterized by a sense of ill health and visual abnormalities (fortification spectra, scotomata, or teichopsia). A throbbing headache then develops, which tends to be unilateral but can become generalized. This is associated with nausea, vomiting, photophobia, and phonophobia. The attack resolves spontaneously after several hours and is often followed by sleep. In uncommon variants of migraine, headache may be accompanied by hemiplegia, ophthalmoplegia, ataxia, vertigo, or unilateral facial palsy. Migraine is more common in women. Provoking factors include menstruation, fatigue, cheese, and red wine.
Cluster headache (migrainous neuralgia) is a severe unilateral pain centered around one eye. The pain lasts for around an hour and occurs daily for several weeks, often waking the patient from sleep. There is ipsilateral nasal congestion, and the eye becomes watery. Horner’s syndrome can develop and is occasionally permanent. Symptom-free periods of many months occur between attacks. Cluster headaches are more common in men and may be precipitated by alcohol.
Trigeminal neuralgia (tic douloureux) is characterized by paroxysms of lancinating pain in the distribution of the 5th cranial nerve. It is stimulated by touching “trigger zones” on the face such as the lips, or by eating or drinking. The pain lasts for up to 1 minute and does not occur during sleep. Spontaneous remissions can last several months. While there is usually no underlying cause, trigeminal neuralgia may occasionally be secondary to multiple sclerosis (MS) in the young patient or to tumors affecting the cerebellopontine angle or 5th cranial nerve.
Chronic Headache or Facial Pain
Persistent pain is a feature of:
- Postherpetic neuralgia
- Post-traumatic headache
- Tension headache
Postherpetic neuralgia, may develop following zoster of the trigeminal nerve (usually the ophthalmic division), with persistent burning pain. Facial scarring is usually apparent, and the pain may disturb sleep. It is uncommon in the young.
Tension headaches are the most common cause of headaches presenting to doctors. The feeling is often described as a “tight band around the head,” being most common in the frontal and occipital regions, or as a “pressure” behind the eyes. It is a constant pain, which tends to be worse toward the end of the day or at times of particular stress. There may be coexistent depression.
Post-traumatic persistent headache may develop following head injury, which may not necessarily be severe, with pain similar to a tension headache. It is associated with poor memory and concentration, dizziness, irritability, and symptoms of depression. The patient may be involved in litigation related to the accident responsible.
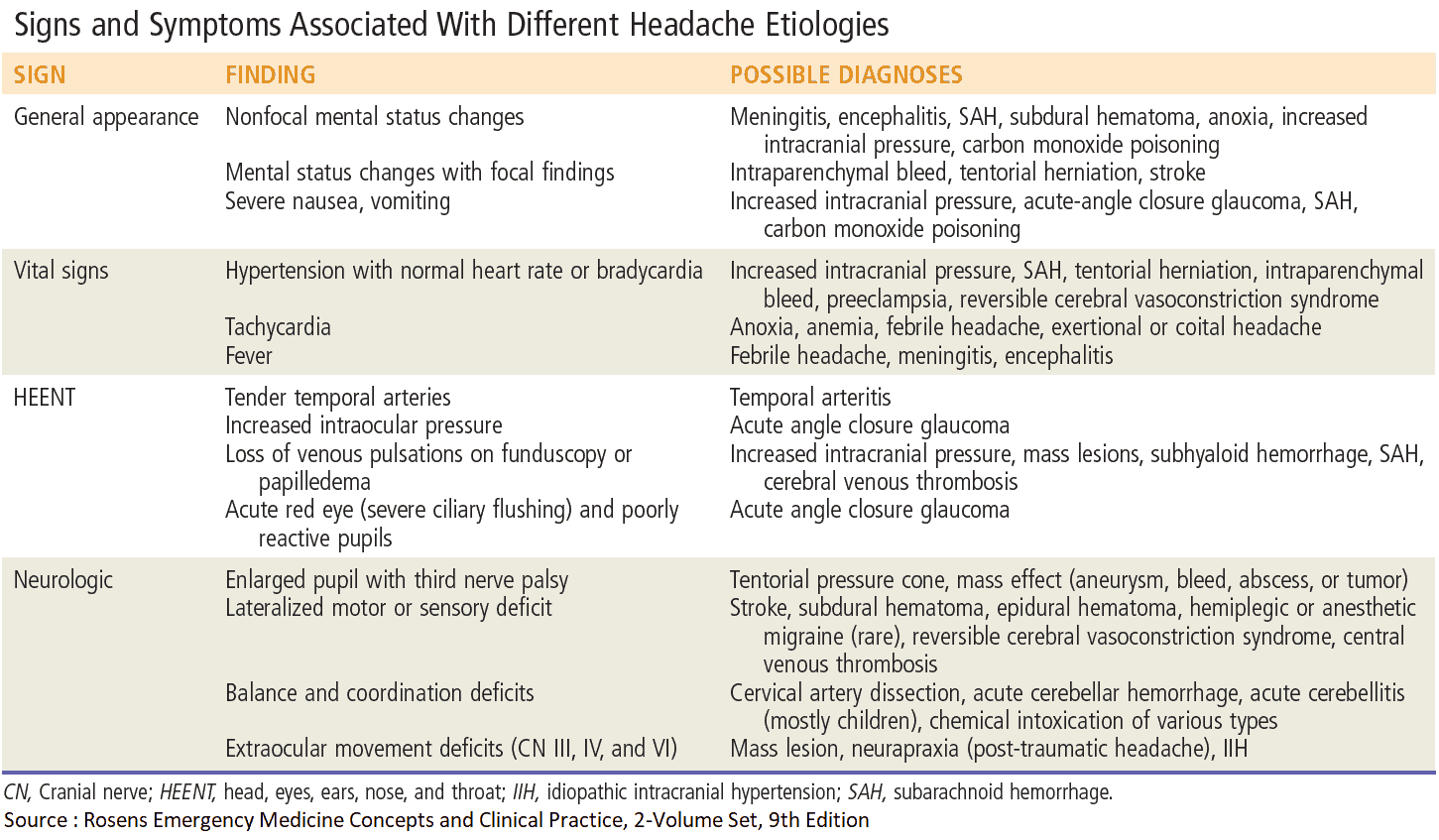
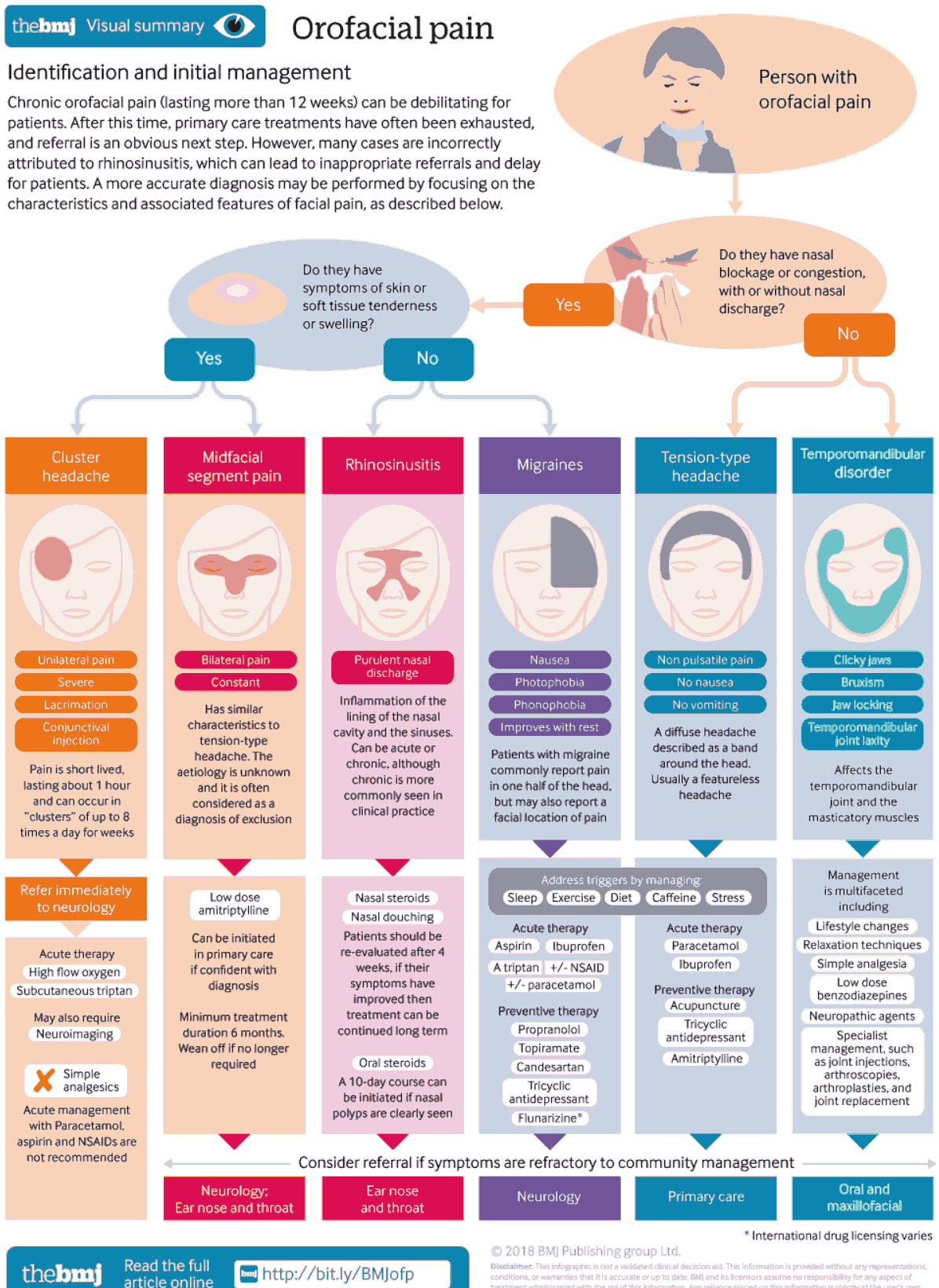
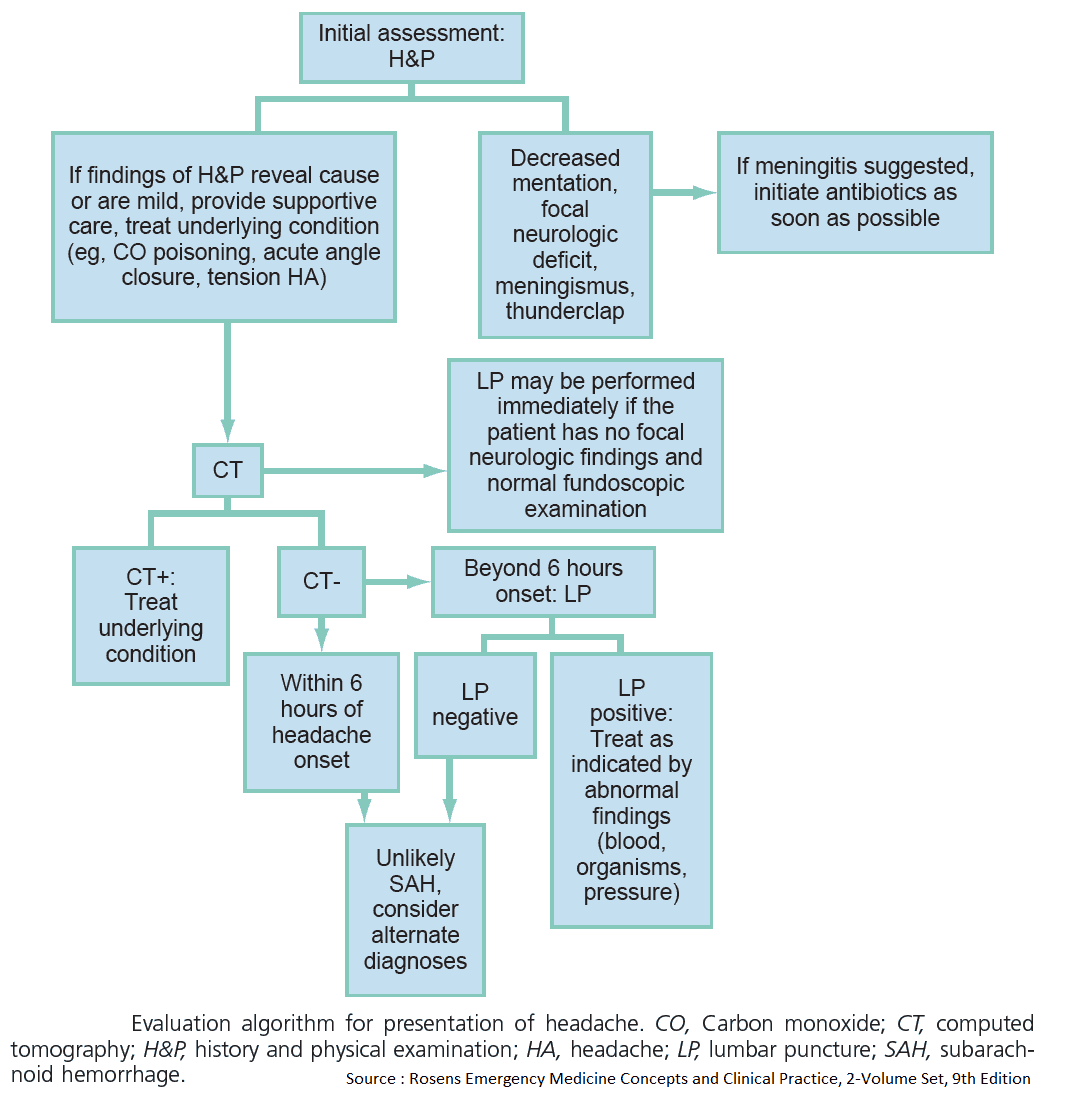
Examination and Signs in the patient with Headache or Facial pain
The diagnosis is often clear from the history. On examination look for evidence of the pathologic processes, such as raised intracranial pressure and meningism. Focal neurologic deficits, if present, help to determine the site of the lesion. Measure blood pressure to rule out hypertensive encephalopathy.
Signs of raised intracranial pressure
- Papilledema: commonly, the only sign
- False localizing sign (ipsilateral, then bilateral 6th cranial nerve palsy)
- Altered level of consciousness, Bradycardia, Hypertension if acute or severe, which can progress to decerebrate posturing and death
Signs of meningism
- Irritability: with a preference for a quiet, darkened room.
- Neck stiffness.
- Positive Kernig’s sign: spasm and pain in hamstrings on knee extension.
- Positive Brudzinski’s sign: neck flexion causes leg flexion.
- Delirium, fever, and petechial rash: may also be present in infectious meningitis.
When meningitis is suspected clinically, treat with antibiotics first and then complete investigations. Patients can die awaiting confirmation of the diagnosis.
If subarachnoid hemorrhage is suspected, look for:
- subhyaloid (retinal) hemorrhage
- bruit of an arteriovenous malformation
- 3rd cranial nerve palsy caused by direct pressure from a posterior communicating artery aneurysm
Signs of temporal arteritis
- Temporal artery tenderness
- Loss of temporal artery pulsation-there may be overlying erythema
- Optic atrophy
- Low-grade fever
Focal neurologic deficit
Focal neurologic signs will help to determine the site of the lesion and may be found in addition to other signs, such as meningism or raised intracranial pressure.
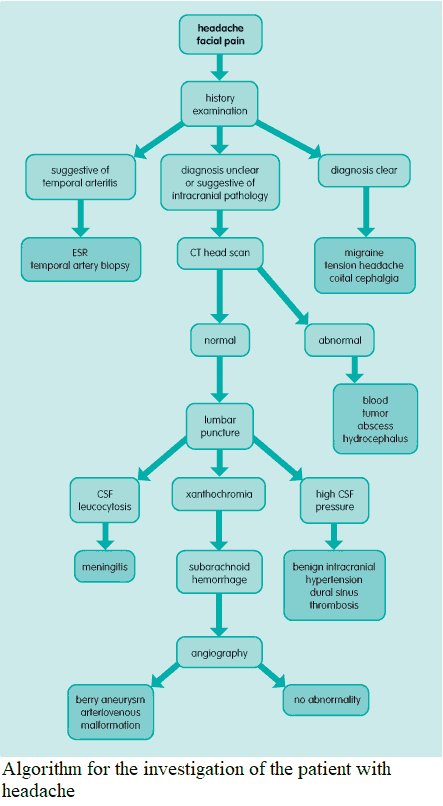
Investigations and Diagnosis of Headache and Facial Pain
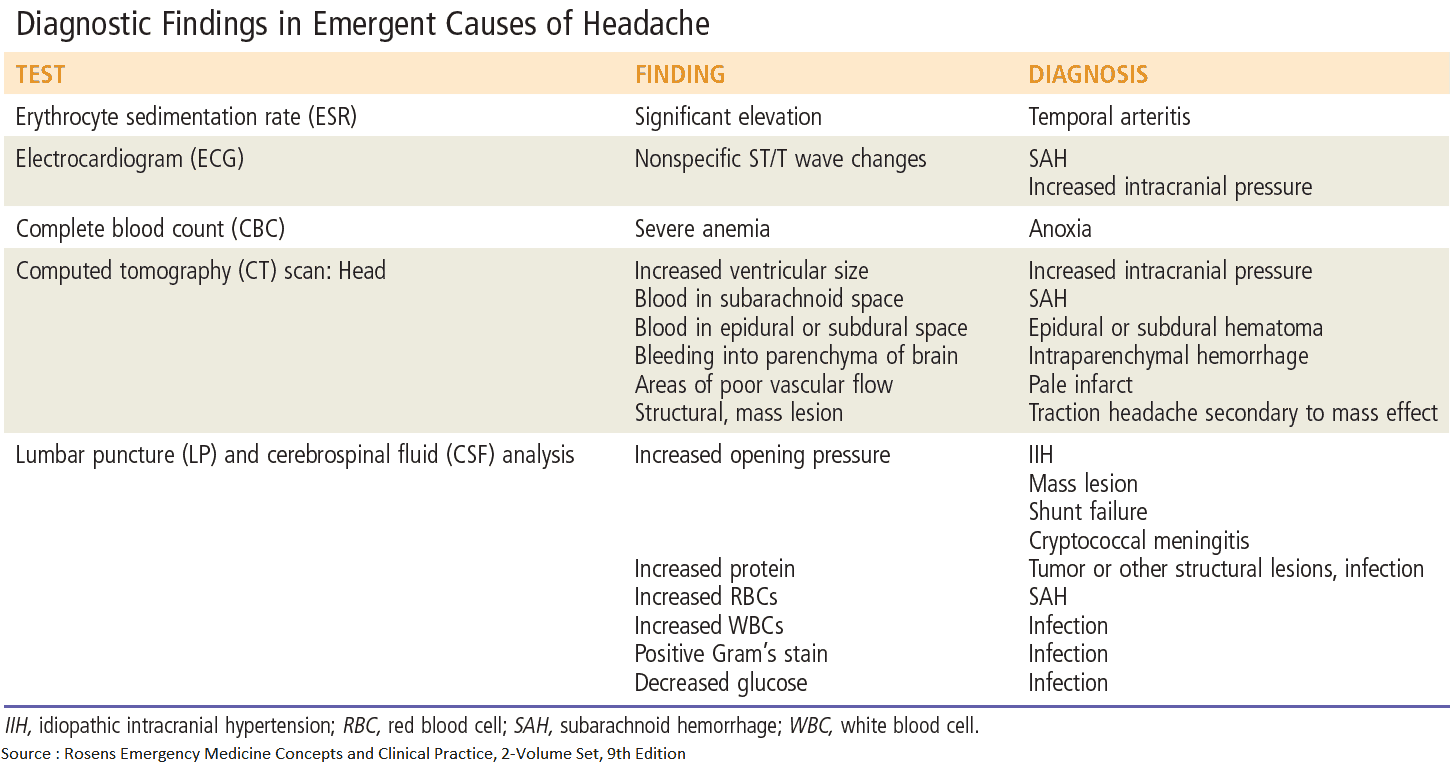
- Complete blood count: normochromic normocytic anemia suggests chronic pathology (e.g., temporal arteritis, tuberculous meningitis); leukocytosis will be seen in infection.
- Erythrocyte sedimentation rate: high in temporal arteritis but may also be raised in infection and malignancy.
- Temporal artery biopsy: temporal arteritis. This is a definitive test, but as there is often patchy vascular involvement, a negative result does not exclude the diagnosis.
- CT scan or MRI imaging of the head: presence of blood, space-occupying lesion (tumor, abscess), or hydrocephalus. Contrast enhancement should be used if tumor is suspected.
- Head CT scan should be done for all cases of trauma, especially in the elderly, patients taking anticoagulants, and patients with mental status changes.
- MRI should be done to look for signs of ischemia. MRA can be done to look for signs of vasculitis.
- Lumbar puncture: this should never be performed when raised intracranial pressure is a possibility, as it causes cerebral herniation. Cerebrospinal fluid (CSF) examination is invaluable in the diagnosis of meningitis. CSF should be sent to the laboratory for assessment of glucose and protein, microscopy, culture, and cytology.
- Cerebral angiography: should be performed if surgery is considered in subarachnoid hemorrhage. It identifies and localizes berry aneurysms and arteriovenous malformations.
- Visual fields: these should be serially measured in patients with benign intracranial hypertension, which carries a serious risk of optic nerve infarction.
- Electroencephalography: herpes simplex encephalitis shows characteristic features.
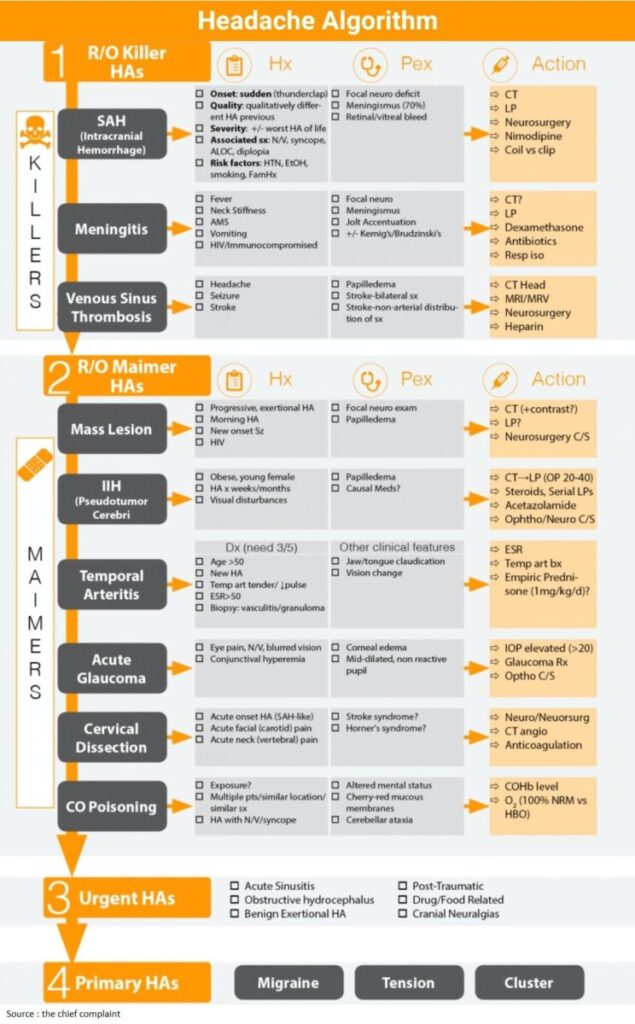
Read Also: Headache Algorithm