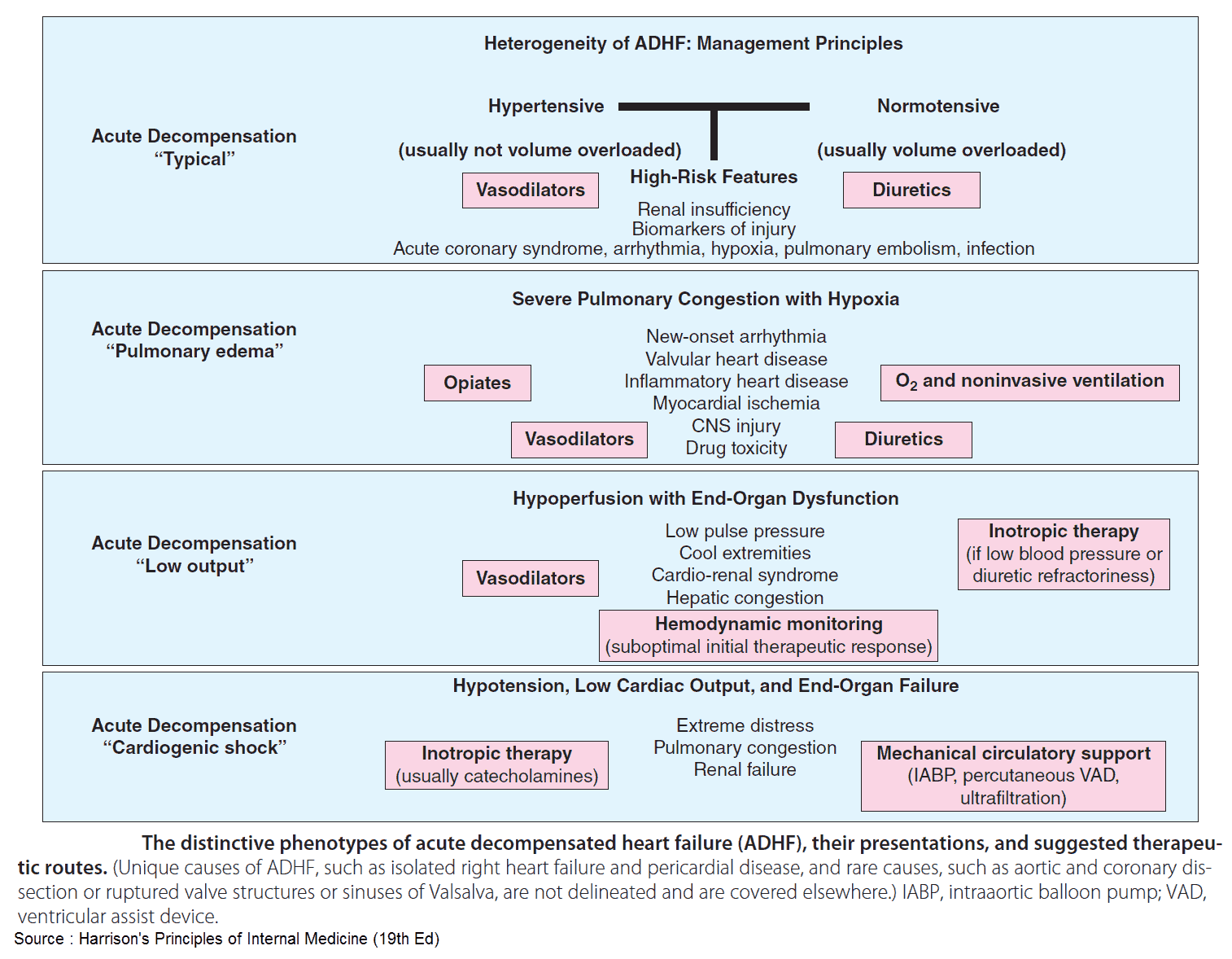
The management of patients with acute decompensated heart failure (ADHF) has historically focused on the administration of diuretic medications.
In fact, the 2013 American Heart Association/American College of Cardiology Foundation Heart Failure Guidelines provide a Class Ia recommendation that “patients with significant fluid overload should initially be treated with loop diuretics given intravenously that should begin in the emergency department without delay.”
In recent years, there are increasing data that support the use of high-dose vasodilator therapy as the initial treatment for patients with ADHF. In 2007, the American College of Emergency Physicians published a clinical policy on ADHF, which emphasized the use of vasodilator therapy in the emergency department (ED) management of patients with ADHF.
Importantly, the majority of ED patients who present with ADHF are not volume overloaded. Rather, their pulmonary congestion is due to volume redistribution.
The classic ED presentation for these patients includes acute dyspnea, hypertension, and pulmonary edema. Often, these patients arrive to the ED by ambulance and receive sublingual nitroglycerin therapy (0.4 mg every 5 minutes) during their transport.
Upon ED arrival, patients should be continued on aggressive vasodilator therapy with nitroglycerin. In most cases, nitroglycerin therapy is started at 50 mcg/min, a dose that is less than what the patient received via the sublingual route with paramedics (80 mcg/min).
Numerous studies have demonstrated the importance of initiating a nitroglycerin infusion at a dose of 120 to 200 mcg/min. A report in the American Journal of Cardiology noted that at least 120 mcg/min of nitroglycerin is required to produce a significant decrease in pulmonary capillary wedge pressure.
The nitroglycerin infusion can be rapidly increased to 400 mcg/min based upon clinical effect and patient symptoms. Though there have yet to be conclusive data that aggressive vasodilator use improves long-term mortality, it has been shown to prevent intubation and mechanical ventilation in this patient population.
The concomitant use of noninvasive ventilation (NIV) and high-dose vasodilator has been shown to decrease intubation rates, intensive care unit admissions, and hospital length of stay for patients with ADHF. NIV should be initiated early in ED patients with ADHF.
Once the patient improves (decreased respiratory rate, decreased dyspnea, improved oxygenation, improved blood pressure), diuretic therapy can be considered.
Importantly, diuretics require adequate renal perfusion in order to be effective. During the initial ED evaluation and management when patients are in extremis, renal perfusion is poor, and diuretics are ineffective.
Though diuretic therapy is eventually needed in all heart failure patients, they are not beneficial in the initial resuscitation period. High-dose vasodilator therapy and NIV should be the initial tenets of the ED management of patients with AHDF.
Key Points
- Diuretics should not be considered first-line therapy in the ED treatment of patients with ADHF.
- High-dose nitroglycerin therapy should be initiated early in ADHF, especially in patients who are hypertensive.
- Do not begin a nitroglycerin infusion at a dose less than that provided by the sublingual route.
- Nitroglycerin doses of at least 120 mcg/min are needed to reduce capillary wedge pressure.
- NIV should be administered early and in conjunction with high-dose vasodilator therapy for patients with AHDF.
Suggested Readings
- Collins SP, Storrow AB, Levy PD, et al. Early management of patients with acute heart failure: State of the art and future directions—A consensus document from the SAEM/HFSA acute heart failure working group. Acad Emerg Med. 2015;22(1):94–112.
- den Uil CA, Brugts JJ. Impact of intravenous nitroglycerin in the management of acute decompensated heart failure. Curr Heart Fail Rep. 2015;12(1):87–93.
- Elkayam U, Bitar F, Akhter MW, et al. Intravenous nitroglycerin in the treatment of decompensated heart failure: Potential benefits and limitations. J Cardiovasc Pharmacol Ther. 2004;9(4):227–241.
- Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: A feasibility and outcome analysis. Ann Emerg Med. 2007;50(2):144–152.
- Sharon A, Shpirer I, Kaluski E, et al. High-dose intravenous isosorbide-dinitrate is safer and better than Bi-PAP ventilation combined with conventional treatment for severe pulmonary edema. J Am Coll Cardiol. 2000;36(3):832–837.