This article is an answer to the ECG Case 170
There is a regular rhythm at a rate of 80 bpm. There is a P wave (*) before each QRS complex, with a stable PR interval (0.14 sec). The P wave is positive in leads I, II, aVF, and V4-V6. This is a normal sinus rhythm. The P wave is broad in leads II and aVF and notched in leads V2-V4, suggesting left atrial hypertrophy.
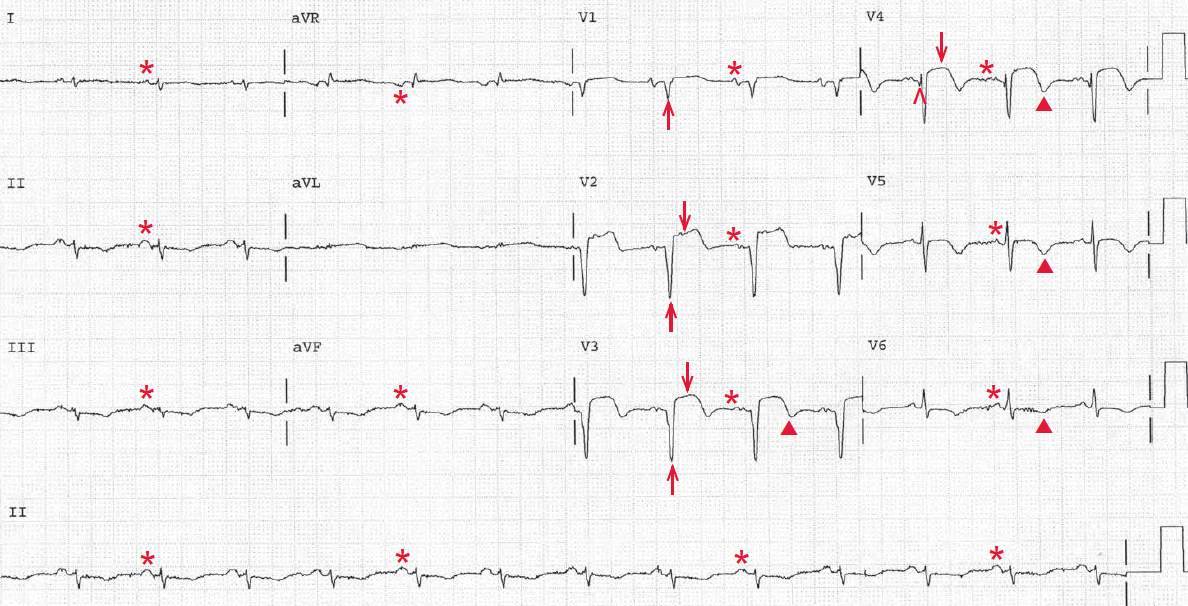
The QRS complex duration is normal (0.08 sec). There is low voltage in the limb leads (defined as a QRS complex amplitude ≤ 5 mm in each lead). The QRS is extremely leftward, between -30 and -90 (positive QRS complex in lead I and negative QRS complex in leads II and aVF). As there are no Q waves in leads II, III, or aVF, indicating an old inferior wall myocardial infarction (MI) accounting for the left axis deviation, this is a left anterior fascicular block. The QT/QTc intervals are prolonged (420/480 msec).
There is a QS complex (↑) in leads V1-V3 and an initial Q wave in lead V4 (^), diagnostic for an MI involving the left ventricular septum and apex. The ST segments are still elevated (↓), and the T waves (▲) are inverted. Based on the patient’s history of an MI 18 months earlier, the ST-segment elevation, which is persistent, represents an old MI and development of an apical left ventricular aneurysm.
However, without this history it would be unclear whether the ST-segment elevation was persistent and the result of an aneurysm or had recently occurred in the setting of an acute MI and hence represents evolution of the ECG changes.
A left ventricular aneurysm is a complication of ST-segment elevation (transmural) MI (STEMI), which results from a thin and dyskinetic region of myocardium in the distribution of a prior MI. Left ventricular aneurysms are associated with mural thrombus formation and systemic cardio-embolization (when they develop early in the setting of an acute MI), re-entrant ventricular arrhythmia, and heart failure.
Patients are treated with anticoagulation with warfarin for 3 months after an acute MI if thrombus is seen. Some physicians will anticoagulate patients with a left ventricular aneurysm even in the absence of thrombus to minimize the risk for thrombus formation that occurs as a result of the acute inflammation of the myocardium. Occasionally, surgery (aneurysmectomy) is necessary when symptoms of recurrent embolization, heart failure, or intractable arrhythmias develop.
A true left ventricular aneurysm should be distinguished from a pseudo-aneurysm, both of which can arise as sequelae of MI. A pseudoaneurysm is a contained myocardial rupture in which the outer layer of the outpouching is comprised of adherent pericardium rather than myocardium. Pseudo-aneurysms are at risk for rupture and often require surgical resection.