Table of Contents
Hypothyroidism results from deficiency of thyroxine (T4) or tri-iodothyronine (T3). The prevalence is 15 in 1000 females and 1 in 1000 males.
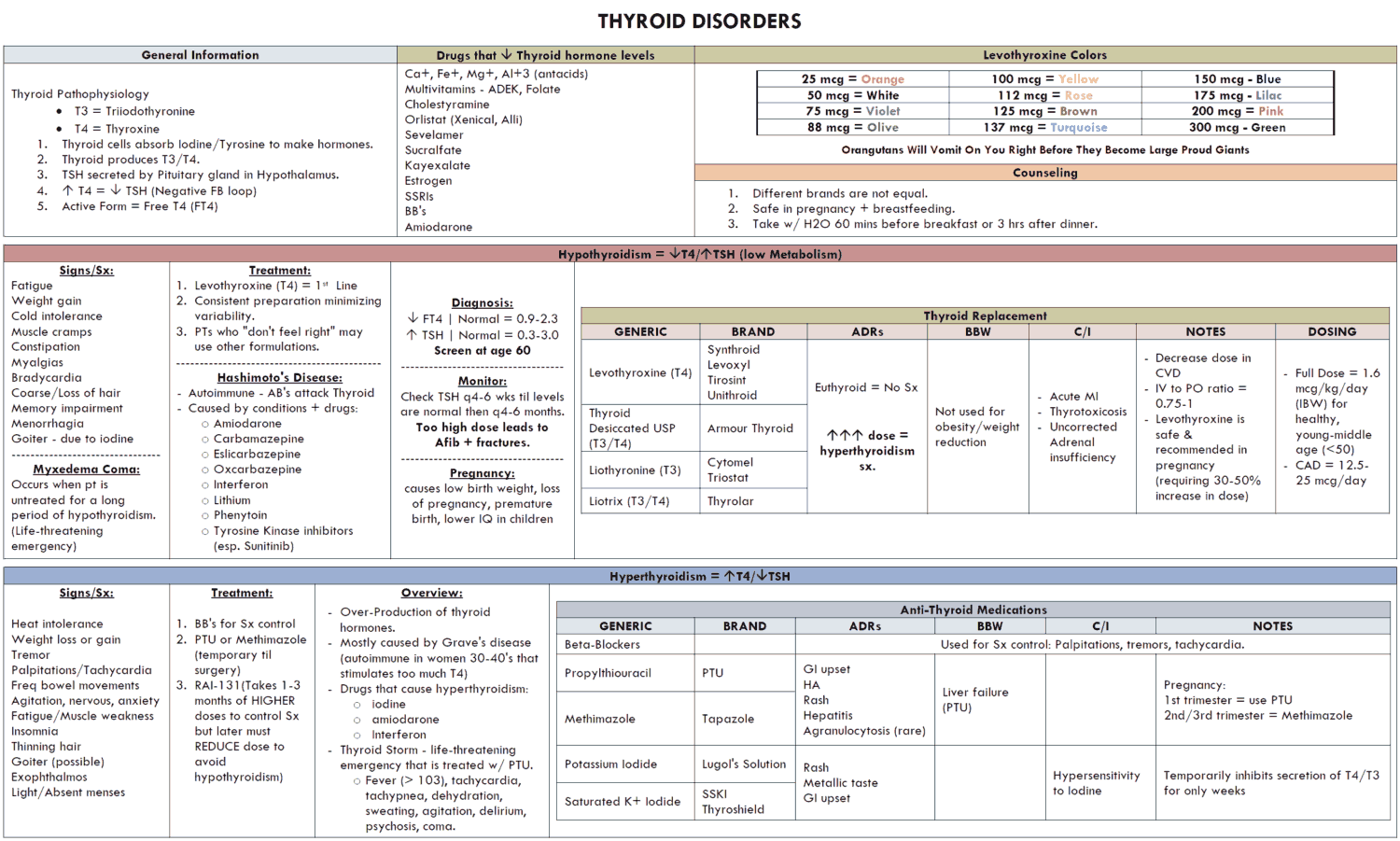
Etiology of Hypothyroidism
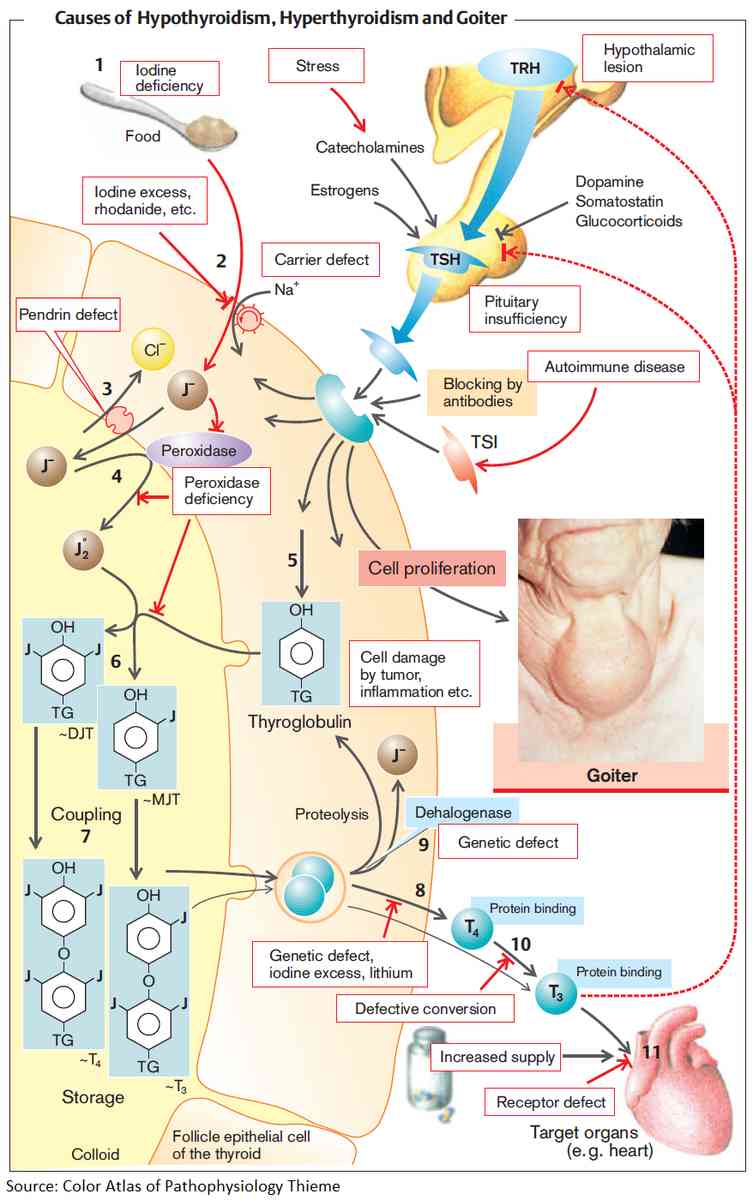
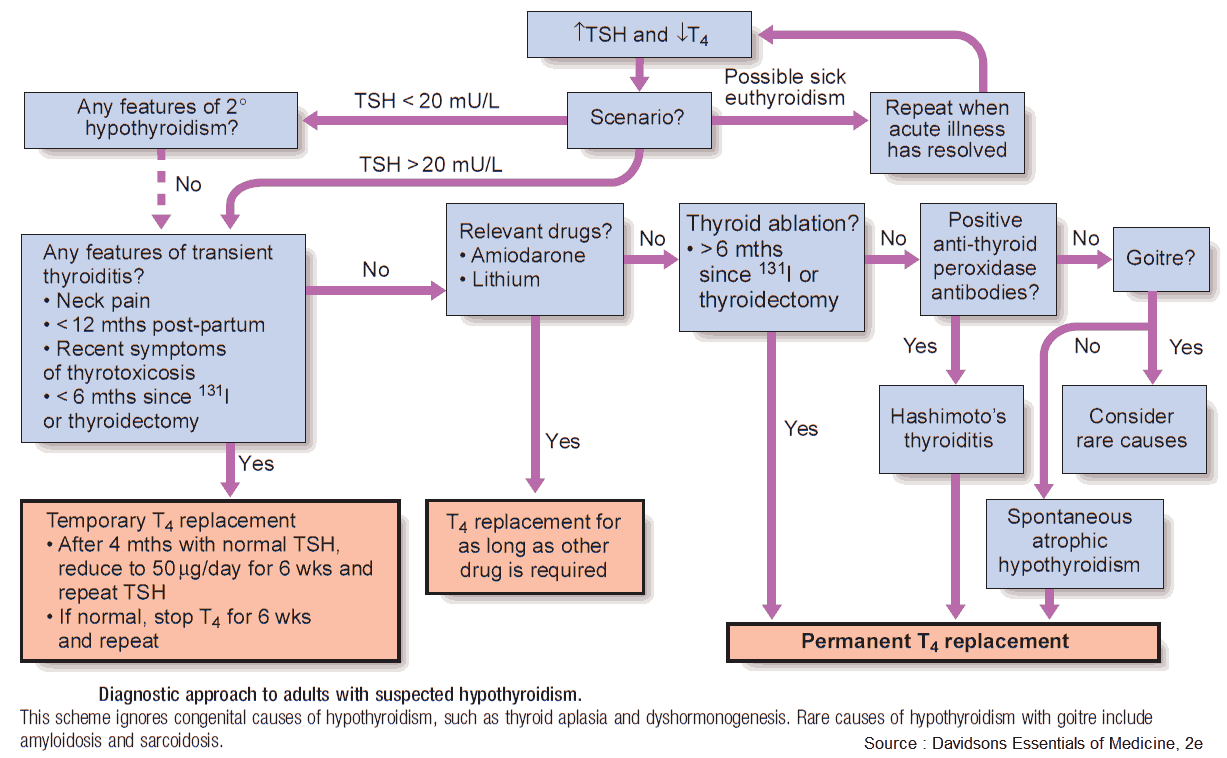
Primary thyroid failure may take the following forms:
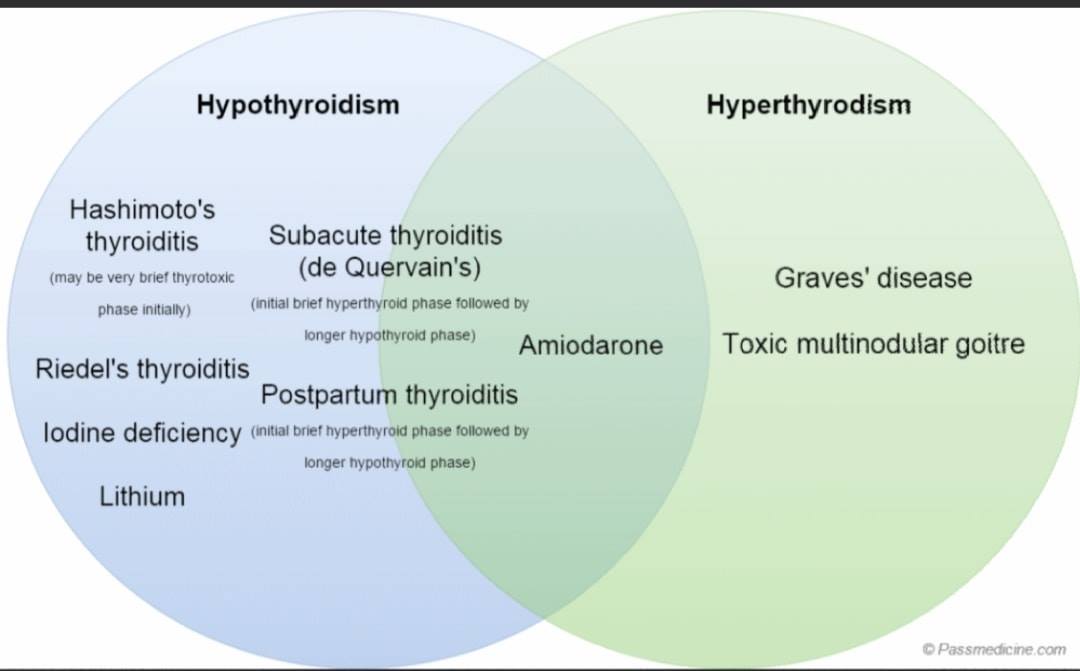
- Autoimmune (Hashimoto’s thyroiditis): this is 15 times more common in women than men and tends to affect the middle-aged and elderly. Patients may present with a firm, nontender goiter, hypothyroidism, or both. It is associated with vitiligo, pernicious anemia, IDDM, Addison’s disease, and premature ovarian failure.
- Idiopathic atrophic hypothyroidism: incidence increases with age and is 10 times more common in women than men. The etiology is probably autoimmune. Previous treatment for hypothyroidism: operative or radioiodine.
- Congenital hypothyroidism: the prevalence in the U.S. is 1 in 4000 infants. It is diagnosed in the first week of life by routine screening, measuring TSH or T4. It is usually due to thyroid agenesis or dyshormonogenesis, which are both due to autosomal recessively inherited enzyme defects. The most common is Pendred’s syndrome, characterized by congenital hypothyroidism, goiter, and nerve deafness in homozygotes.
- Iodine-deficient hypothyroidism: this is a major cause of hypothyroidism and goiter worldwide, although most iodine-deficient people are euthyroid, even though they have a goiter.
- Iatrogenic hypothyroidism: long-term iodine therapy, for example in expectorants, may result in hypothyroidism. Other drugs include amiodarone and lithium carbonate.
Secondary thyroid failure is caused by diseases of the hypothalamus or pituitary. These are very rare.
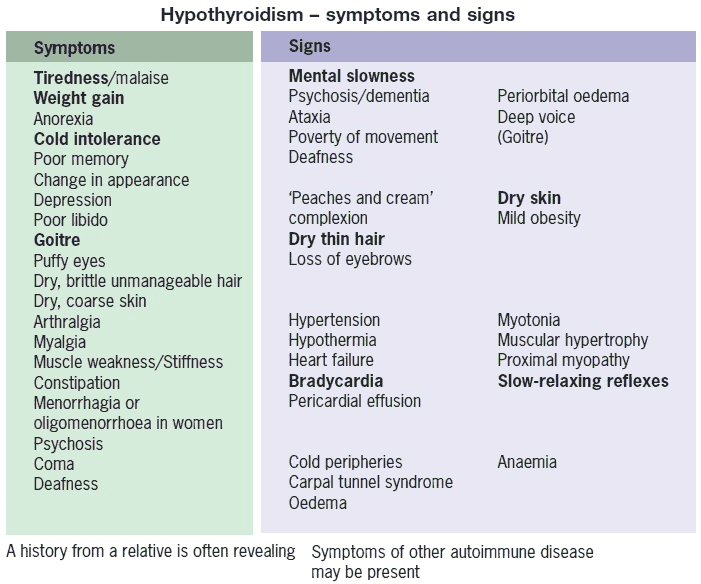
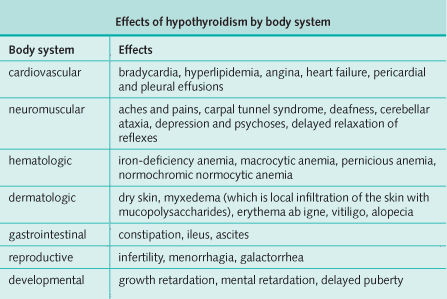
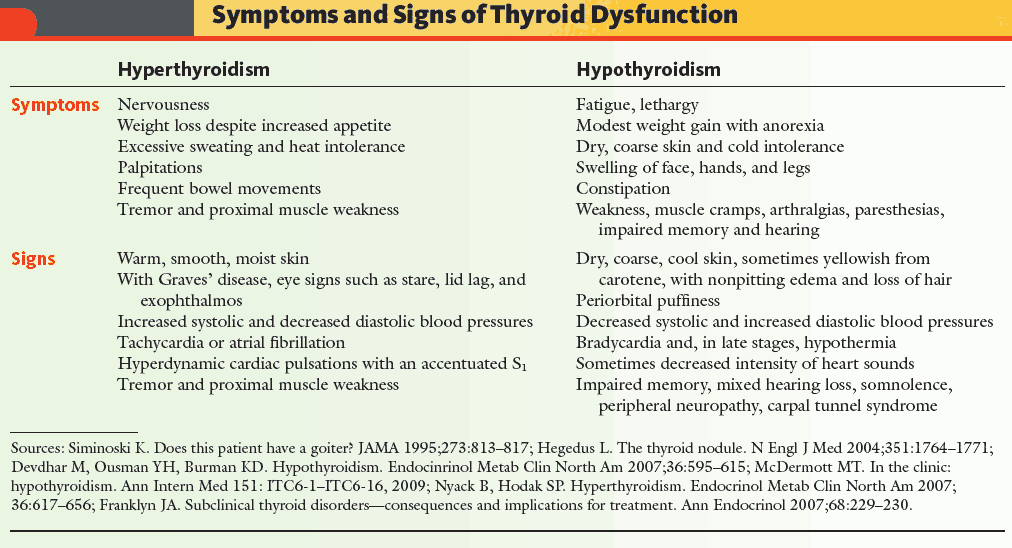
Clinical Presentation of Hypothyroidism
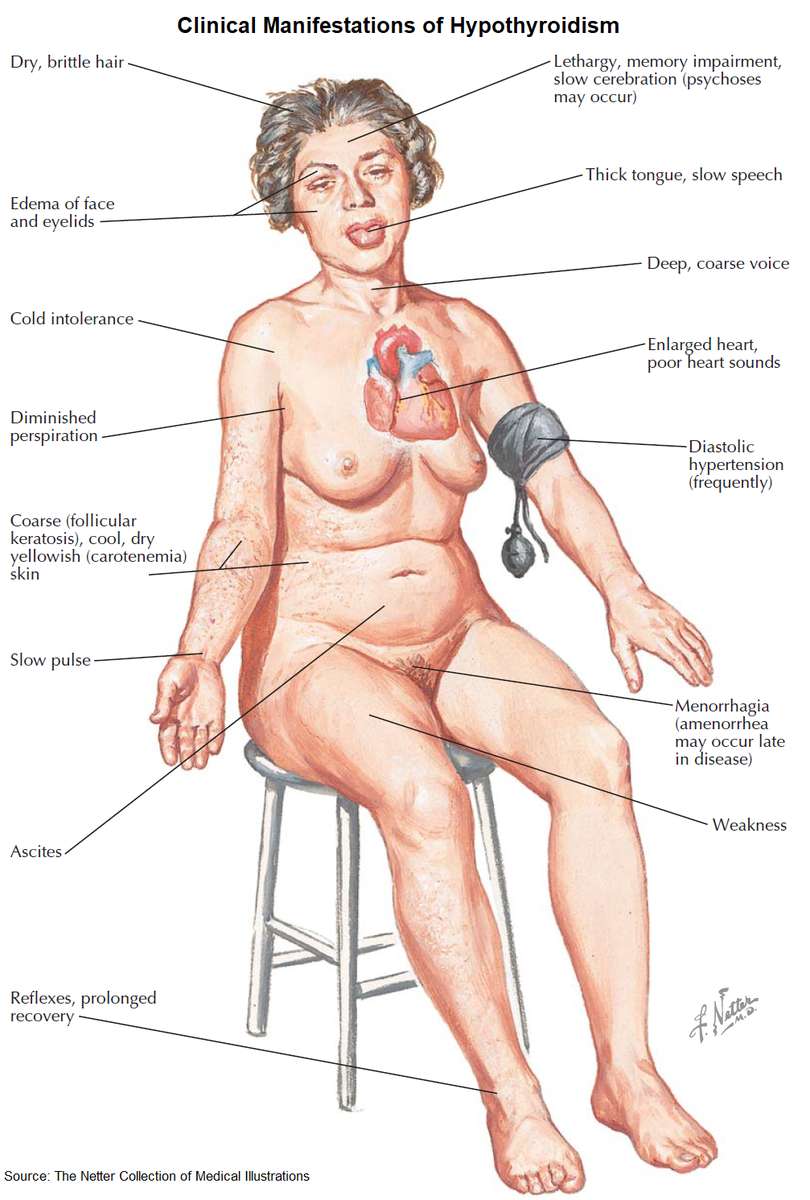
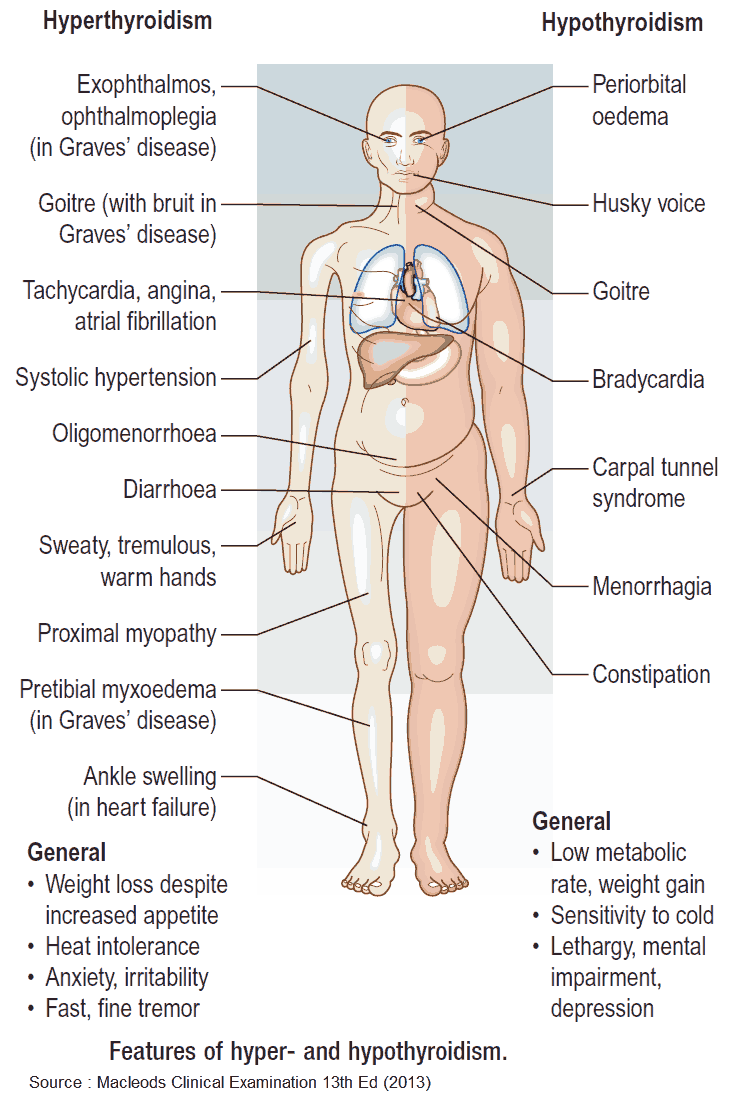
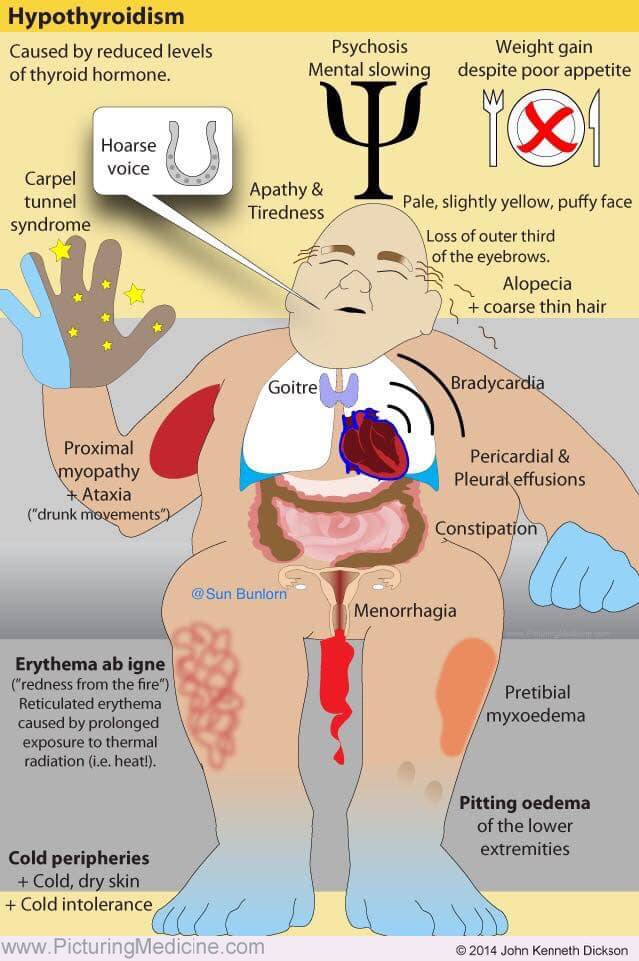
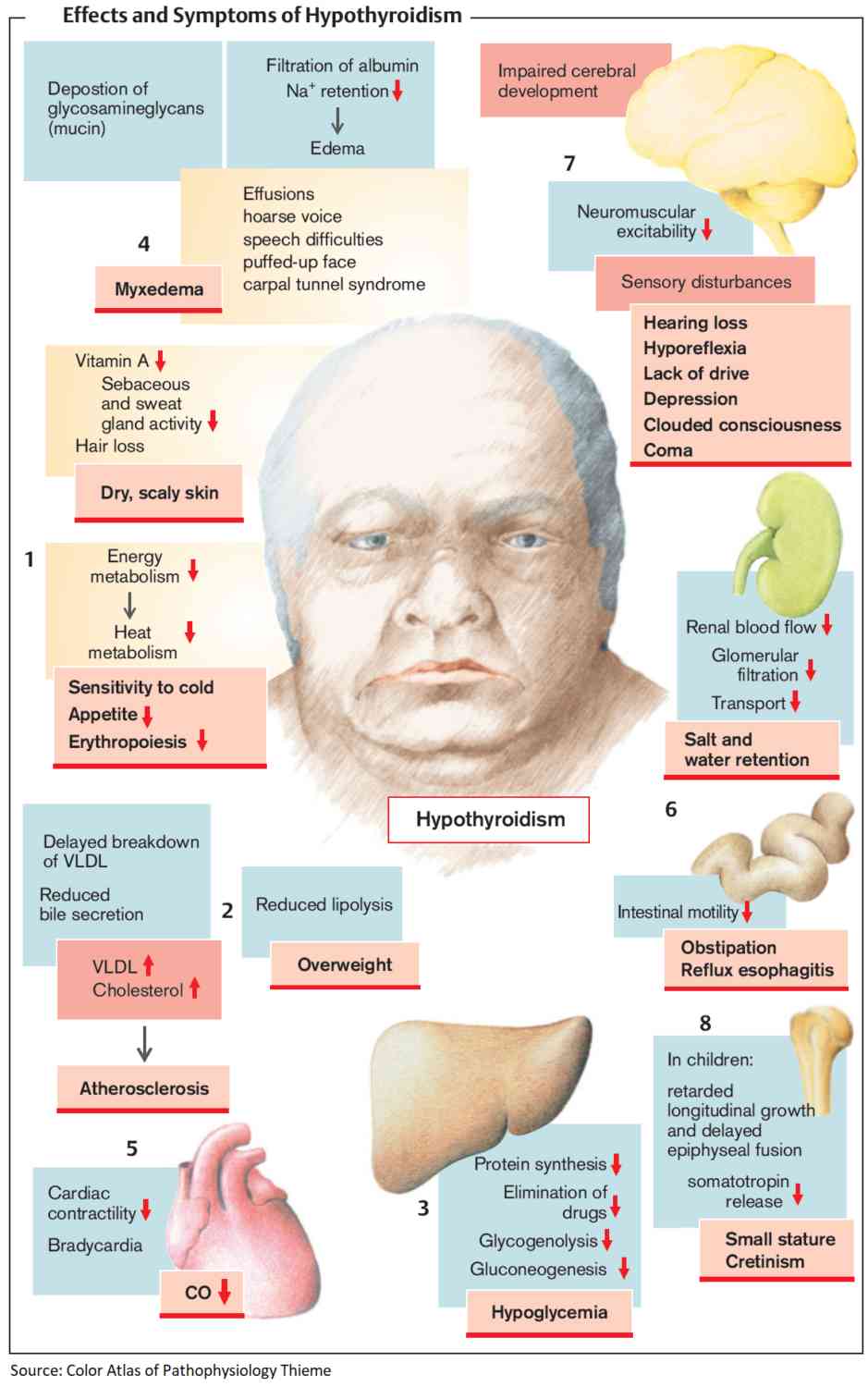
The onset is insidious and the symptoms often nonspecific and vague. Common presenting symptoms include tiredness, lethargy, weight gain, cold intolerance, hoarseness, and dryness of the skin. However, virtually any organ system can be affected.
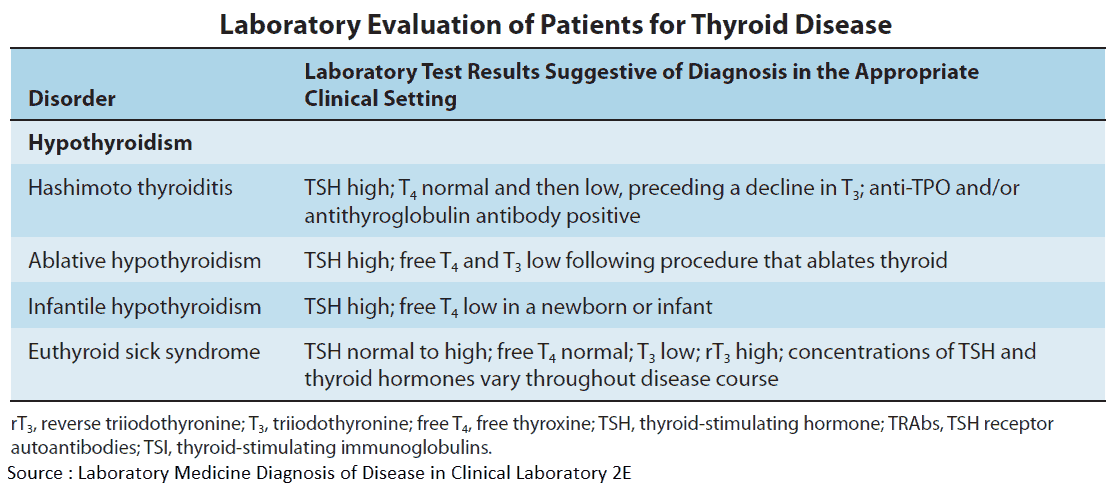
Hypothyroidism: Investigations and Diagnosis
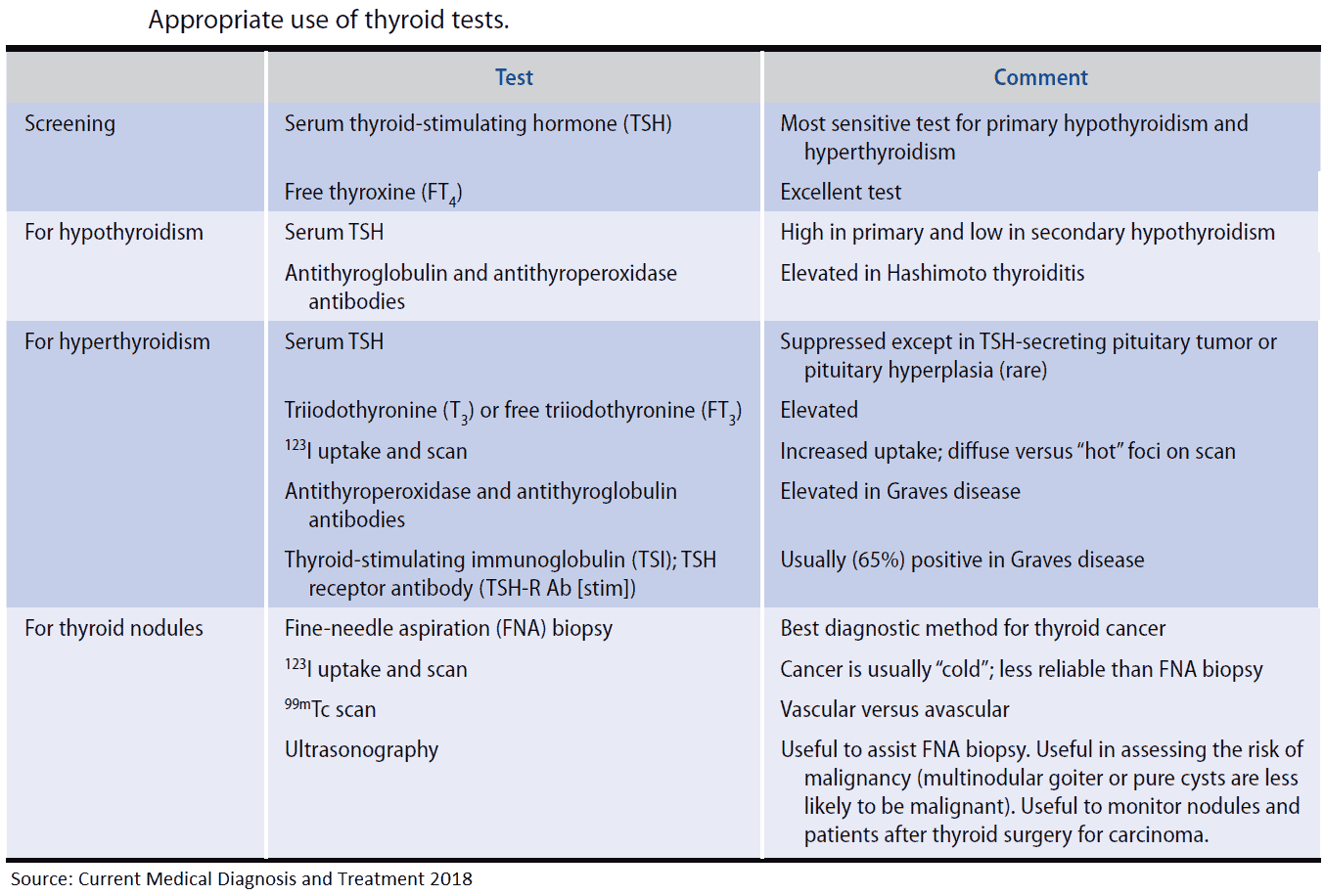
The following investigations are important in patients with hypothyroidism:
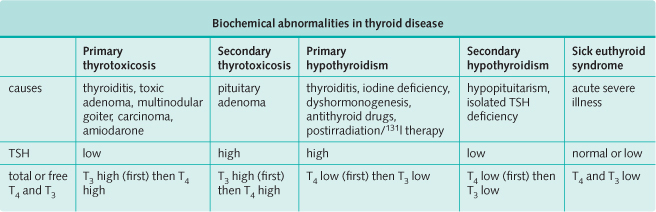
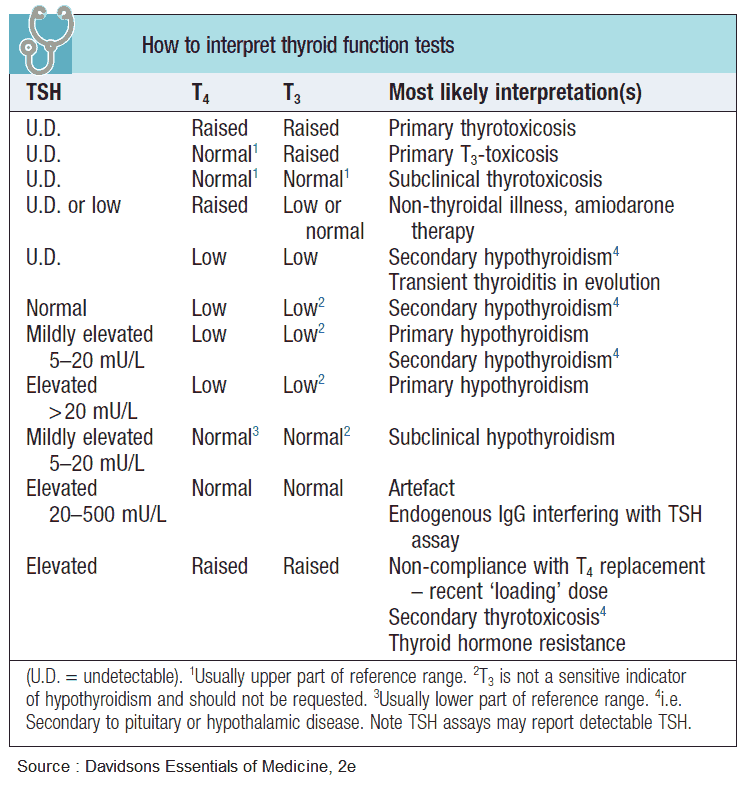
- Free or total T4 are reduced, and serum TSH is high.
- T4 may be normal with a high serum TSH. This indicates subclinical hypothyroidism.
- If secondary hypothyroidism is suspected, the free and total T4 are reduced and the TSH is also low. This picture is also obtained in sick people without thyroid disease, and patients on steroids and anticonvulsants.
- Antibodies to thyroglobulin or thyroid peroxidase (microsomal antibodies): typically strongly positive in Hashimoto’s thyroiditis.
- Cholesterol: raised.
- CBC: anemia and raised mean corpuscular volume.
- ECG: sinus bradycardia, low voltage complexes.
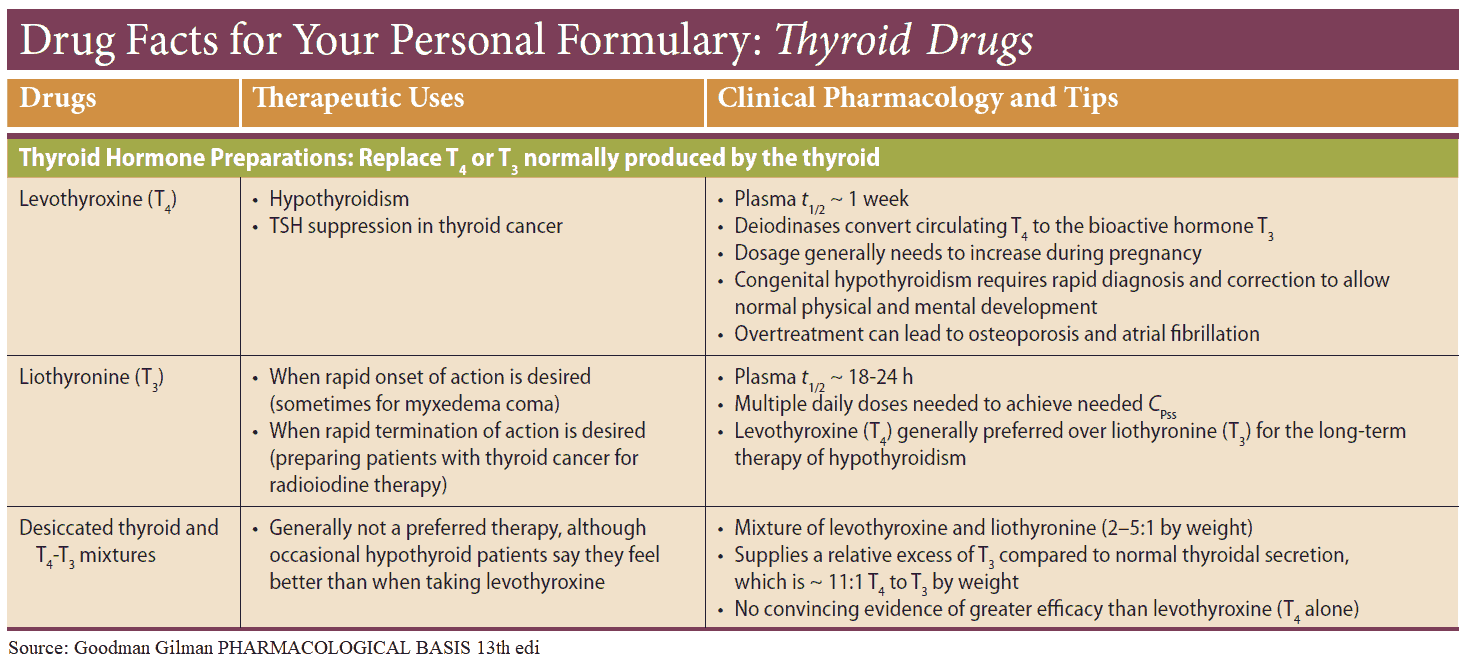
Treatment of Hypothyroidism
Thyroxine sodium is the treatment of choice for maintenance therapy. Usual maintenance doses are between 100-200 μg daily. The initial dose is usually 50 μg, increased as necessary over a few weeks, and even lower doses (25 μg) are started in elderly patients or patients with cardiac disease to avoid worsening angina or precipitating a myocardial infarction. Treatment is monitored by serum TSH and serum T4 and is nearly always lifelong, except in cases of subacute or silent thyroiditis.
Myxedema coma
This is uncommon. It is typically seen in the elderly and precipitated by infection, treatment with sedatives, or inadequate heating in cold weather. Most patients have hypothermia and are hypotensive with heart failure, hyponatremia, hypoxia, and hypercapnia.
Treatment is with T3 intravenously because of its rapid action. Supportive measures are also needed including intravenous fluids, antibiotics, ventilation, and slow rewarming. T4 can be substituted after 2-3 days if there is a clinical improvement.