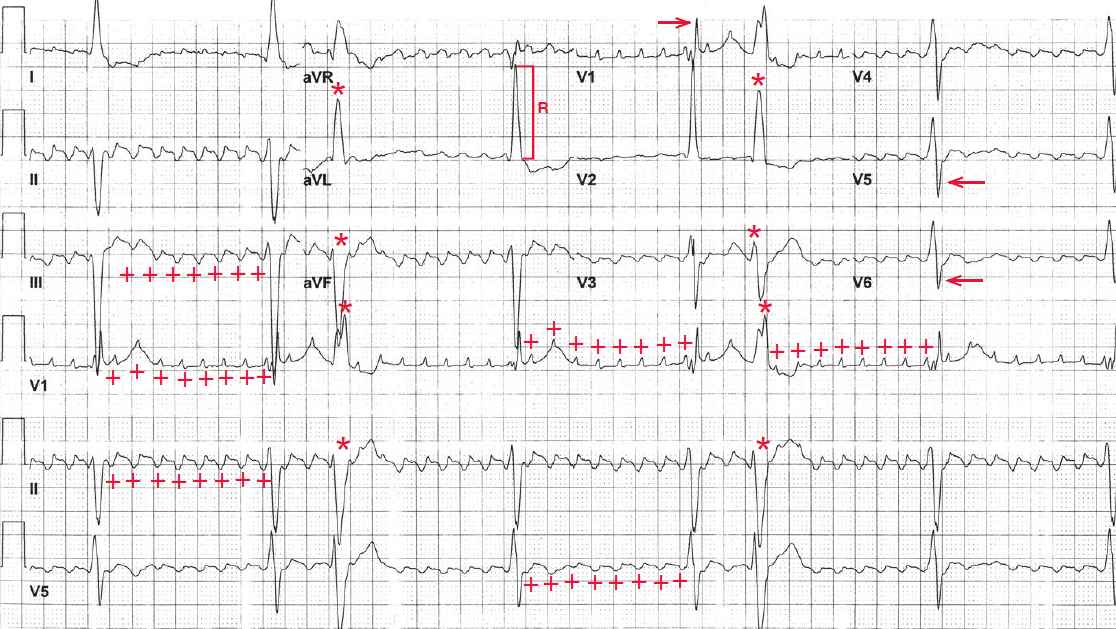
The rhythm is basically regular, but there are two premature complexes (third and sixth) (*) that are wide and abnormal with a morphology that differs from the others. These are premature ventricular complexes.
All the other RR intervals are identical. Hence this is a regularly irregular rhythm at a rate of 38 bpm. Because there is a high degree of AV block (8:1), prominent flutter waves (+) can be seen at a regular rate of 300 bpm.
The flutter waves are uniform in morphology, amplitude, and interval and have a typical undulating (saw-tooth) pattern. There is no isoelectric baseline between each flutter wave.
The important characteristics of atrial flutter are a regular atrial rate of greater than 260 bpm with uniformity of all the waveforms and a consistent undulation of the waveforms without an isoelectric baseline between them. This is because atrial flutter is the result of a single reentrant circuit (in the right atrium) and consistent and continuous electrical activity is generated as a result.
The QRS complexes are wide (0.16 sec) and have a right bundle branch block morphology (RSR′ in lead V1 [→] and broad S wave in leads V5-V6 [←]). The axis is extremely leftward, between –30° and –90° (positive QRS complex in lead I and negative QRS complex in leads II and aVF).
There are two etiologies for an extreme left axis,ie, an old inferior wall myocardial infarction with initial deep Q waves in leads II and aVF or a left anterior fascicular block in which there is an rS morphology of the QRS complex in leads II and aVF. Hence, this is a left anterior fascicular block. This conduction abnormality (ie, right bundle branch block and left anterior fascicular block) is termed bifascicular block.
The R-wave amplitude in lead aVL is 20 mm ( ] ), meeting criteria for left ventricular hypertrophy (ie, R-wave amplitude in lead aVL > 18 mm in the presence of a left axis). The QT/QTc intervals are normal (600/480 msec and 540/420 msec when corrected for the prolonged QRS complex).
The patient has evidence of significant conduction system disease with high-degree AV block as well as bifascicular block. The conduction system disease is likely the result of the underlying cardiomyopathy. The presence of advanced conduction abnormalities suggests complete heart block as a cause of syncope.
The treatment of choice for complete heart block and symptomatic bradycardia is placement of a pacemaker. However, another cause for syncope in patients with hypertrophic cardiomyopathy is ventricular tachyarrhythmia. Hence the etiology for the syncope should be further evaluated and established before pursuing a specific therapy.
- READ MORE:
- SIMILAR CASES: