This article is an answer to the ECG Case 160
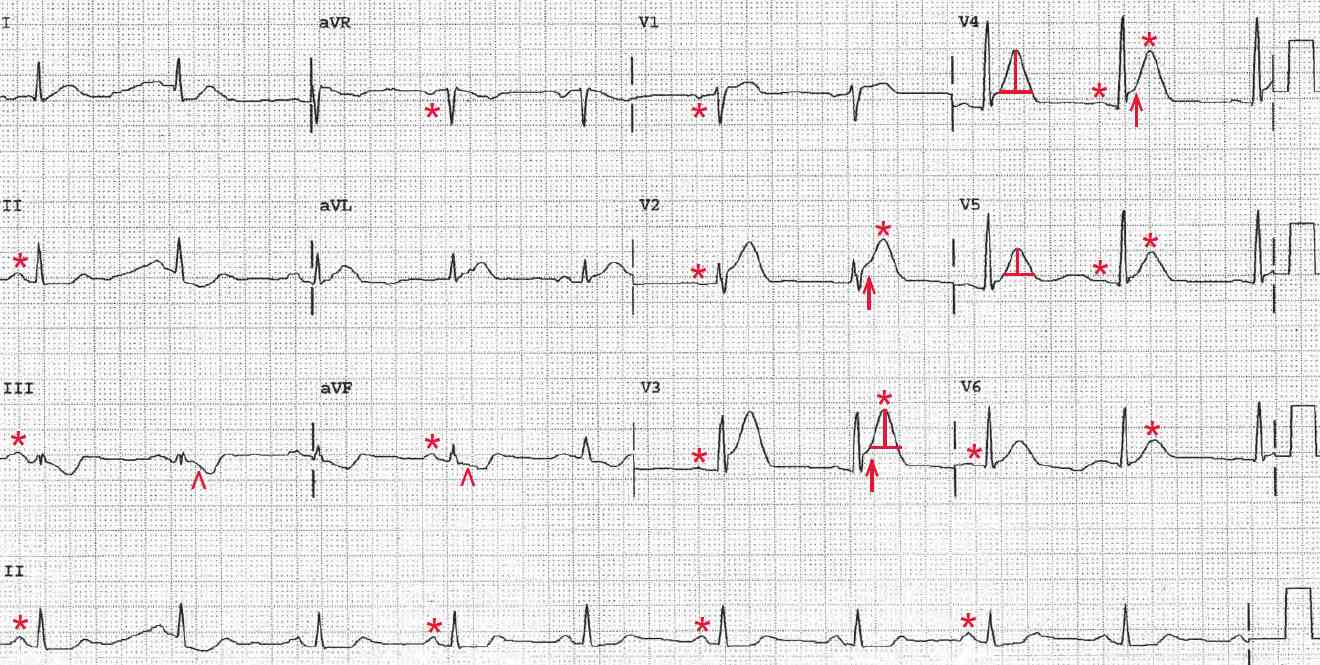
There is a regular rhythm at a rate of 56 bpm. There is a P wave (*) before each QRS complex, with a stable PR interval (0.20 sec). The P wave is upright in leads I, II, aVF, and V4-V6 and negative in lead aVR. The P-wave morphology is normal. This is a normal sinus bradycardia.
There are tall and symmetric T waves (+) in leads V2-V6. The normal T wave is asymmetric (ie, the upstroke is slower than the downstroke). T waves that are tall, peaked and, most importantly, symmetric (hyperacute) are seen with hyperkalemia.
Hyperkalemia may be systemic or localized, as is seen in acute transmural myocardial infarction (MI). Hyperacute T waves are the first abnormality noted in an acute transmural MI and are due to localized hyperkalemia. They occur in the area of myocardium involved and are seen even before there are any ST-segment changes.
Also noted is ST-segment elevation (↑) in leads V2-V4, and the ST segments are convex. Hence this is an early acute anteroapical ST-segment elevation MI (STEMI).
In addition, ST-segment depressions (^) are noted in leads III and aVF; these are reciprocal ST-segment changes that are due to the same ST-segment changes viewed from another angle or direction.
This patient is having acute transmural myocardial ischemia and possibly an acute anterior wall MI, likely resulting from his recent cocaine use. If the T-wave and ST-segment abnormalities resolve with nitrate therapy, the cause is most likely spasm. Persistent changes would suggest an acute transmural MI.
Non-ischemic chest pain is common in patients who use intranasal cocaine, so differentiating myocardial ischemia from noncardiac chest pain can be challenging. Cocaine can cause ischemic chest discomfort by inducing vasospasm and increasing myocardial oxygen demand by increasing heart rate, blood pressure, and inotropy.
Although uncommon, cocaine can provoke an acute MI by spasm associated with thrombus formation due to increasing thrombogenicity as a result of enhanced platelet activation and aggregation. Chronic use is associated with hypertension, left ventricular hypertrophy, cardiomyopathy, myocarditis, and occasionally aortic dissection and stroke.
Chronic cocaine use can also result in accelerated atherosclerosis as a result of endothelial dysfunction. Therefore, it is also possible that the infarction is the result of an acute plaque rupture, induced by cocaine and vasospasm. This would occur if the spasm occurs in the area of an atherosclerotic plaque, with resultant plaque disruption, setting up the usual mechanism for thrombus formation and a typical MI.