This post is an answer to the ECG Case 209
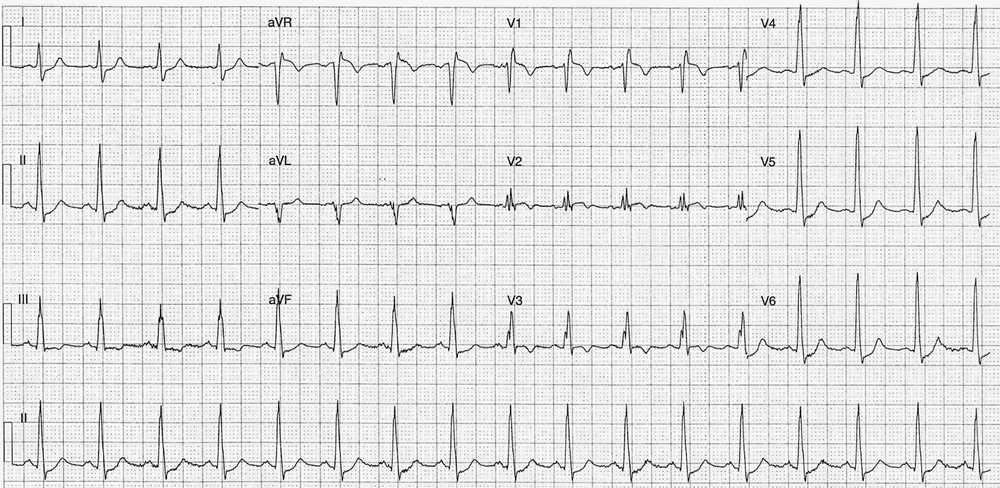
- Rate: 102 bpm
- Rhythm:
- Regular
- Sinus Rhythm
- Axis:
- Normal (~80 deg)
- Intervals:
- PR – Normal (~160ms)
- QRS – Prolonged (100-120ms)
- QT – 320ms (QTc Bazette ~410 ms)
- Segments:
- ST Elevation in leads aVR (1.5mm) V1 (1mm) V2 (subtle)
- ST Depression in Leads I, II, III, V4, V5, V6
- Additional:
- T wave inversion leads III, aVR, V1, V2, V3
- S wave lead I
- Small Q waves (<1mm) leads II, III, aVF
- RSR’ pattern V1, V2
- Partial / Complete RBBB – QRS varies 100-120ms
Interpretation
The ECG findings really suggest two likely pathologies, Pulmonary Embolism or ACS. With this clinical stem of hypoxia, hypotension, tachycardia and pre-syncope PE is more likely than ACS .
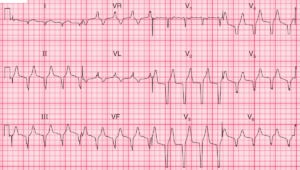
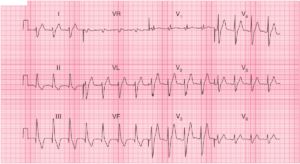
The presence of T wave inversion in lead V1 plus lead III, as in our case here, was only seen in 1% of ACS patients versus 88% of patients with Acute Pulmonary Embolism (n=87 in ACS group, n=40 in PE group) according to Kosuge et al. paper here.
The ECG in Pulmonary Embolism ultimately lacks sensitivity and specificity. Its most important role is the detection of another cause for the patients symptoms e.g. ACS or STEMI.
Some ECG features that are associated with PE are:
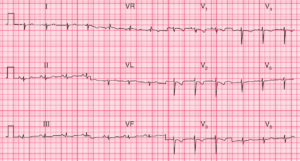
- Normal ECG in 9-26% of cases
- Sinus Tachycardia in 44-73% of cases
- RBBB (Complete or incomplete) in 18-25% of cases
- RAD in 16-23% of cases
- P Pulmonale in 9-33% of cases
- Supraventricular arrhythmia in 8-33% of cases
- Clockwise rotation in 18-30% of cases
- T inversion Right Precordial leads in 10-46% of cases
- S1Q3T3 in 12-25% of cases
- S1Q3T3 whilst oft quoted as ‘the’ ECG finding in PE lacks sensitivity, specificity, and is certainly not pathognomonic of PE.
What happened next ?
Formal CTPA report: Saddle pulmonary embolism is noted. Heavy bilateral thrombus burden. There is CT evidence for right heart strain.
The patient was then transferred to a Tertiary Center and underwent a successful pulmonary embolectomy and was discharged from hospital within a week.
READ MORE: Pulmonary Thromboembolism and Thrombolytics
SIMILAR CASES: