This post is an answer to the Case – Sudden Unconsciousness and Hemiparesis
What is seen on the CT ?
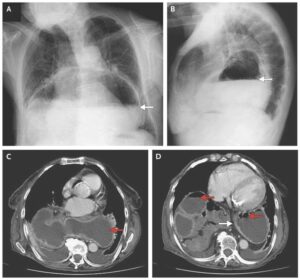
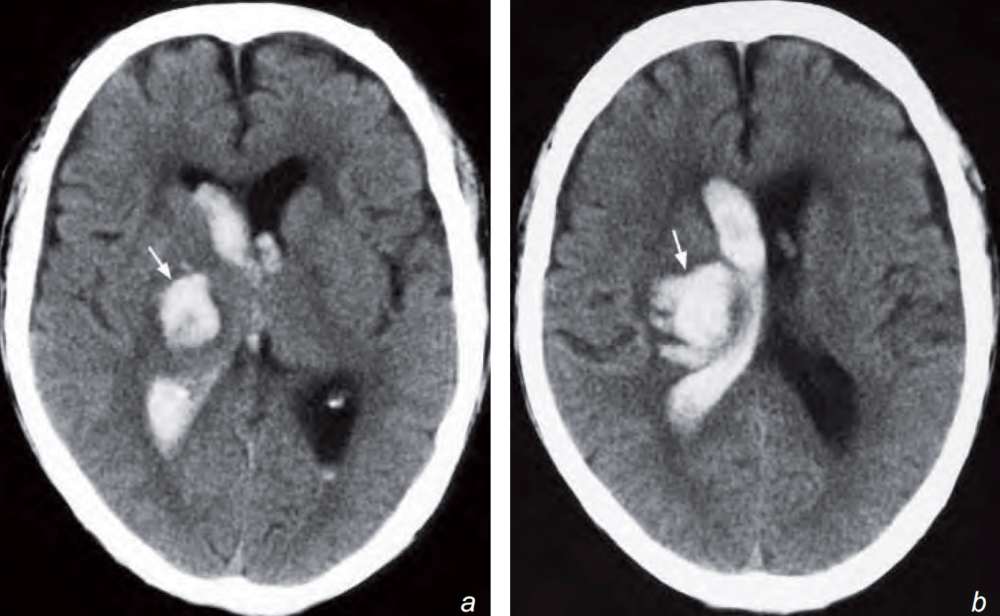
There is an acute intraparenchymal haematoma in the right thalamus and lentiform nucleus with intraventricular extension into the lateral ventricles.
What is the diagnosis ?
Non-contrast axial CT scan showing a right thalamic and lentiform nucleus haemorrhage (arrow) with extension of blood into the lateral ventricle. The location is typical for a hypertensive haemorrhage.
Discussion
Note that both infarcts and haemorrhage cause stroke and their clinical presentation may be very similar. A CT scan is indicated to differentiate the two as the treatment options are very different. Anticoagulation/thrombolytic treatment is contraindicated in patients with intracranial haemorrhage.
Common causes of intraparenchymal haemorrhage:
- Hypertensive haemorrhage:
- a. Typical location: basal ganglia, brainstem, cerebellum
- Variable secondary intraventricular and subarachnoid extension
- May cause hydrocephalus or brain herniation due to its mass effect
- Often not associated with much surrounding oedema.
- Ruptured/leaking aneurysm
- Bleeding from an ateriovenous malformation (AVM)
- Trauma
- Intra-tumoural or peritumoural haemorrhage. Haemorrhagic tumours:
- Glioblastoma multiforme (GBM)
- Anaplastic astrocytoma
- Oligodendroglioma
- Ependymoma
- Primitive neuroectodermal tumours (PNETs)
- Pituitary adenoma
- Metastases Contrast
- CT may show enhancement of the nonhaemorrhagic component in tumour haemorrhage. The presence of persistent white matter oedema around the haemorrhage may suggest that the haemorrhage is probably within an underlying tumour and further imaging with contrast enhanced CT or MRI is necessary.
- Haemorrhagic infarct
- Coagulation disorder
Venous haemorrhage:
This may be due to thrombosis of the intracranial venous sinuses/ veins which results in increased back-pressure and therefore haemorrhage and/or cerebral oedema. Common causes of venous sinus thrombosis include:
- Idiopathic
- Adjacent septic focus, e.g. mastoiditis
- Trauma
- Tumour compressing or invading into adjacent sinus
- Hypercoagulability, e.g. oral contraceptives, pregnancy, antiphospholipid syndrome
The superior sagittal sinus is most commonly involved. Others include transverse, sigmoid and straight sinuses. Non-contrast axial CT scan shows unilateral or bilateral parenchymal haemorrhage which is typically close to a venous sinus. CT scan may show a thrombus or a contrast filling defect in the adjacent sinus (termed the ‘delta sign’ for the superior sagittal sinus) with/without outward bowing of sinus wall.
The venous phase of a cerebral angiogram is currently the gold standard for diagnosing venous sinus thrombosis but it is an invasive procedure. Multi-detector CT venography shows promising potential.
MR venogram offers a radiationfree alternative. The technique relies on a loss of fl ow-related signal within the venous sinus for diagnosis or the presence of a filling defect.
READ MORE: Stroke and TIA: From Diagnosis to Treatment