Table of Contents
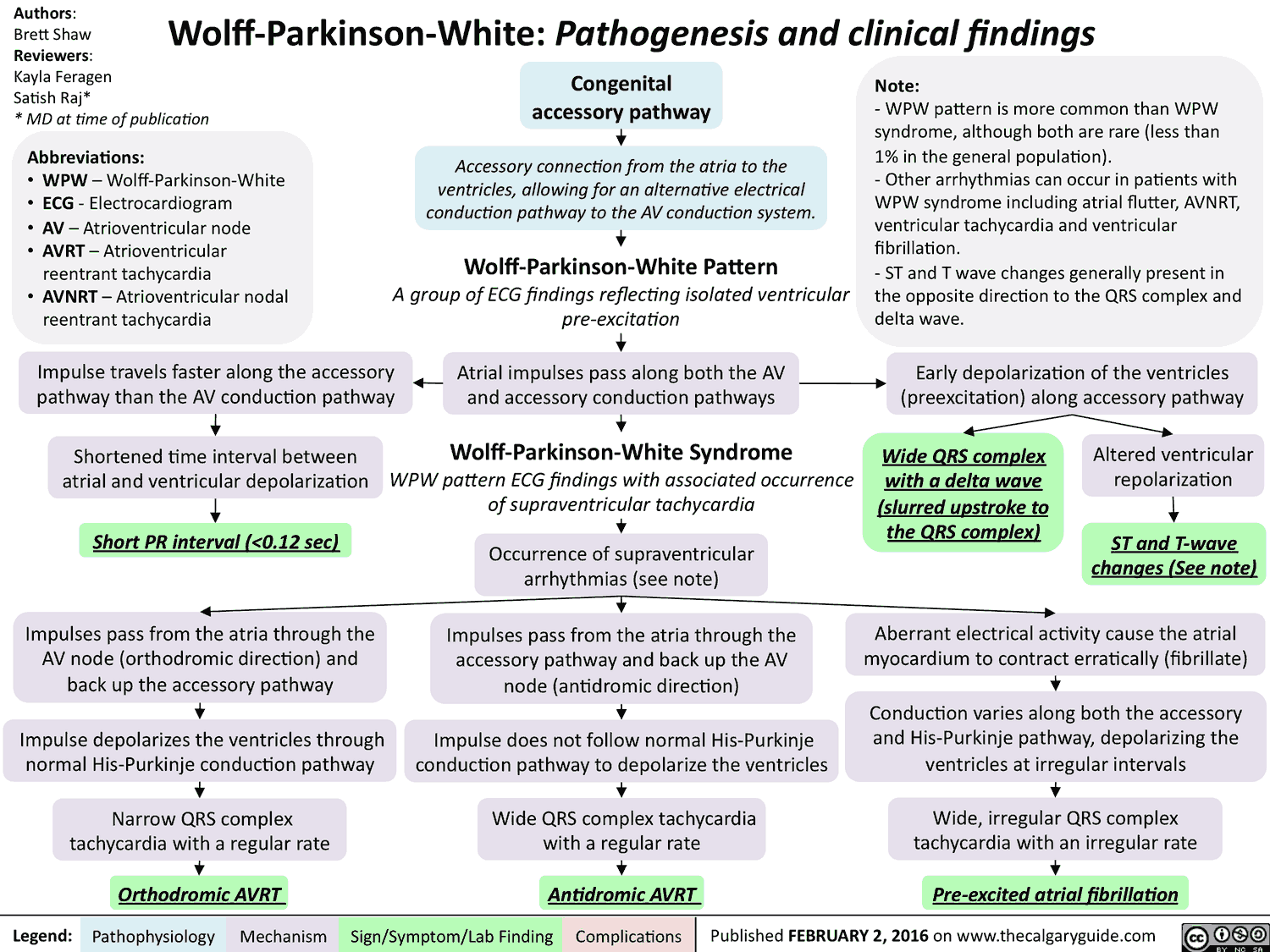
In 1930, Wolff, Parkinson, and White described the combination of bundlebranch block, shortened PR interval, and recurrent episodes of tachycardia that occurred in young, healthy patients with structurally normal hearts.
This combination of electrocardiographic (ECG) findings described the ventricular pre-excitation syndrome known as the Wolff-Parkinson-White (WPW) syndrome.
In WPW, an accessory pathway connects the atrial tissue to the ventricular myocardium. This connection bypasses the atrioventricular (AV) node and creates a direct electrical connection between the atria and ventricles.
Patients with WPW can experience a range of tachydysrhythmias, which can lead to disabling symptoms, cardiovascular collapse, and death in select cases.
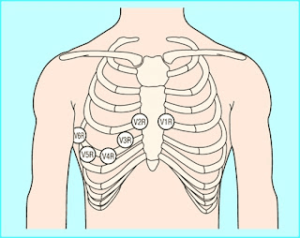
ECG features of Wolff-Parkinson-White (WPW)
The three hallmark ECG features of WPW include:
- PR interval <0.12 seconds
- Delta wave (initial slurring of the QRS complex)
- Wide QRS complex (width >0.10 seconds)
Pathophysiology of Wolff-Parkinson-White (WPW)
The PR interval is short because the impulse that progresses down the accessory pathway arrives earlier than anticipated to the ventricle. This portion of the impulse is not subjected to the physiologic slowing that occurs in the AV node.
The delta wave represents activation of a portion of the ventricle through the accessory pathway.
Simultaneously, there is the impulse that travels through the normal pathway into the AV node and innervates the remainder of the ventricle. This is represented by the middle and terminal segments of the QRS complex.
Ultimately, the ventricle is activated by two distinct pathways and results in a wide QRS complex that is a fusion of the two impulses.
Importantly, only a portion of patients with the classic ECG triad of WPW are diagnosed with the syndrome. Patients must have symptoms consistent with a tachydysrhythmia (i.e., palpitations, syncope) to be diagnosed with WPW syndrome.
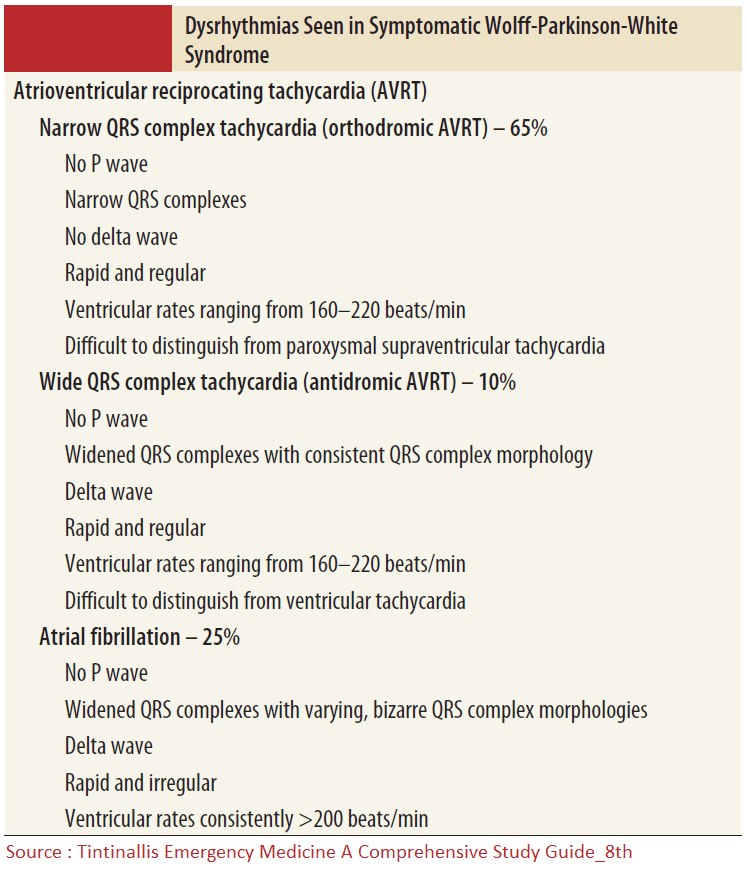
Tachydysrhythmias Seen in WPW
The most common tachydysrhythmias seen in WPW patients include:
- Narrow complex atrioventricular reciprocating tachycardia (Orthodromic AVRT)
- Atrial fibrillation
- Wide-complex Tachycardia (Antidromic AVRT)
Atrial fibrillation can be seen in up to 25% of patients with WPW syndrome. In atrial fibrillation, the multiple foci of atrial impulses can be transmitted through the accessory pathway and result in an uncontrolled ventricular rate.
When these uncontrolled ventricular depolarizations occur along with those that arrive via the AV node, patients can experience rapid ventricular rates and cardiovascular collapse.
ECG features of WPW with Atrial Fibrillation
In patients with WPW syndrome who experience atrial fibrillation, the ECG demonstrates several unique features that include:
- Very rapid, irregularly irregular rhythm
- Wide QRS complex
- Significant beat-to-beat variation in QRS complex morphologies
- A delta wave can also be seen in these patients.
Management of WPW-related Atrial Fibrillation
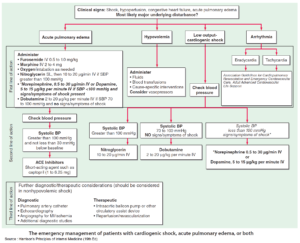
The management of WPW-related atrial fibrillation is largely based on the hemodynamic status of the patient.
- In the hemodynamically unstable patient, cardioversion with sedation is the treatment of choice.
- In the stable patient, rate control with medications can be attempted, though cardioversion and other resuscitation interventions should be immediately available.
Once the patient is stabilized and the rhythm converted to sinus rhythm, admission to a monitored critical care bed is most appropriate. Cardiology consultation should also be obtained.
Read More about Management of Atrial Fibrillation (AF) with Rapid Ventricular Response (RVR)
Procainamide
Procainamide is the primary agent for control of WPW-related atrial fibrillation in the stable patient. Procainamide is dosed at 20 to 30 mg/minute, until the dysrhythmia is terminated or one of the following end points is reached:
- development of hypotension
- the QRS complex widens by 50% or more from its original width
- acceleration of the tachycardia
- a total of 1 g is administered
Patients who are treated with procainamide should be placed on continuous cardiac monitor and have frequent assessments of blood pressure.
Regardless of the administration strategy, procainamide has a relatively slow onset of action and may not reach therapeutic blood levels for 40 to 60 minutes.
Amiodarone
Amiodarone should be avoided in the treatment of patients with WPW related atrial fibrillation. Amiodarone was previously recommended as an appropriate agent in this setting.
However, its diverse electrophysiologic effects (i.e., beta-adrenergic, calcium channel, fast sodium channel blocking mechanisms) impact the accessory pathway and make rapid intravenous administration dangerous.
Amiodarone can accelerate the ventricular rate and result in ventricular fibrillation or cardiovascular collapse.
AV Blocking Medications
Medications that block the AV node are contraindicated in the treatment of patients with WPW and atrial fibrillation. Calcium channel antagonists, beta-adrenergic blocking agents, adenosine, and digoxin can enhance conduction via the accessory pathway, and lead to rapid ventricular rates, malignant ventricular dysrhythmias, and cardiovascular collapse.
Atrial fibrillation occurring in the setting of the WPW syndrome should be included in the differential diagnosis of patients with a wide-complex tachycardia.
Clinical clues to the diagnosis include a young patient who presents with a very rapid, irregularly irregular rhythm that has significant beat-to-beat variation in the QRS complex morphology.
Key Points
- The classic ECG triad of WPW includes a short PR interval, delta wave, and a widened QRS complex.
- Atrial fibrillation can occur in up to 25% of patients with WPW syndrome.
- Cardioversion is the treatment of choice for unstable patients with WPW-related atrial fibrillation.
- Procainamide is the primary medication for control of WPW-related atrial fibrillation in the stable patient.
- All medications that block the AV node should be avoided in the treatment of patients with WPW-related atrial fibrillation.
Suggested Readings
- Brady WJ. Wolff-Parkinson-White syndrome. In Brady WJ, et al. eds. The ECG in Prehospital Emergency Care. London: Wiley, 2012.
- Wolff L, Parkinson J, White PD. Bundle-branch block with short PR interval in healthy young people prone to paroxysmal tachycardia. Am Heart J. 1930;5:685–704. https://pubmed.ncbi.nlm.nih.gov/17040283/

![Read more about the article Left Ventricular Hypertrophy (LVH): How to Recognize it on ECG [With Examples]](https://manualofmedicine.com/wp-content/uploads/2025/12/Summary-of-the-various-diagnostic-ECG-criteria-for-left-ventricular-hypertrophy-LVH.png)